Intensive Care Medicine
QUESTIONS
Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation. Please answer True or False:
- Risk factors for neonatal sepsis include:
a. Male sex
b. Pre-term birth
c. Maternal Group B Streptococcus colonisation
d. Premature rupture of membranes
e. Caesarian section - Regarding the initial management of neonatal collapse:
a. An initial fluid challenge of 20ml/kg of crystalloid is appropriate
b. The usual dose range for dinoprostone is 50 -100ng/kg/min
c. Cefotaxime is an appropriate first line antibiotic therapy
d. Intra-osseous access should only be used as a last resort
e. Dobutamine is the most appropriate first-line inotrope - Regarding congenital heart disease (CHD):
a. CHD presenting in the neonatal period is usually ‘duct dependent’
b. Functional closure of the Ductus Arteriosus can be reversed by administering prostacyclin
c. Response to dinoprostone is usually seen within 15 minutes
d. High flow oxygen should be administered in all cases of suspected CHD
e. Neonatal tachyarrhythmias should be suspected when the heart rate is greater than 160bpm
Key Points
- Antibiotics should be administered within 1 hour of any suspected case of severe neonatal infection and not delayed for confirmation of diagnosis
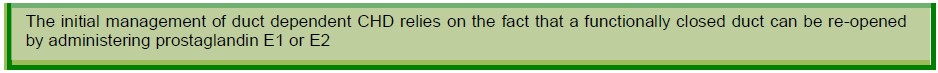
- When congenital heart disease is suspected a prostaglandin infusion should be started, with the aim of reversing functional closure of the ductus arteriosus
- Non accidental injury can be difficult to recognise and requires a high index of suspicion
- Investigation to rule out inborn errors of metabolis
INTRODUCTION
This is the second article of a two article series on the practical management of the collapsed neonate. The first article (Anaesthesia tutorial of the week number 355) covers the initial assessment and initial management of a collapsed neonate. This article expands on the specific management of each of the four most common conditions responsible for causing neonatal collapse. This article is not intended to be an authoritative text on this important subject but we hope that it will be a useful resource for those of us who do not regularly face this scenario. References for some of the excellent, more detailed educational material are provided. The appendix of the previous article includes a list of medical equipment that should be readily available in all departments that are responsible for caring for this patient group.
There are four main causes of neonatal collapse; congenital heart disease, infections, in-born errors of metabolism and non-accidental injury. Often initially the exact cause is not clear. Consequently, an extremely important principle is that collapsed neonates should be managed as if they have any one of these four conditions. As previously emphasised, the management of these babies is complex; it requires the rapid assembly of the most experienced team possible. Whilst some specialist techniques, such as neonatal echocardiography, can be extremely helpful, they are not universally available. If congenital heart disease is suspected, appropriate treatments, including an infusion of dinoprostone, should be commenced as soon as possible, and specialist help should be urgently sought. Each of the 4 main conditions will be discussed in turn.
NEONATAL SEPSIS
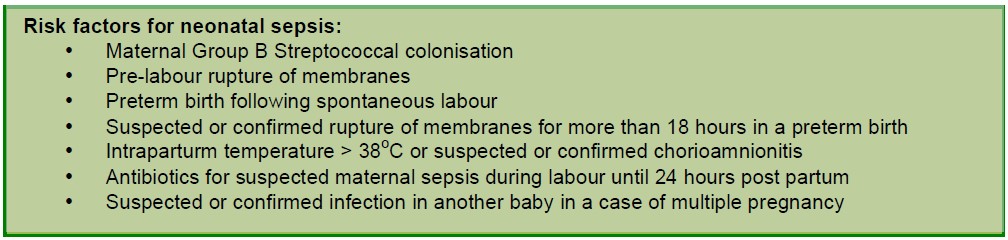
Neonatal sepsis can often be difficult to diagnose. Therefore all neonates who present acutely unwell should be treated as if they have a serious underlying infection until proven otherwise. Preceding symptoms can either be absent altogether or very vague. Examples of the latter include: altered behaviour, a change in muscle tone, difficulty with feeds and a change in skin colour. More clear clinical indicators of sepsis are a temperature <36°C or >38°C, local signs of infection, evidence of shock, oliguria, metabolic acidosis and coagulopathy. Some of the many risk factors for neonatal sepsis are listed below.
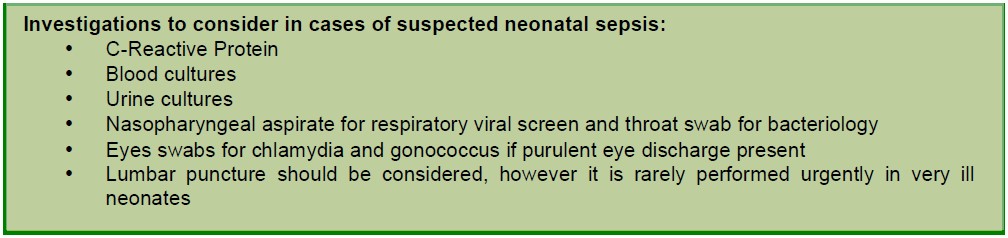
In suspected or possible severe neonatal infections antibiotics should be administered as soon as possible and certainly within 1 hour of the decision that they are indicated. Evidence in adults suggests that there is a linear relationship between duration of delay in administration of appropriate antibiotic therapy in patients with sepsis induced hypotension and increased mortality1. In cases of suspected neonatal sepsis, antibiotic administration must not be delayed for confirmation of the diagnosis. It is much safer to give antibiotics and then stop them at a later date if cultures remain negative and there is no confirmatory evidence. When possible it is clearly very important to obtain appropriate cultures prior to antibiotic administration but this should not include waiting to perform a lumbar puncture.
Current NICE guidelines suggest an initial empirical regimen of benzylpenicillin 25mg/kg and gentamicin 5mg/kg unless microbiological surveillance data reveal local bacterial resistance patterns indicating different antibiotic choice2. In general, protocols from either your hospital or your tertiary receiving centre should be followed.
NEONATAL CONGENITAL HEART DISEASE
A collapsed neonate presenting to the emergency department is unlikely to have an obvious diagnosis of congenital heart disease (CHD). For this reason a high index of suspicion is vital and it is often necessary to treat the neonate as if they have a diagnosis of CHD until proven otherwise. Duct dependent lesions tend to present within the first 2 weeks of life. For this reason, measuring both pre- and post-ductal blood pressures and oxygen saturations should be routinely assessed in any unwell neonate. Non-duct dependent lesions may present at any time, including the first 2 weeks of life. A basic understanding of some of the changes in the foetal circulation around birth is required for successful management.
The ductus arteriosus (DA) is a conduit between the pulmonary artery and the descending aorta that allows blood to bypass the lungs in utero. Closure of the DA is a two-stage process. Functional closure of the duct usually occurs within 15 hours of delivery. Functional closure is precipitated by a marked drop in pulmonary vascular resistance, which in turn is caused by both increasing oxygen levels and a decrease in serum levels of maternal prostaglandins in neonatal blood. Anatomical closure usually follows within a few weeks of delivery.
Functional closure of the DA can unmask CHD in one of three ways:
- By interrupting blood supply to the systemic circulation – seen in left-sided obstructive lesions
- By interrupting blood supply to the pulmonary circulation – seen in right-sided obstructive lesions
- By removing an important mixing point whereby blood from otherwise separate pulmonary and systemic circulations can mix – seen in transposition of the great vessels.
Left-sided obstructive lesions
Left-sided obstructive lesions that may present at the time of duct closure include coarctation of the aorta, critical aortic stenosis and hypoplastic left heart syndrome (HLHS). Typically these neonates present with shock, metabolic acidosis, pallor, mottling and absent or reduced peripheral pulses. Importantly these signs are not specific to CHD and once again the clinical presentation can be indistinguishable from other causes of neonatal collapse, such as sepsis or inborn errors of metabolism.
Coarctation of the aorta and critical aortic stenosis are conditions that most non-paediatric specialists are familiar with. It is also fairly easy to understand why restoring or improving the patency of the DA will improve systemic perfusion temporarily in these lesions, pending surgical correction.
Hypoplastic left heart syndrome (HLHS) is less well understood by non-specialists. HLHS describes mitral atresia with failure of development of both the left ventricle and first part of the aorta; a condition, which until around 30 years ago, was considered invariably fatal condition. As a result of these abnormalities, systemic circulation is reliant on a patent DA with early survival also being dependent on a non-restrictive ASD. Direction of blood flow across the DA and ASD will depend on the balance between pulmonary and systemic vascular resistance. This balance is important because too much pulmonary blood flow may cause a dangerous and potentially life-threatening decrease in systemic perfusion. High PaO2, low PaCO2 and high systemic vascular resistance will increase pulmonary blood flow. As a result, ventilation with high FiO2 levels may lead to low cardiac output and cardiac arrest. Therefore conservative targets are required for many physiological variables. Typically initial target oxygen saturations should be between 75-85% and blood gas targets for both PaO2 and PaCO2 should be around 7KPa. Unless the ventilator in use can provide a minimum fractional inspired oxygen concentration of 21% or less it is unlikely that the low PaO2 target will be met. Both mechanical ventilation and inotropic drugs are commonly required before urgent surgery.
Right-sided obstructive lesions
Right-sided obstructive lesions include critical pulmonary stenosis, pulmonary atresia, tricuspid atresia and Fallot’s tetralogy. The latter 2 conditions are causes of cyanotic CHD, although an asymptomatic acyanotic Fallot’s variant has been recognised. Most of the right-sided obstructive conditions will have a secondary mixing point, such as a ventricular septal defect (VSD) or atrial septal defect (ASD), which will allow cardiac output to be maintained to some extent despite duct closure. Neonates with right-sided obstructive conditions may present with cyanosis from birth or present at the time of duct closure with shock, metabolic acidosis and features of reduced lung perfusion on chest x-ray (CXR).
Transposition of the great vessels
Transposition of the great vessels is a condition with duct dependent mixing of pulmonary and systemic blood. Here the systemic and pulmonary circulations exist as two separate parallel circuits with three potential mixing points: a patent DA, a patent foramen ovale (PFO) and an ASD. Transposition usually presents with cyanosis at birth and as such, the majority of these neonates will present to the neonatal teams rather than adult intensive care or emergency medicine teams within non-specialist centres. However transposition can present late at the time of duct closure, hence its description here.
Neonatal tachyarrhythmias
Neonatal tachyarrhythmias are another group of cardiovascular causes of neonatal collapse. And should be suspected in any neonate with a heart rates of over 220 beats per minute. A 12 lead ECG is often required to identify the specific arrhythmia. Advice on further management should be sought from a paediatric cardiologist. If they are not immediately available then they should be supplied with faxed or scanned copies of the ECGs. A detailed description of these abnormalities and their specific management is beyond the scope of the article but the interested reader is directed towards an update on neonatal tachycardias: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2672672/.
Initial approach for suspected or proven CHD
In keeping with all cases of neonatal collapse, initial management of suspected or proven CHD should be delivered by a skilled team and involve rapid assessment of the adequacy of Airway, Breathing and Circulation. Whilst CHD should be suspected as an underlying cause in all cases of neonatal collapse the presence of cyanosis not responding to oxygen, poor or absent femoral pulses, a heart murmur, cardiomegaly or hepatomegaly should all further increase suspicion. An echocardiogram performed by a skilled operator will prove very useful but this should not delay initial stabilisation. Importantly stabilisation itself does not often rely on identification of a specific diagnosis.
Prostaglandins
Both prostaglandin E2 (dinoprostone) and prostaglandin E1 (alprostadil) can be administered via infusion to either prevent closure of the DA or reverse functional closure. Dinoprostone is the most commonly preferred therapy. If duct dependent CHD is suspected then an infusion should be immediately commenced. Usual starting doses of dinoprostone are 5 ng/kg/min if the neonate is well and up to 20 ng/kg/min if the neonate is unwell with absent femoral pulses. Doses in excess of 50 ng/kg/min have been used when there has been no response to lower doses and the neonate remains shocked, but in general, infusion rates higher than 30 ng/kg/min should be discussed with the retrieval or paediatric cardiology team. These drugs are potent vasodilators and systemic hypotension is a recognised side effect, particularly with increasing doses. Apnoeas are also a frequent side-effect and preparations should be made for intubation and mechanical ventilation if prostaglandin infusions are being used, particularly if dinoprostone infusion rates exceed 20ng/kg/min or if transfer to another hospital is being considered. Improvement is usually seen within 15 minutes of starting an infusion and an alternative diagnosis should be considered if response to treatment is poor.
Inotropes
Most critically unwell neonates will require inotropic support. It is often impractical to site central access in a non-sedated child, but an inotropic infusion should always either be available or running for all neonates who are due to undergo emergency induction of anaesthesia. Dopamine is the most common first line choice of inotrope. It has the advantage that it can safely be given, in a more dilute preparation, via a peripheral cannula. Alternatively, all inotropes can be administered via an IO needle. Initial starting rates of inotropes infusions are dependent on clinical state, but dopamine is commonly commenced at 5 mcg/kg/min and then up titrated as necessary.
NON-ACCIDENTAL INJURY
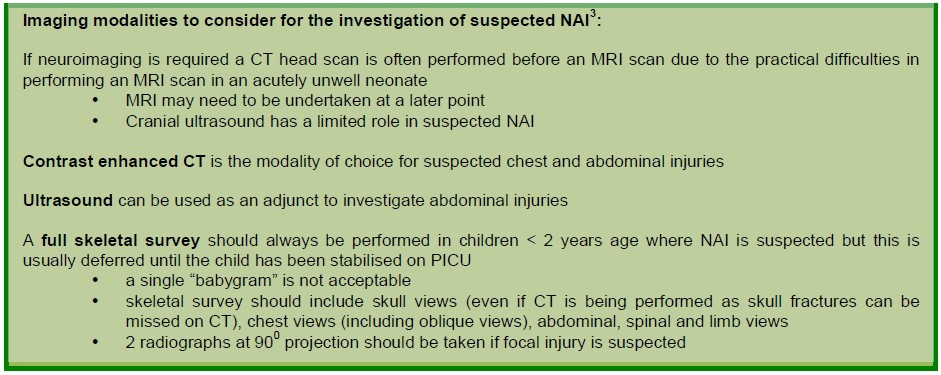
Sadly NAI remains the leading cause of death in the first year of life outside of the newborn period. Certain features may be suggestive of NAI such as delayed presentation, a history incompatible with the physical development of the child, a previous history of abuse, bite marks, cigarette burns and finger print bruising. However signs may be absent or vague and a high index of suspicion is required. As the history given by the parents may not be accurate, a detailed assessment is vital. As soon as the neonate has been stabilised a thorough examination of the child should be completed with full exposure. Fundoscopy and retinal photography by an ophthalmologist should also be performed in order to identify and record the presence of any retinal haemorrhages, which in this age group are highly indicative of NAI. A full skeletal imaging series may be required.
Due to the highly sensitive nature of this diagnosis it is important that appropriately trained specialists perform both the formal examination and the later interpretation of any imaging studies. Thorough documentation is particularly important.
IN-BORN ERRORS OF METABOLISM
The in-born errors of metabolism (IBEM) are biochemical disorders that usually occur as a result of inherited defects in enzymes that are needed to convert one metabolite to another. This leads to an accumulation of potentially toxic metabolites such as ketones, ammonia, lactate and organic acids. Clinical effects seen are due to the accumulation of these toxic metabolites and a high incidence of central nervous system effects are observed. If untreated, permanent neurological damage can ensue.
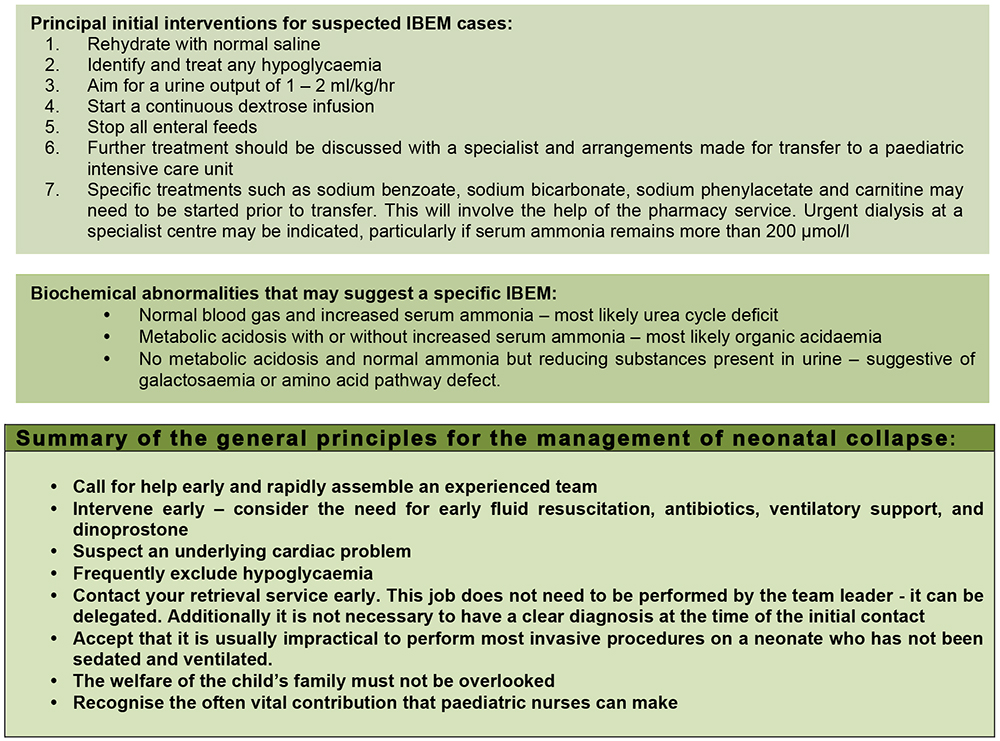
IBEM can present at any age but are more usual in the neonatal period. They normally present between 2 – 7 days after birth, coinciding with the commencement of feeds. As mode of presentation is non-specific, investigations to exclude an IBEM should be performed in all critically ill neonates. Laboratory features that may support a diagnosis of IBEM include; high or low blood glucose, metabolic acidosis, elevated lactate (which can be seen in the absence of acidosis), elevated serum ammonia, hypocalcaemia, serum ketones > 1mmol/l, acetonuria and urine pH > 5. It is important to obtain and freeze a urine sample for organic acid assay as soon as possible to aid diagnostic yield: if this is not done a false negative result may occur due to the volatile nature of these compounds.
WHAT TO DO IN THE EVENT OF THE DEATH OF A NEONATE
In the event of an unexpected death of a child where the cause is unknown the Coroner (or Procurator fiscal in Scotland) must be informed, as they will have jurisdiction over the body. The parents must be communicated with in as sensitive and caring a way as possible. Breaking bad news should be undertaken by the senior members of staff involved in a quiet, private area with time available to answer all questions. A senior member of the nursing staff should always be present. The parents should not be made to feel that they are under suspicion for the infant’s death and it is important to be honest and not to speculate if the cause of the collapse is unclear. The parents should be made aware of the involvement of the coroner and police and the need for further investigations and a post-mortem. An initial discussion should take place between the senior medical professionals and the police to agree an approach and social services should be contacted to review any relevant history. If it were not possible to take samples prior to death, post-mortem samples maybe required to aid diagnosis. You should review your local agreement with the Coroner regarding the taking of such samples and consent should be sought first from the parents and coroner.
Baseline samples to consider after discussion with a pathologist and/or biochemist include:
- Throat and nose swabs for bacterial and viral culture
- Blood culture
- Blood and urine metabolic studies (including glucose, acylcarnitine, organic and amino acids including orotic acid and sulphocysteine)- urine should be frozen
- Blood for DNA, chromosomes and dried spots on several cards
- CSF for biochemistry, glucose, culture, virology, lactate, amino acids including glycine- this should be frozen
- Skin biopsy for culture and storage of fibroblasts- sent to cytogenetics laboratory
- Muscle biopsy for electron microscopy, histopathology, enzymology- wrapped in foil and frozen to -70
Such a tragic event is undoubtedly a very distressing time for all members of staff involved. The value of a thorough debrief in which members of the team are encouraged to talk openly about the events cannot be overemphasised. Formal counselling should also be available4.
CONCLUSION
Caring for an acutely unwell neonate is both an uncommon and stressful situation. When faced with any acutely unwell neonate, help should be called for immediately and an experienced team should be assembled as soon as possible. Because the exact cause of the neonatal collapse is often not clear initially it is important to treat the neonate as if they may have any of the 4 most common causes. The initial broad aims of the management of neonatal collapse are given below.
- Perform a rapid thorough ABCDE assessment.
- Optimise oxygen delivery, fluid balance, electrolytes, blood glucose, temperature management and neurological protection.
- Identify the likely cause(s).
- Commence early appropriate treatment, accepting that this will almost always include fluid and antibiotic administration.
In common with many other areas of medicine, attention to detail and clear communication are absolutely vital. Early contact with a specialist paediatric critical care and retrieval team is advised and once the situation is resolved debrief exercises are often helpful. The performance of individuals and teams can be significantly improved by training and prior preparation. Multidisciplinary simulation is an obvious tool that should be used to achieve these goals.
ACKNOWLEDGEMENTS
We would like to thank Dr Anthony Bradley, Bristol Children’s Hospital, Dr Linda Chigaru, Children’s Acute Transport Service and Great Ormond Street Hospital, London and Professor Ibronke Desalu, Lagos University Teaching Hospital, Nigeria for their assistance in preparing these articles.
ANSWERS TO QUESTIONS
- Risk factors for neonatal sepsis include:
a. False: There is no association with gender
b. True
c. True
d. True
e. False: Caesarean section does not increase the risk of sepsis - Regarding the initial management of neonatal collapse:
a. True
b. False: 5-20ng/kg/min in first instance, but can consider increasing doses after discussion with specialist team
c. False: NICE guidance is benzylpenicillin and gentamicin. However always follow local policy
d. False: Obtaining IV access can be extremely difficult, especially if shocked or critically unwell
e. False: Dopamine is the typical first choice inotrope and can be given peripherally if sufficiently diluted - Regarding congenital heart disease (CHD):
a. True
b. False: Prostaglandins can be given by infusion to reverse functional closure of the DA
c. True: Response to dinoprostone is usually seen within 15 minutes if not one should reconsider the diagnosis
d. False: In patients with suspected CHD of unknown aetiology care must be taken with administration of high flow oxygen, as this can reduce pulmonary vascular resistance which can be disastrous in certain types of CHD such as Hypoplastic Left Heart Syndrome
e. False: A heart greater than 220bpm should increase suspicion of a neonatal tachycardia
REFERENCES AND FURTHER READING
- Kumar A, Roberts D, Wood KE et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 2006; 34(6): 1589- 1596
- NICE guidelines [CG149] Antibiotics for early-onset neonatal infection: Antibiotics for the prevention and treatment of early-onset neonatal infection. August 2012. https://www.nice.org.uk/Guidance/CG149
- The Royal College of Radiologists and The Royal College of Paediatrics and Child Health. Standards for Radiological Investigations of Suspected Non-Accidental Injury. March 2008 https://www.rcr.ac.uk/sites/default/files/publication/RCPCH_RCR_final_0.pdf
- Recommendations from a Professional Group on Sudden Unexpected Postnatal Collapse. Newborn Infants who suffer a Sudden and Unexpected Postnatal Collapse in the First Week of Life. March 2011. British Associaton of Perinatal Medicine. http://www.bapm.org/publications
- A variety of useful clinical guidelines including an approach to the investigation and management of neonatal collapse as well as guidelines on specific conditions such as the management of duct dependent congenital heart disease and in-born errors of metabolism can be found at the following sites: http://site.cats.nhs.uk, http://www.strs.nhs.uk, http://www.sort.nhs.uk
- The Wales and West Acute Transport for Children paediatric drug dose calculator can be accessed at: http://www.watchtransport.uk/page8/
- The KIDS team Drug Calculator can be accessed at: http://kids.bch.nhs.uk/healthcare-professionals-2/drug-calculator/
- Anaesthesia tutorial of the week – Intubation of sick children http://www.frca.co.uk/Documents/169%20Intubation%20of%20sick%20children%20.pdf
- Anaesthesia tutorial of the week – Resuscitation of the newborn: http://www.frca.co.uk/Documents/167%20Resuscitation%20of%20the%20Newborn.pdf
- Anaesthesia tutorial of the week – Neonatal Anaesthesia: https://www.aagbi.org/sites/default/files/65-Neonatal-anaesthesia-part-1-physiology1.pdf
- Anaesthesia tutorial of the week – Anaesthesia for the pre-term infant: http://www.frca.co.uk/Documents/259%20Anaesthesia%20for%20the%20Pre-term%20Infant.pdf
- An approach to the investigation and management of neonatal collapse (including an excellent datasheet) endorsed by the British Society of Perinatal medicine is available online at: http://www.bapm.org/publications/documents/guidelines/SUPC_Booklet.pdf
- Skone R, Reynolds F, Cray S et al. Managing the Critically Ill Child. A Guide for Anaesthetists and Emergency Physicians. 1st edn. Cambridge University Press, 2013
- Murphy PJ, Marriage SC, Davis PJ. Case studies in Paediatric Critical Care. 1st edn. Cambridge Medicine, 2009
- Brough H, Griffiths B, Champion M, Riphagen S. South Thames Retrieval Service. In born errors of metabolism. September 2015: http://www.strs.nhs.uk/resources/pdf/guidelines/inbornerror.pdf



