General Topics
Self Assessment
- What are the adverse metabolic consequences of insulin deficiency?
a. Increased glycogenolysis and gluconeogenesis
b. Ketogenesis and metabolic acidaemia
c. Protein synthesis
d. Dehydration
e. Lipolysis - What additional clinical/laboratory tests might you perform in a diabetic patient presenting for elective major abdominal surgery? Why might the test be useful?
a. Heart rate variability
b. Glycosylated haemoglobin (HbA1C)
c. Assessment of interphalangeal joint stiffness
d. Pulmonary function tests
e. Neurological examination - Which of the following diseases are associated with diabetes?
a. Pancreatitis
b. Acromegaly
c. Cushing’s syndrome
d. Hypothyroidism
e. Phaeochromocytoma
Key Points
- Diabetics are at increased risk of perioperative complications
- Cardiac, renal and neurological manifestations are common
- Aim for a stable plasma glucose and avoid hypo/hyperglycaemia
- Tight glycaemic control can impove perioperative outcome
Biochemical classification of Diabetes Mellitus
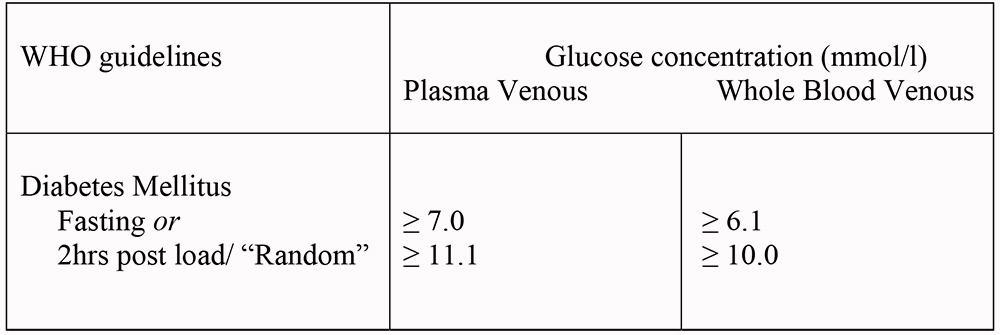
Aetiological Classification of Disorders of Glycaemia
Type 1 – Autoimmune/non-immune forms. Early onset. Beta-cell destruction. Genetic susceptibility and environmental factors implicated. Ketosis occurs with absolute lack of insulin, so previously known as “Insulin-dependent” diabetes mellitus (IDDM).
Type 2 – Previously known as “Non-insulin- dependent” diabetes (NIDDM) or “Maturity-onset”. Encompasses a spectrum of insulin hyposecretion and insulin resistance. Ketosis rare. Risk factors include obesity (especially abdominal), reduced exercise and racial origin.
Others -where the cause is known – such as gestational diabetes, drug-induced diabetes, pancreatic diseases, endocrinopathies like acromegaly/Cushing’s
Introduction
Diabetes is a multisystem disorder caused by a relative or absolute lack of insulin. The prevalence of diabetes is approximately 7%. The majority (85%) have type 2 diabetes. With increasing obesity, reduced exercise and alterations in dietary habits, the prevalence of diabetes is increasing. For every case of diagnosed type 2 diabetes, there is another undiagnosed individual.
Pathophysiology
The cleaving of proinsulin from the beta cells of the pancreas produces the peptide hormone insulin. Insulin has both excitatory and inhibitory effects. For example, it simultaneously stimulates lipogenesis from glucose whilst inhibiting lipolysis. It is the inhibitory actions, such as the tonic inhibition of lipolysis, proteolysis, glyogenolysis, gluconeogenesis and ketogenesis, that are the physiologically more important. Thus, the fasting hyperglycaemia of diabetes is due predominantly to overproduction of glucose by the liver as opposed to the commonly thought, underutilisation of glucose by peripheral tissues. In effect, insulin “keeps the brakes on” a number of key metabolic processes and prevents over-secretion of the “anti-insulin” hormones -glucagon, cortisol, growth hormone and catecholamines. These hormones also happen to be released as part of the “stress response” to surgery.
In the absence of insulin, the “brake” is removed and a sort of metabolic mayhem ensues. The resulting hyperglycaemia leads to an osmotic diuresis and dehydration with associated sodium and potassium loss. In the absence of insulin (type 1 DM), ketogeneis also occurs with associated metabolic acidaemia – a state of diabetic ketoacidosis (DKA). If there is some residual insulin activity (type 2 DM), enough to inhibit lipolysis and ketogenesis but not gluconeogenesis, then a hyperosmolar non-ketotic (HONK) diabetic coma can ensue. Both states are medical emergencies with a high mortality; the specific treatments are beyond this review.
Chronic hyperglycaemia results in microvascular (including proliferative retinopathy and diabetic nephropathy), neuropathic (autonomic and peripheral neuropathies) and macrovascular (accelerated atherosclerosis) complications. Improved glycaemic control has a beneficial effect on the microvascular and neuropathic complications in type 2 diabetes. Blood pressure control is particularly important to help prevent macrovascular complications. It is the chronic complications that need careful assessment in the preoperative period.
Preoperative Assessment
A standard assessment is required with specific attention to the following details:
Autonomic Neuropathy
Autonomic dysfunction is detectable in up to 40% of type 1 diabetics. Only a few have the typical symptoms and signs of postural hypotension, gastroparesis, gustatory sweating, and nocturnal diarrhoea. It is worth assessing all diabetic patients for autonomic neuropathy. The easiest way is to assess heart rate variability. The normal heart rate should increase by over 15 beats/minute in response to deep breathing. Neuropathy is likely is there is less than 10 beats/minute increase.
Peripheral Neuropathy
The commonest type of peripheral neuropathy is the “glove and stocking” type. However diabetics are also prone to mononeuritis multiplex and some particularly painful sensory neuropathies.
Poor patient positioning is more likely to result in pressure sores that are often slow to heal given poor peripheral blood flow. Documentation of existing neuropathy is prudent, especially if considering a regional technique.
Cardiovascular
Diabetics are more prone to ischaemic heart disease (IHD), hypertension, peripheral vascular disease, cerebrovascular disease, cardiomyopathy and perioperative myocardial infarction. Ischaemia may be “silent” as a result of neuropathy. Routine ECG should be performed and appropriate stress testing if in doubt.
Autonomic neuropathy can result in sudden tachycardia, bradycardia, postural hypotension and profound hypotension after central neuraxial blockade.
Respiratory
Diabetics, especially the obese and smokers are more prone to respiratory infections and might also have abnormal spirometry. Chest physiotherapy, humidified oxygen and bronchodilators should be considered.
Gastrointestinal
Gastroparesis is characterised by a delay in gastric emptying without any gastric outlet obstruction. Increased gastric contents increase the risk of aspiration. Always ask about symptoms of reflux and consider a rapid sequence induction with cricoid pressure even in elective procedures. If available prescribe an H2 antagonist such as ranitidine150mg plus metoclopramide 10mg, at least 2 hours preoperatively.
Airway
Glycosylation of collagen in the cervical and temporo-mandibular joints can cause difficulty in intubation. To test if a patient is at risk, ask them to bring their hands together, as if praying, and simultaneously hyperextend to 90 degrees at the wrist joint. If the little fingers do not oppose, anticipate difficulty in intubation.
Renal
Diabetes is one of the commonest causes of end-stage renal failure. Check urea, creatinine and electrolytes. Specifically check the potassium especially in view of the possible need for suxamethonium as a result of gastroparesis. If unavailable, proteinuria is likely to indicate kidney damage. Ensure adequate hydration to reduce postoperative renal dysfunction.
Immune system
Diabetics are prone to all types of infection. Indeed an infection might actually worsen diabetic control. Tight glycaemic control will reduce the incidence and severity of infections and is routine practice in the management of sepsis and diabetic foot infections. Perform all invasive procedures with full asepsis.
Other
Autonomic neuropathy predisposes to hypothermia under anaesthesia Diabetics are prone to cataracts and retinopathy. Prevent surges in blood pressure, for example at induction, as this might cause rupture of the new retinal vessels.
Hypoglycaemic Therapy
Type 1 diabetics always require insulin.
Insulin can be extracted from bovine or porcine pancreas, or more commonly now, synthesised using recombinant DNA technology.
There are three types of insulin preparation, each classified by its duration of action. Soluble insulin has a rapid onset and short duration of action. Intermediate and longer acting insulins are mixed with protamine or zinc to delay absorption, are insoluble and should only be given S/C.
Type 2 diabetics can be managed with diet alone, diet and oral agents or insulin, depending on the degree of insulin resistance and residual insulin activity.
Dietary advice and weight loss is the mainstay of therapy
There are four groups of oral hypoglycaemics (see table below).
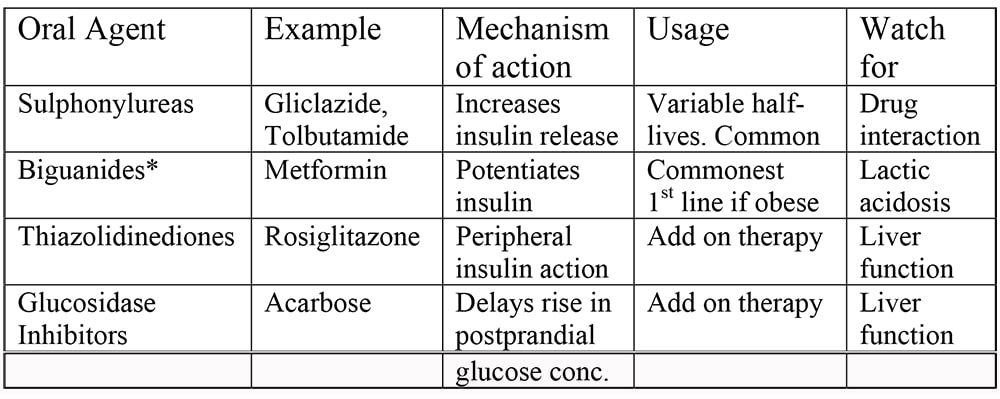
*Risk of acidosis is not as great as was thought. More likely to occur in the elderly, with associated dehydration and with higher doses. Reduce dose with renal impairment. Metformin is well tolerated, causes beneficial weight loss, has been unequivocally shown to reduce mortality and is less likely to cause hypoglycaemia than sulphonylureas. Thus it is the first choice agent if diet therapy alone fails.
Anaesthetic Management
General Principles
- Avoid hypoglycaemia (under 4mmol/l) as this can cause irreversible cerebral damage
- Avoid severe hyperglycaemia (over 14mmol/l) to minimise dehydration and metabolic upset
- Type 1 diabetics need insulin to prevent ketogenesis and “metabolic mayhem”
- Aim for a blood glucose between 6 and 10mmol/l
- Accurate, easy-to-use glucose monitors, make the practice of “permissive hyperglycaemia” unacceptable given the known outcome benefits of tight control
- Diabetic patients should be placed first on the operating list to shorten the preoperative fast and potentially allow normal oral intake later that same day
- Tight metabolic control is important for both type 1 and type 2 patients. If control has been tight in the preceding weeks then fluid and electrolyte balance will be essentially normal.
The best marker for recent control is the percentage of glycosylated haemoglobin (HbA1C). If available, levels less than 7% indicate good control whilst levels over 9% and particularly 12%, indicate poor control and likely associated electrolyte and water loss. These patients should be admitted preoperatively for correction of these abnormalities and stabilisation of blood sugar levels before the addition of surgical stressors.
If this is unavailable, try to assess control by looking at the patient’s own log of urine or blood glucose.
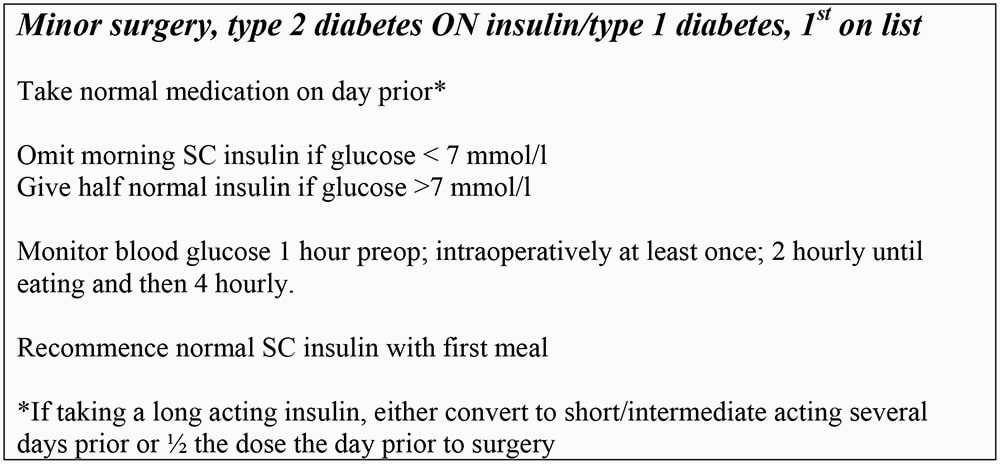
- Continue all diabetic medication until the day of surgery except:
a.) Chlorpropamide (stop 3 days prior as long acting, substitute with a shorter acting sulphonylurea)
b.) Metformin only if major surgery as risk of lactic acidosis
c.) Glitazones
c.) Long acting insulin – substitute with short/intermediate acting - Measure blood sugar preoperatively – 4 hourly if on insulin, 8 hourly if not
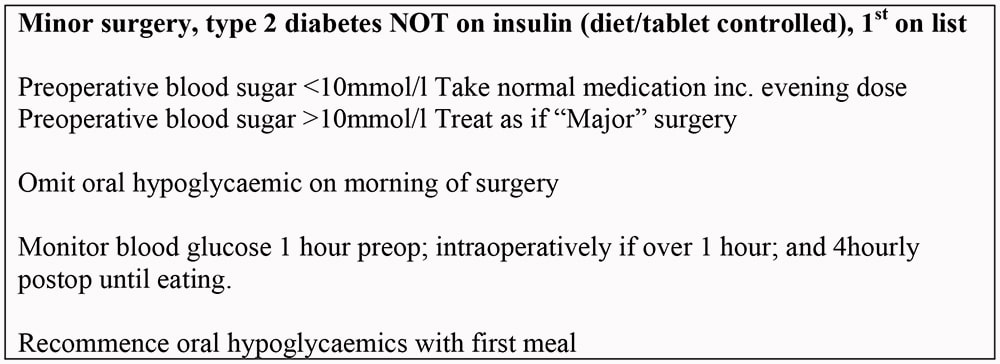
- If the patient is expected to eat within 4 hours of the operation then treat this group as having “Minor” surgery. Otherwise, surgery is “Major”
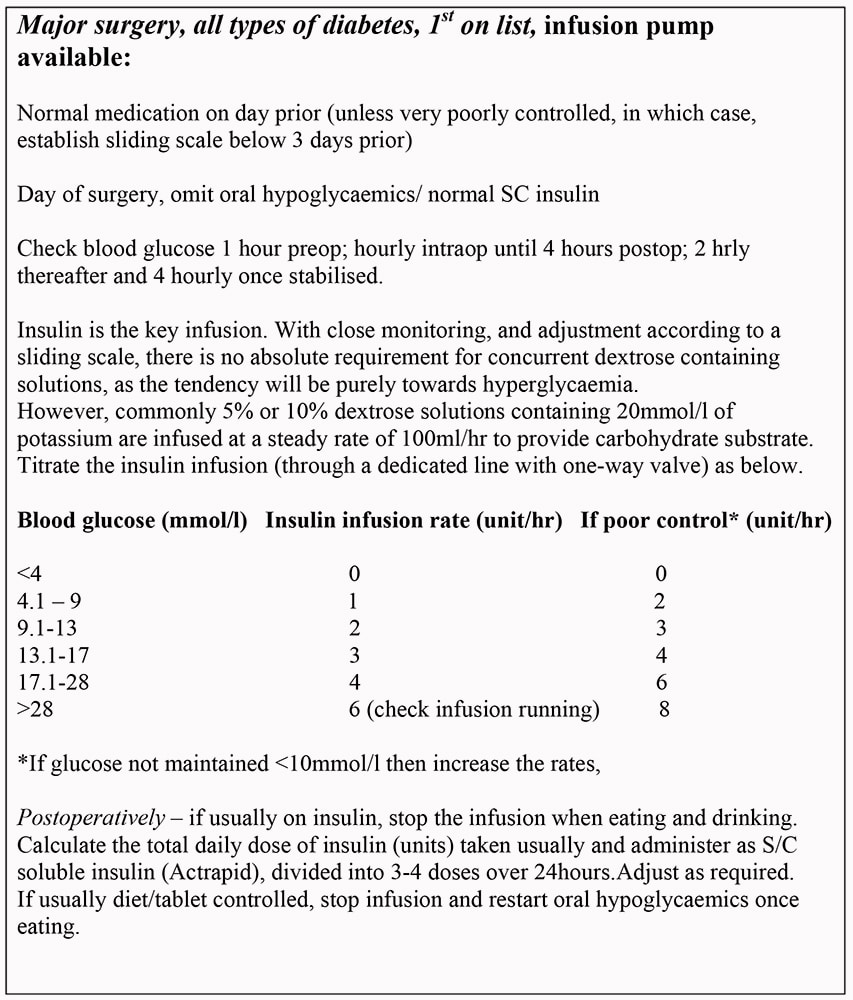
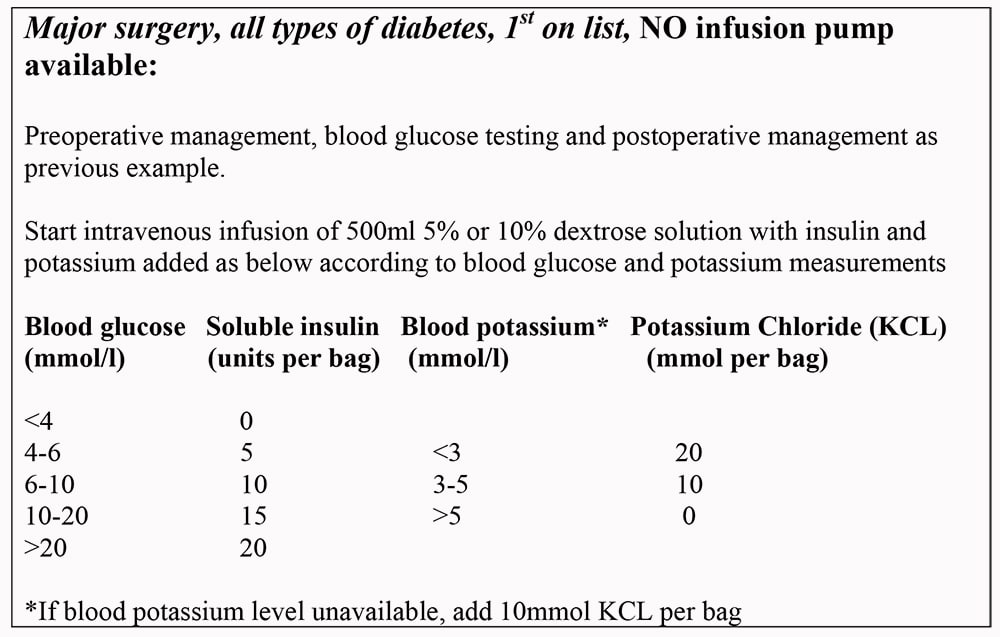
- If local guidelines exist, follow those for continuity of practice. Below are some examples of diabetic protocols
Hypoglycaemia
Defined as blood glucose less than 4mmol/l, hypoglycaemia is one of the main dangers to patients in the perioperative period. In the awake patient, the usual warning symptoms and signs include profuse sweating, pallor, light-headedness, tachycardia, confusion and incomprehensible speech progressing to convulsions and coma.
Irreversible brain damage can occur. Alcohol consumption, liver disease, fasting and sepsis exacerbate hypoglycaemia. Hypoglycaemia may also result inadvertently by poor blood glucose monitoring or equipment failure.
The best warning sign, that of the conscious patient detecting a forthcoming “Hypo”, is lost under general anaesthesia together with most of the other signs.
Frequent monitoring of blood glucose, and appropriate adjustments to therapy is the key in prevention
Once detected, give 25ml of 50% dextrose intravenously and repeat if blood sugar measurement doesn’t increase. Glucagon 1mg IM or IV is an alternative but slower strategy. If the patient is awake, try any sugary food/solution to hand
Regional anaesthesia and diabetes
Regional techniques are not contraindicated in the diabetic patient and offer some potential advantages such as the avoidance of intubation, having an awake patient to warn of impending hypoglycaemia, and an earlier return to normal eating patterns.
Document any existing motor/sensory neuropathies prior to performing any blocks and look for evidence of autonomic neuropathy. If present, expect increased hypotension after neuraxial blocks. The chances of epidural abscess are also increased.
Conclusion
The diabetic patient provides many challenges to the anaesthetist, most of which can be anticipated with good preoperative assessment, careful monitoring and an understanding of the relevant pathophysiological features. Regional techniques might reduce some of the associated risks but require similar vigilance.
Answers to self assessment
- T T F T T
See text for answers – proteolysis resulting in poor wound healing - T T T T T
a. Heart rate variability to assess for autonomic neuropathy
b. Glycosylated haemoglobin is used to measure recent glucose control. Levels are less than 6.2% in normal subjects. A level of 7% or under indicates good recent control in a diabetic patient. If the level is over 9% then control has been poor and thus the metabolic consequences are likely to be more pronounced with associated dehydration and electrolyte loss. Levels over 12% indicate incipient ketoacidosis. Correcting electrolyte and water losses preoperatively and “shutting off” lipolysis and proteolysis with insulin should improve outcome.
c. See text – may herald a difficult airway/intubation
d. Diabetes is associated with obstructive spirometry and altered diffusing capacity
e. Documentation of pre-existing neuropathy is vital if considering a regional technique. Neuropathic patients are particularly liable to further neuropathy –position and pad with care. Significant neuropathy should warn of system involvement elsewhere e.g. cardiac/renal - T T T F T
a-c. See Text
d.e. Hyperthroidism is associated with diabetes as is phaeochromocytoma
References and further reading
- Sonksen P, Sonksen J. Insulin: understanding its action in health and disease. Br J Anaesth 2000, 85: 69-79
- McAnulty GR, Robertshaw HJ, Hall GM. Anaesthetic management of patients with diabetes mellitus. Br J Anaesth 2000, 85: 80-90
- French G. Clinical management of diabetes mellitus during anaesthesia and surgery. Update in Anaesthesia 2000, 11: Article 13



