Covid-19
Please answer the following questions before reading the tutorial. The answers are contained in the article.
- A 70-year-old man with ischaemic heart disease has been in hospital for two days following a road traffic accident in which he sustained injuries to his spleen, bowel and several long bones. He has become markedly short of breath. What further information would you seek to make a diagnosis of ARDS?
- Describe the pathological processes occurring in the lungs of a patient with ARDS that can lead to
- Shunt
- Deadspace
- Decreased compliance
- ARDS is diagnosed in the patient in question 1. He has now been ventilated in the ICU for 3 days. You are called because the PaO2 has decreased and the airway pressures have increased. The nurse mentions that respiratory secretions have become purulent. Describe the procedures / investigations you might carry out.
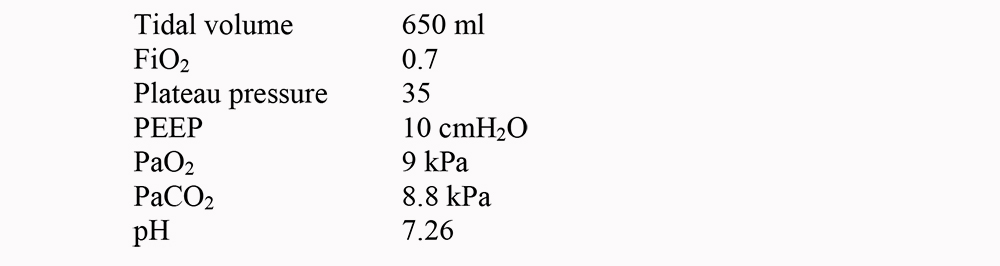
- A 70 kg patient with ARDS is being ventilated with the following settings and arterial blood gases. Which if any would you consider changing, and why?
- A 60 kg patient with ARDS is receiving volume-controlled ventilation with the following settings:
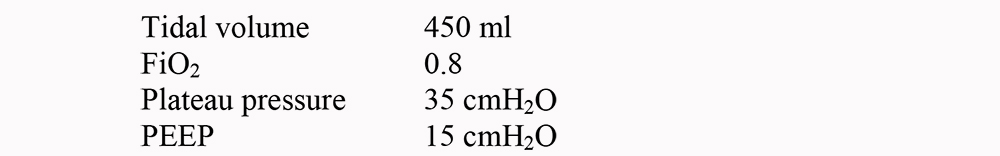 PaO2 remains less than 8 kPa. What ventilatory strategies would you consider to improve the PaO2? Which if any have been shown to improve survival?
PaO2 remains less than 8 kPa. What ventilatory strategies would you consider to improve the PaO2? Which if any have been shown to improve survival? - What are the disadvantages of using pressure-controlled inverse-ratio ventilation?
Introduction
First described in 1967, ARDS is a process of hypoxaemic respiratory failure associated with non-cardiogenic pulmonary oedema. It is the result of diffuse inflammatory damage to the alveoli and pulmonary capillaries from a range of local or systemic insults. ARDS is often associated with multiple organ dysfunction and carries a high mortality and financial cost.
Definitions
ARDS is diagnosed on clinical grounds. The most commonly used criteria were produced by the 1994 American-European Consensus Conference1.
- Acute onset
- Appropriate precipitating condition
- New bilateral fluffy infiltrates on chest x-ray (CXR)
- No clinical evidence of cardiac failure, fluid overload or chronic lung disease
- Pulmonary artery occlusion pressure of ≤ 18mmHg
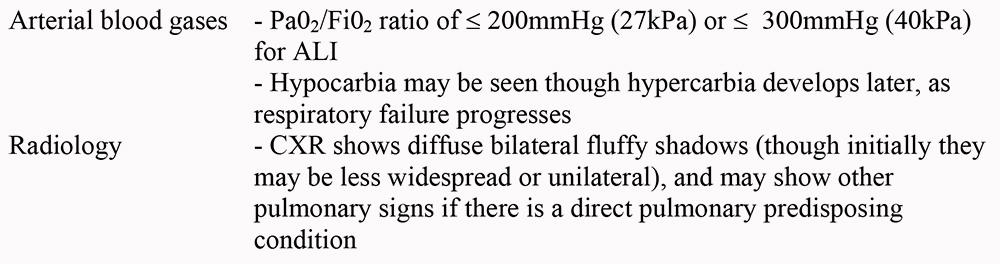
- Pa02/Fi02 ratio of ≤ 200mmHg (27kPa)
Acute Lung Injury (ALI) is a less severe form of ARDS in which the Pa02/Fi02 ratio is ≤ 300mmHg (40kPa). Note that the Pa02/Fi02 ratio is independent of PEEP. As pulmonary artery catheters are used rarely in our ICUs now the occlusion pressure ≤18 is often not sought and clinical grounds or echocardiography used to exclude cardiac failure.
Epidemiology
The true incidence of ARDS is unknown; estimates vary depending on the definitions used, with values ranging from 1.5 per 100 000 population per year to 75 per 100 000 population per year. Recent data from an Australian study which used the 1994 consensus conference definition for ARDS would suggest that one in ten noncardiothoracic ICU patients will develop ARDS.
Although ARDS may affect children it is more common in those over the age of 65, which may reflect a higher incidence of predisposing conditions. Gender has no effect.
In recent years mortality rates have decreased from about 60% to 30-40% but mortality is higher in the elderly and in patients with factors such as chronic liver disease. Most of those who die do so from sepsis or multiple organ failure and not from respiratory failure. Survivors usually have little in the way of pulmonary sequelae, although the severest cases may have restrictive lung disease
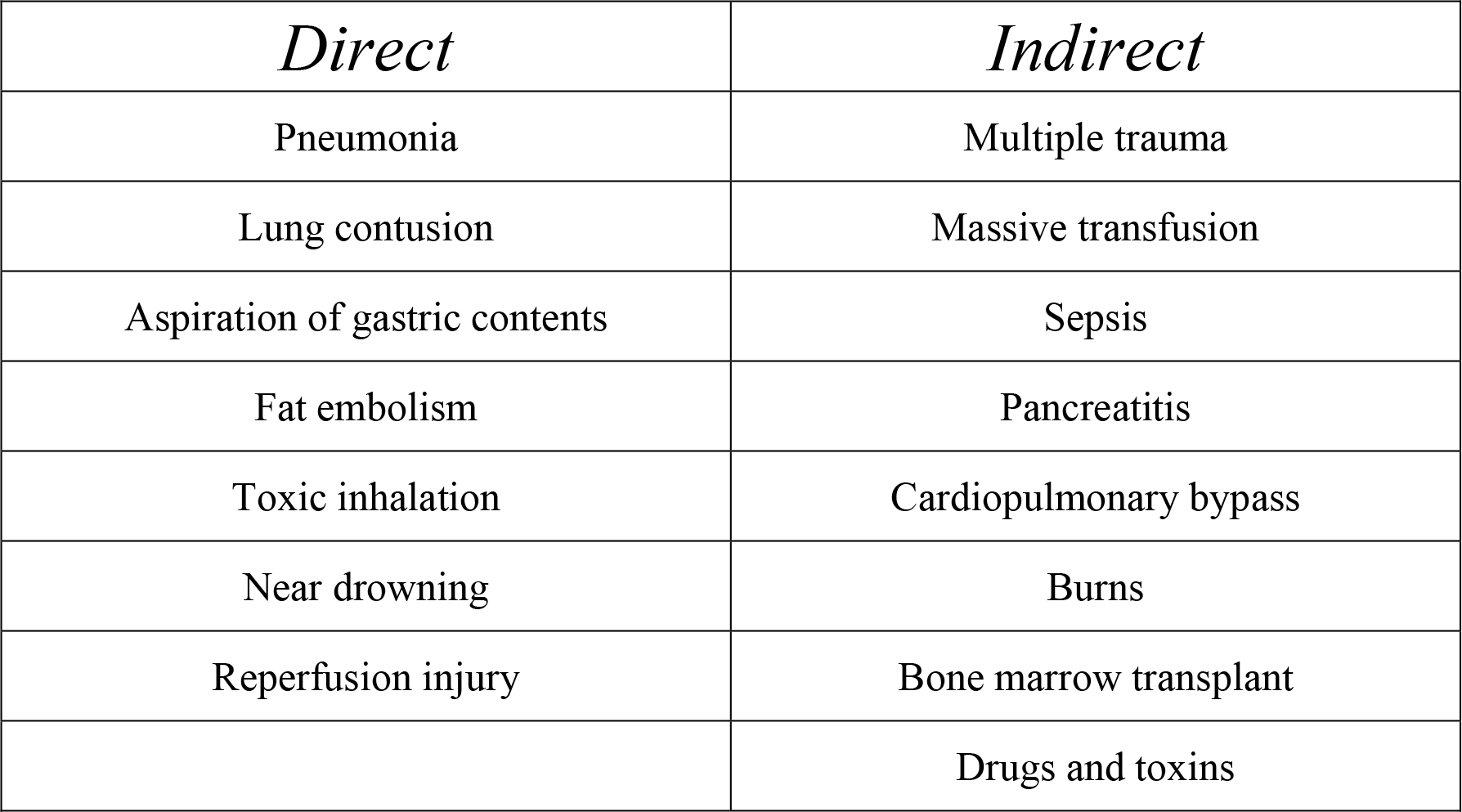
Precipitating conditions
Theses can be classified as direct or indirect
Pathophysiology
It is not understood why some individuals develop ARDS/ALI while others with the same pattern of predisposing injury do not. In those that do there are said to be three overlapping phases2: an inflammatory phase, a proliferative phase and a fibrotic phase caused by the subsequent reparative response. Patients with ARDS/ALI do not have to progress through all three phases as resolution can occur at any point. However, the severest form of ARDS will progress to the fibrotic phase.
Inflammatory phase
This lasts for one week after the onset of respiratory failure. Neutrophils accumulate in the capillaries, interstitial tissue and airspaces, and cause cell damage through the production of free radicals, inflammatory mediators and proteases. However neutrophils are not the only cell type involved as ARDS does occur in neutropenic patients. Cytokines (most importantly TNF-α, IL-1 IL-6 and IL-8) are also released by endothelial and immune cells and promote similar microvascular damage. The result is leakage of fluid and plasma proteins into the alveoli and interstitial tissues (‘non-cardiogenic pulmonary oedema’), while at the same time the plasma proteins denature alveolar surfactant causing alveolar collapse. This creates hypoxia as the fluid-filled alveoli shunt blood. Shunt is created when areas of lung receive a blood supply but are unable to oxygenate it (in this case by creating a diffusion barrier.)
To complicate matters further vasoconstriction and occlusion of pulmonary capillaries by neutrophils, platelets and fibrin also occurs leading to areas of lung that are ventilated but not perfused – deadspace.
The increase in total lung water also stiffens the lung (decrease in compliance) and this dramatically increases the work of breathing.
Proliferative phase
This phase is characterised by proliferation of type II pneumocytes and fibroblasts, with the formation of hyaline membranes. However, these pneumocytes do not make any surfactant and total production of surfactant decreases (this exacerbates the loss of surfactant caused by protein denaturing.)
Fibrotic phase
Disordered collagen deposition occurs, leading to extensive lung scarring. This makes the lung stiffer and further increases the work of breathing. This can be severe enough to make it impossible to wean the patient from a ventilator but normally it is a matter of restoring the patients muscle strength to the point where they are able to cope with the increased effort required.
Presentation
The timing of the onset of clinical features varies from a few hours to several days after the precipitating insult.
History
Shortness of breath is universal, but other symptoms are related to the predisposing condition
Examination
Findings are similar to those of pulmonary oedema due to other causes:
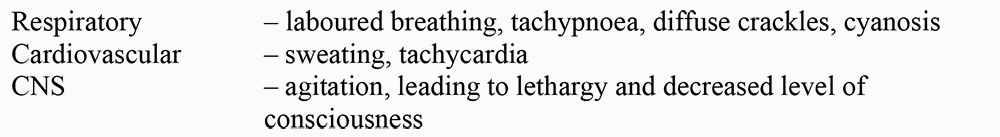
In addition there may be features of the underlying condition.
Investigations
Management (1) – supportive measures
There are no established treatments for ARDS but treating the underlying condition (for example eradicating infection with antibiotics or surgery), and providing support for each system are paramount.
Respiratory support
Frequent CXRs will help to detect pneumothorax, fluid overload and pneumonia, which may all complicate ARDS. Pneumothorax in particular should be sought if there is a sudden increase in ventilation pressures or deterioration in blood gases. CT scanning may help to show occult pneumothorax.
Frequent physiotherapy is also important, to prevent plugging of airways by sputum. If plugging is suspected (for example by lobar collapse and deterioration in blood gases) bronchoscopy and lavage can help.
Cardiovascular support
The aim is to maintain adequate oxygen delivery to the tissues
In ARDS cardiac output can be decreased due to sepsis or due to medical treatments (high ventilation pressures, PEEP, or inversed inspiratory : expiratory ratios), thus monitoring of cardiac output and filling pressures are important. This can be achieved using a pulmonary artery catheters, oesophageal Dopplers, LidCO or PiCCO devices but clinical signs are also important. Even something as simple as the presence of cold fingers implies an inadequate cardiac output (or excessive vasoconstrictor therapy). Fluid management is always difficult in these cases – excessive fluids will worsen lung function and inadequate fluids will exacerbate renal failure. With cardiac output monitoring the situation is easier – volume challenges of 250ml can be given to achieve the highest stroke volume the patient is capable of and if cardiac output is still inadequate then inotropes are indicated. If cardiac output monitoring is unavailable then systolic pressure variation can be helpful (although there are limitations such as the patient needing to be deeply sedated.) Measure the systolic blood pressure when the airway pressure is help at 30 cm H20 and when it is held at 10 cm H2O if the difference is greater than 10 mmHg then fluid may help.
Appropriate targets are cardiac output 3.5 – 5 l.min-1.m2, [Hb] 7-9 g.dl-1 (do not overtransfuse) and Sa02 ≥ 90% (see below).
Renal support
Renal failure is common, due to the underlying condition, low cardiac output, sepsis, and so on. Renal replacement therapy (for example with haemofiltration) may also improve gas exchange, by removing excess fluid.
Nutrition
Enteral nutrition should be established quickly, using nasogastric feed with prokinetics (such as metoclopramide) or nasojejunal feeding. TPN can be considered if all attempts at enteral feeding fail.
Managing Sepsis
Sepsis may have precipitated the lung injury, or may develop during the course of ARDS. However, the systemic inflammatory response syndrome is often associated with ARDS in the absence of infection, thus detecting sepsis may be difficult.
Change in sputum colour and new shadows on the CXR may point to pulmonary infection. Other sources of sepsis should be frequently reviewed (line sites, urine, wounds).
If infection is suspected, appropriate samples should be sent for microscopy and culture. This may include bronchoscopy and lavage or removing and culturing invasive line tips, for example. Lavage is particularly useful in this setting. 20 mls of normal saline are injected into the airway either through a bronchoscope or via a sterile suction catheter (placed blindly through the endotracheal tube until resistance is felt) and suctioned back into a culture pot. The likelihood of a significant positive result is higher with this technique and less tracheal contamination is encountered. Antimicrobial therapy should be guided by the results of these investigations, though ‘blind’ treatment may be reasonable if sepsis causes severe cardiovascular instability or impairment of gas exchange.
Management (2) – Ventilation
Continuous positive airways pressure (CPAP) may be of benefit in mild cases, however most patients will require early intubation and mechanical ventilation. Indications include hypoxaemic or hypercarbic respiratory failure, acidosis, exhaustion and reduced conscious level. Profound sedation is usually required for ventilation as struggling or coughing can cause loss of recruited lung and worse oxygenation. Paralysis may be necessary if sedation alone does not settle the patient.
The aim of ventilation is to improve oxygenation without causing further damage to the lungs. Difficulties arise as some alveoli are normal and open whilst other alveoli are stiff and collapsed. It is therefore necessary to try to open the collapsed alveoli without damaging the normal areas. The main causes of ventilator-induced lung damage are high Fi02 (increased free radical damage) and over-distension of alveoli. Ventilation reduces the work of breathing and reduces oxygen demand and this should help correct acidosis and improve cardiovascular stability.
With the exception of low tidal volumes (see below) there is little evidence of survival benefit for any particular ventilation strategy, however, volume-controlled ventilation is usually used initially, with the following targets:
- Fi020.5-0.6 to minimise oxygen toxicity
- Pa02 ≥ 8kPa (Sa02 ≥ 90%) – do not attempt to achieve higher values
- PaC02 < 10kPa as long as pH > 7.2. Do not attempt to achieve lower values if this requires excessively high tidal volumes (‘permissive hypercapnia’)
- Tidal volumes 6-8ml.kg-1 body weight (to minimise alveolar distension and volutrauma), as suggested by the ARDS Network study3
- Plateau pressures of 30-35 cmH20 to minimise alveolar distension and volutrauma
- Positive end-expiratory pressure (PEEP) titrated to achieve best oxygen delivery – commonly 10-15 cmH2 This increases functional residual capacity, recruits alveoli and puts the lung on the steeper part of the compliance curve. Higher levels of PEEP should be avoided, as they decrease venous return and thus cardiac output – PEEP should be set to maximise oxygen delivery rather than oxygenation alone.
- Recruitment manoeuvres. This is the use of a high level of CPAP (30-40 cmH20) for 30 seconds in an apnoeic patient via a ventilator. The aim is to recruit collapsed alveoli, and its occasional use may lead to marked improvements in oxygenation.
Pressure-Controlled Inverse Ratio Ventilation (PC-IRV)
When ventilation using the above targets fails to improve oxygenation, PC-IRV may be attempted. The key features are:
- The inspiratory time (I) is prolonged till it is equal to or greater than expiratory time (E), for example using an I:E ratio of 1:1, 2:1 or 3:1. This allows time for poorly compliant lung units to be ventilated and should improve oxygenation.
- The pressure-controlled nature of the breath allows a plateau pressure to be set, to prevent over-distension of compliant (less diseased) alveoli.
- Plateau pressures should not exceed 35 cmH20, and should be set to achieve tidal volumes of 6-8ml.kg-1 body weight
This technique has important side effects:
- Mean intra-thoracic pressures will be raised, thus decreasing venous return and cardiac output.
- The shortened expiratory time may not leave enough time for gas to escape from the lung, leading to high levels of ‘auto-PEEP’ (also called ‘intrinsic PEEP’). As well as further decreasing venous return, high auto-PEEP can impair ventilation, as the resting lung pressure becomes too high to allow expansion during inspiration. It is important therefore to periodically measure total PEEP (set PEEP plus auto-PEEP) and decrease set PEEP accordingly.
- Auto-PEEP is measured by placing the ventilator into expiratory pause and measuring the highest airway pressure created. Airway pressure should be the same as PEEP but if gas trapping occurs airway pressure will rise as the alveoli empty – auto PEEP.
- The shortened expiratory time may also lead to hypercarbia – high respiratory frequency may be needed to avoid excessive respiratory acidosis
- PC-IRV is also extremely uncomfortable for the patient, thus heavy sedation +/- paralysis are usually needed.
Ventilation in the prone position
Dramatic improvements in oxygenation are often seen in patients who are turned into the prone position for several hours, and this improvement may be sustained when they are returned to the supine position4. The technique should be used for periods of 12 – 24 hours. Prone ventilation is commonly used in patients with ARDS.
The mechanism probably involves better matching of lung perfusion with ventilation, and redistribution of dependent lung oedema. However, there are practical difficulties in turning the critically ill patient and in nursing the patient in the prone position. It should also be noted that there is no mortality benefit to be gained – at best it can buy time in cases of resistant hypoxaemia.
Management (3) – additional measures
A number of advanced techniques are available, but there is little evidence of increased survival with any of them.
- Nebulised prostacyclin – this produces pulmonary vasodilation, dilating those vessels in well ventilated parts of the lung, thus improving ventilation/perfusion matching. Because it is removed from the circulation rapidly it does not cause systemic hypotension. Prostacyclin should be continuously nebulised at a rate of 5-20 ng.kg-1.min-1
- Inhaled nitric oxide – like prostacyclin this is a selective pulmonary vasodilator, and is used in doses of 1-40 parts per million. Neither agent has been shown to influence survival.
- Corticosteroids – there is some evidence from a small study of a reduction in mortality associated with the use of methylprednisolone to suppress ongoing inflammation during the fibroproliferative phase of ARDS. The initial regimen consists of methylprednisolone 2 mg/kg daily. After 3-5 days a response must be apparent. In 1-2 weeks the dose can be tapered to methylprednisolone 0.5-1.0 mg daily. In the absence of results steroids can be discontinued.
- Surfactant therapy – aims to replace surfactant lost from the lung and thus improve compliance and alveolar stability, and decrease lung water. However early results have been disappointing.
- High frequency jet ventilation – this can be used to raise mean airway pressure without dangerous increases in peak airway pressure, but is expensive and only available in specialist centres
- Extracorporeal membrane oxygenation – a pump oxygenator performs gas exchange allows the lungs to be ‘rested’. Again, only available in specialist centres.
Summary
ARDS is diagnosed clinically on the basis of the acute development of hypoxaemic respiratory failure, CXR changes and non-cardiogenic pulmonary oedema, on the background of a pulmonary or non-pulmonary precipitating condition. ARDS may affect one in ten intensive care unit patients, and it carries a mortality of 30-40%.
Pathologically ARDS is characterised by an inflammatory phase involving neutrophils and cytokines, followed by a reparative process that may end in fibrosis.
Patients exhibit the signs and symptoms of pulmonary oedema, though features of the underlying condition may influence the picture.
Management consists of treating the underlying condition, providing support for failing systems and early invasive ventilation. Limiting the Fi02 may help to prevent further lung damage, while limiting tidal volumes to 6-8 ml.kg-1 has been shown to reduce mortality. In cases of refractory hypoxaemia PC-IRV or ventilation in the prone position may improve blood gases, but have not been proven to influence survival. In addition there are many advanced techniques but many are only available in specialist centres, and none convincingly reduce mortality.
References
- Bernard GR, Artigas A, Brigham KL, et al. The American-European Consensus Conference on ARDS: definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 1994; 149: 818-24.
- Luce JM. Acute lung injury and the acute respiratory distress syndrome. Crit Care Med 1998; 26(2): 369-76.
- Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Eng J Med 2000; 342: 1301-8.
- Gattinoni L, Tognoni G, Pesenti A, et al. Effect of prone positioning on the survival of patients with acute respiratory failure. N Eng J Med 2001; 345: 56873



