Paediatric Anaesthesia
QUESTIONS
Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation.
- Which of the following statements are true or false?
- The peak age for OSA in children is in the teenage years
- Young children with OSA are generally obese
- Children with severe OSA are at high risk during anaesthesia
- Children with severe long-standing OSA may develop pulmonary hypertension
- Name 4 key clinical questions to diagnose OSA in children
- Which of the following statements are true or false?
- A child presenting for elective tonsillectomy for OSA who has a cold should have surgery postponed.
- An oral airway may be useful on induction in a child with OSA
- Young children with severe OSA undergoing tonsillectomy are best managed with a laryngeal mask airway.
- Children with OSA have increased opiate sensitivity
- Children with severe OSA benefit from a nasopharyngeal prong airway on the first night of surgery after tonsillectomy
- Children with OSA may be safely managed as a day case after tonsillectomy.
INTRODUCTION
Sleep disordered breathing in children describes a continuum of disorders ranging in severity from primary snoring which is seen in 20% of children, to obstructive sleep apnoea which is seen in 2% of children. This tutorial will discuss the definition of sleep disordered breathing (SDB) in children, the aetiology, the diagnosis, pathophysiology and clinical features, and the anaesthetic management of a child with OSA.
SLEEP DISORDERED BREATHING IN CHILDREN
SDB in children encompasses primary snoring, upper airways resistance syndrome, obstructive hypopnoea and obstructive sleep apnoea (1,2).
Primary snoring is defined as noisy breathing during sleep without desaturation or obstructive episodes and without daytime symptoms. It is due to increased nasal airflow turbulence and vibration of pharyngeal structures. It has previously thought to be harmless, but some children may suffer from frequent microarousals during sleep leading to poor school performance. Symptoms usually resolve as the child grows and the dimensions of the airway increase. Some children with poor school performance may benefit from adenotonsillectomy.
Upper airways resistance syndrome (UARS) is defined as snoring associated with sleep disruption and arousal, with daytime symptoms but no abnormalities of gas exchange at night.
Obstructive hypoventilation (OH) occurs when upper airways resistance is increased sufficient to cause paradoxical ventilation (loss of synchrony between thoracic and abdominal movements), with desaturation and or carbon dioxide retention.
Obstructive sleep apnoea (OSA) is the most severe form of SDB when children demonstrate cessation of nasal/oral airflow during sleep with preserved thoracic and abdominal respiratory effort and oxygen desaturation.
OSA in children shows distinctive differences from OSA in adults. The typical clinical picture of severe OSA (type I OSA) is a young child where the parents are concerned about the child’s breathing at night, the child has noisy breathing associated with ‘snorts’ after periods of apnoea, and the parents have to shake the child or reposition them during sleep. The child is not gaining weight despite good appetite, may be hyperactive with behavioural difficulties by day, habitually mouth breathes and has a blocked nose. It has recently been recognised that there is an emerging subset of obese adolescents with OSA (‘type II OSA’) who have similar clinical features to adults with OSA (see table 1).
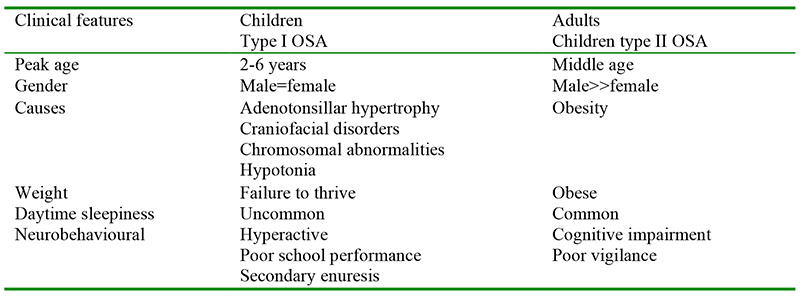
Table 1. Clinical features of OSA in children and adults (2)
AETIOLOGY OF SLEEP DISORDERED BREATHING IN CHILDREN
The most common aetiology of SDB in children in children is adenotonsillar hypertrophy. This becomes clinically significant in the 2-6 year age group as the adenoids and tonsils enlarge but the absolute size of the airway is still small. The tonsils may be large enough to meet in the midline (‘kissing tonsils’). African children tend to be more severely affected by SDB than Caucasian children. Other causes of SDB include chromosomal abnormalities such as Downs syndrome (mild mid-face hypoplasia, large tongue, generalised hypotonia), craniofacial abnormalities associated with severe mid-face hypoplasia such as Aperts or Crouzons syndrome; Treacher-Collins or Pierre Robin sequence (micrognathia); cerebral palsy (hypotonia); sickle cell disease (lymphoid hyperplasia); papillomatosis, cystic hygroma (foreign body). Obesity is becoming an increasingly common cause of OSA in older children.
PATHOPHYSIOLOGY
Children with ‘type I’ OSA have failure to thrive, central nervous system and cardiovascular complications. Failure to thrive is possibly due to reduced caloric intake, increased work of breathing at night, or reduced secretion of growth hormone. Central nervous system complications include memory, learning and behavioural problems as a consequence of sleep disturbance. There is some evidence that the CNS complications may be related to an inflammatory response secondary to repeated nocturnal hypoxia. Cardiovascular complications are of particular interest to the anaesthetist. Severe OSA with repeated nocturnal hypoxia is associated with pulmonary hypertension which if severe and long-standing may result in right heart failure. This situation is not commonly seen in UK practice. The clinical history is of a child with long standing severe OSA with general ill health and failure to thrive, who rather than being hyperactive by day is listless and has reduced activity. Clinical examination reveals the cause of OSA (e.g. signs of adenotonsillar hypertrophy, narrow midface) and signs of cardiomegaly that may be confirmed on CXR. The CXR may also demonstrate prominent central pulmonary arteries. An ECG reveals signs of right ventricular hypertrophy (right axis deviation, peaked P waves, tall R waves in lead V1). Echocardiography confirms the diagnosis of pulmonary hypertension, right ventricular hypertrophy +/- dilatation. These children are at high risk during anaesthesia (see below) but signs and symptoms resolve completely within months of treating the OSA (4).
Children with type II OSA are obese and may suffer from systemic hypertension in common with adults with OSA. Adenotonsillar hypertrophy may contribute in part to OSA and these children may benefit from tonsillectomy. Nasal cpap may be the treatment of choice.
DIAGNOSIS OF SDB IN CHILDREN
The ‘gold standard’ to diagnose SDB in children is using an overnight sleep study in a sleep laboratory (polysomnography) that includes measures of nasal airflow, chest wall and abdominal wall movement, a continuous monitor of expired CO2, and oxygen saturation. However the facilities to do formal sleep studies are expensive and not widely available and are only indicated where there is some diagnostic uncertainty. There is little uniformity between different units in the definition of severity of OSA, but they generally include a measure of apnoeic events (central or obstructive), CO2 clearance and desaturation events (baseline saturation, number and severity of desaturation <92%).
‘Mini sleep studies’ using overnight pulse oximetry and heart rate monitoring give an excellent measure of severity of OSA in children, and may be performed on the ward or more usefully at home.
Clinical diagnosis of OSA. Many units in the UK rely on a clinical diagnosis of OSA in children. There are some key questions to ask in the clinical history (2):
- Does your child snore at night?
- Do they stop breathing?
- Do they sweat?
- Are they restless?
- Does you child breathe through their mouth when awake?
- Is there a family history of OSA?
- Does your child have behavioural problems?
At GOSH we use a clinical score of severity (3) (table 2)
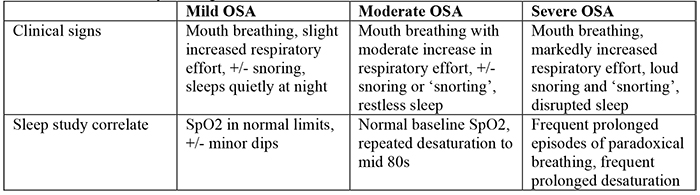
Table 2. OSA severity scoring
ANAESTHETIC MANAGEMENT OF A CHILD WITH OSA
Surgical and anaesthetic preassessment should identify those children at high risk for complications after adenotonsillectomy, and plans for perioperative and postoperative care made as appropriate (5):
- Age < 3 years
- Severe OSA
- Failure to thrive
- Cardiac complications
- Obesity
- Prematurity
- Recent URTI
- Craniofacial abnormalities
Children with OSA with a cold should be postponed for 4 weeks. Children with signs and symptoms suggestive of severe OSA with cardiac involvement (rare in UK practice) need to be assessed by a cardiologist prior to surgery (4). Our practice with these children is to insert a nasopharyngeal prong airway in the first instance (to relieve the airway obstruction), treat the cardiac failure, and then if indicated, proceed to definitive surgical treatment for the OSA. The improvement is not immediate, but children are dramatically improved in the weeks after surgery.
Sedative premedication should be avoided for children with OSA and it is our practice to allow the parents to accompany the child to the anaesthetic room to reduce the child’s anxiety. Induction may be gaseous or intravenous, depending on the child and the preference of the anaesthetist.
Induction may be gaseous or intravenous, depending on the child and the preference of the anaesthetist. Those with severe adenotonsillar hypertrophy and/or midface hypoplasia obstruct their airway almost immediately after induction with the loss of pharyngeal tone – obstruction may be relieved by jaw thrust and the application of cpap. An oral airway should be inserted as soon as the child is deep enough and effectively relieves the obstruction. Obstruction on induction is usually a good indication that the child will require a nasopharyngeal prong airway after surgery (see below). These children are usually easy to intubate. Children with severe micrognathia on the other hand will not be easy to intubate – a cautious gas induction is sensible in this situation.
It is our practice to intubate and electively ventilate children with severe OSA, usually using a short acting non-depolarising nmj blocker. Intubation under deep anaesthesia without muscle relaxant is unwise in this situation – suxamethonium should be used if non-depolarising agents are not available. A laryngeal mask airway is not suitable for small children with OSA and adenotonsillar hypertrophy. The children are extubated awake at the end of surgery.
Children with severe OSA have increased opioid sensitivity and have been estimated to require 50% less opioid than normal children (6). This is postulated to be due to up-regulation of μ opioid receptors (7). Analgesia should be carefully titrated to effect. Simple analgesics should be used (and for general surgical procedures in children with OSA, regional blocks); opioid analgesia should be kept to a minimum in the postoperative period. It is our practice to use regular paracetamol and NSAIDs, including for children with tonsillectomy. The risk for increased reoperations for bleeding due to NSAIDs is more than offset by improved analgesia, avoidance of opioids, and reduced PONV (8). It is our current practice to use ondansetron and a small dose of dexamethasone (0.1mg/kg, maximum dose 4mg) for PONV.
Airway obstruction is not relieved immediately after surgery in children undergoing adenotonsillectomy for severe OSA. This is mainly due to oedema and swelling at the operation site, which improves in the first 24-48 hours after surgery (9). It is our practice to electively insert a nasopharyngeal prong airway (NP airway) for these children at the end of surgery (10). The surgeon prepares the NP airway at the end of the operation. A tracheal tube the same size as that used for surgery (or 1⁄2 size smaller) is placed into the right nostril (so that the bevel of the tube faces medially); the tube is positioned so that the tip protrudes 0.5 cm below the soft palate. The tube is cut to length, attached to a tube connector and taped in position to the child’s face. It is important to obtain the correct length of NP airway – too short and it is ineffective, too long at it causes laryngeal irritation and continuous coughing. The child is nursed on the ward with the NP airway in position for the first night at least – it is very important that the nursing staff regularly suction the airway with soft suction catheters, inserting them only 0.5 cm beyond the NP airway. Since we have been using NP airways routinely we longer admit children with severe OSA to the intensive care unit after adenotonsillectomy.
All children with severe OSA should be admitted after surgery for careful overnight observation. We use saturation monitoring as part of routine monitoring on the ward, but do not administer oxygen to those with severe OSA unless required; a small minority of patients with OSA will rely on hypoxic drive to maintain ventilation, so oxygen is best avoided unless the saturation is <90%.
SUMMARY
In summary, sleep disordered breathing in children may vary from simple snoring to severe OSA. Severe OSA is due to a variety of causes, the most common of which is adenotonsillar hypertrophy in young children. Severe OSA results in failure to thrive, behavioural problems, and rarely in the worst cases, pulmonary hypertension with right heart failure. Children with OSA should be anaesthetised with care; deep anaesthesia should be avoided and they are sensitive to opioids. Those undergoing adenotonsillectomy should be cared for in a monitored environment postoperatively as the obstruction will not be relieved on the first postoperative night (swelling at the surgical site); and there is the added risk of the effects of residual anaesthesia. A nasopharyngeal prong airway should be considered; it has revolutionised our care of these patients.
ANSWERS TO QUESTIONS
- Question 1
- False. The peak age for OSA in children is the 2-6 years age range when the adenoids and tonsils develop.
- False. Young children with OSA may have severe failure to thrive due to disturbed sleep and increased work of breathing at night, reduced calorie intake during the day, and possibly due to reduced secretion of growth hormone (GH). GH secretion is maximal during sleep.
- True. Young children with severe OSA are at risk of hypoxia on induction of anaesthesia due to loss of pharyngeal tone.
- True. This is uncommon in UK practice but may be more common in areas where tonsillectomy is rarely performed as an elective procedure. In a child with severe OSA and pulmonary hypertension, increased hypoxia on induction may lead to further increase in pulmonary vascular resistance, right heart dilatation, compression of the left ventricle and loss of coronary blood flow leading to cardiac arrest. Children with severe right heart failure should have a nasopharyngeal airway inserted to relieve the OSA in the first instance, and heart failure treatment before surgery
- Question 2 – Key questions to diagnose OSA in children:
- Does your child snore at night? (Do they stop breathing, do they sweat, are they restless at night)
- Does your child breathe through their mouth when awake?
- Is there a family history of OSA?
- Does your child have behavioural problems?
- Question 3
- True. A child presenting for elective tonsillectomy for OSA who has a cold should have surgery postponed as a cold, airway surgery and OSA are all independent risk factor for increased complications after surgery.
- True. An oral airway may be useful on induction in a child with OSA as the airway obstruction will increase as pharyngeal tone is lost.
- False. Young children with severe OSA undergoing tonsillectomy are best managed by intubation and ventilation; there will not be sufficient room for the surgeon to operate safely in a young child with sever OSA if an LMA is used.
- True. Children with OSA have increased approx 50% increased sensitivity to morphine.
- True. A child who has a tonsillectomy for OSA may have residual airway obstruction on the first night of surgery due to oedema, blood and secretions and the residual effects of anaesthesia. A nasopharyngeal airway is useful to relieve residual airway obstruction.
- False. Child with severe OSA should be monitored in hospital after tonsillectomy
REFERENCES
- Lerman J. A disquisition on sleep-disordered breathing in children. Pediatric Anesthesia 2009 19: 100-108
- Schwengel D et al. Perioperative management of children with obstructive sleep apnoea. Anaesthesia and Analgesia 2009 109: 60-75
- Ahmed et al. The role of the nasopharyngeal airway for obstructive sleep apnoea in syndromic craniosynostosis. The J Craniofacial Surgery 2008 19: 660-3
- Wilkinson et al Electrocardiographic signs of pulmonary hypertension in children who snore. BMJ 1981 282:1579-81
- American Academy of Pediatrics Clinical Practice Guidelines. Pediatrics 2002 109: 704-712
- Brown K et al. Recurrent hypoxaemia in children is associated with increased analgesic sensitivity in children Anaesthesiology 2006 105: 665-9
- Lerman J. Unravelling the mysteries of sleep disordered breathing in children. Anesthesiology 2006 105: 645-7
- Moiniche et al. Nonsteroidal anti-inflammatory drugs and the risk of operative site bleeding after tonsillectomy: a quantitative systematic review. Anesthesia and Analgesia 2003 96: 68-77
- Nixon GM et al. Sleep disordered breathing on the first postoperative night after adenotonsillectomy for obstructive sleep apnoea. Pediatric Pulmonology 2005 39: 332-8
- Tweedie et al The nasopharyngeal prong airway: an effective postoperative adjunct after adenotonsillectomy for obstructive sleep apnoea in children Int J Pediatric Otorhinolaryngology 2007 71: 563-69



