General Topics
Before reading the tutorial, please complete these MCQs.
Multiple Choice Questions
- In Benign Prostatic Hypertrophy:
- The incidence is not related to age
- All patients require surgery
- Symptoms do not always correlate to prostate size
- Renal impairment may be a complication
- Lymph node involvement may occur
- Trans urethral resection of the prostate (TURP):
- May be used for prostates over 80 grams
- Diathermy is used
- The patient is supine
- Normal saline is used to irrigate the bladder
- Bladder perforation is extremely rare
- With regards to TURP syndrome:
- Transient blindness may occur if glycine solutions are used
- The diagnosis may be made sooner if general anaesthesia is used
- Haemolysis is less of a problem if isotonic solutions are used
- Irrigating fluid is absorbed mainly through the bladder
- Fluid overload may only become apparent as a regional block wears off
- Radical Prostatectomy
- Carries about a 0.2% mortality
- Is used for large prostates with BPH
- Post-operative complications include thromboembolic events
- Blood loss is usually minimal
- Regional anaesthesia is not appropriate for this surgery
- Methods to reduce blood loss in prostatic surgery include:
- Use of regional anaesthesia
- Methoxamine
- Pre-operative heamodilution
- Good surgical technique
- Reducing the height of the irrigating fluid in TURP
Key Points
- Patients are usually elderly, and may have co-existing medical problems.
- Blood loss may be a problem with all types of prostatic surgery.
- Regional anaesthesia carries many benefits.
Introduction
The prostate is a secretory secondary sexual organ which is wrapped around the urethra between the urinary bladder and pelvic floor. It is innervated by both sympathetic and parasympathetic nerves, which arise from T11 to L2 (sympathetic) and S2 to S4 (parasympathetic). The common conditions affecting the prostate are benign prostatic hypertrophy (BPH) and cancer.
BPH is an ageing process which leads to bladder outflow obstruction. Complications includerecurrent infections, stone formation, haematuria and impairment of renal function. Drug treatment may be used as a first line measure, usually with specific inhibitors of 5 alphareductase (e.g. finasteride) or uro-selective alpha blockers (eg. prazosin).
Prostate cancer is a common malignancy, being the second leading cause of cancer death in men in USA. Risk factors include increasing age, positive family history and there are racial variations. The risk is lowest in Asian males, higher in North Europeans and highest in African Americans. Many patients present late, with metastatic disease which is usually to bones or lymph nodes. Prostate specific antigen (PSA) levels in the blood may be used as a screening test for prostate cancer, although it is not diagnostic. Digital rectal examination is important in diagnosis, and fine-needle aspiration or tru-cut biopsy (which may be ultrasound guided) gives a definitive diagnosis. Radical prostatectomy is reserved for those with disease confined to the prostate. Conservative treatment with radical radiotherapy or anitandrogen therapy may also lead to cure Palliative care for more advanced disease includes local radiotherapy or analgesia for bone pain, and symptomatic treatment for urinary symptoms, which may include surgery.
Anaesthetic problems
Patients presenting for prostate surgery are often elderly and may have co-existing morbidities. Cardiovascular and respiratory problems are not uncommon, and they are often on various medications. Specific problems related to their prostatic disease include an element of renal impairment, anaemia due to recurrent haematuria, or urinary tract infection. Pre-operative investigations should be targeted appropriately to investigate these and any other medical problems.
Prostatic surgery carries a high risk of intra-operative bleeding, and so ideally all patients should have blood taken for cross matching. Anticoagulant drugs such as aspirin and non-steroidal anti-inflammatory drugs should be stopped 10 days prior to surgery. Patients on warfarin must be considered on an individual basis in conjunction with their physician. Those requiring continuous anticoagulation may need to be changed into intravenous heparin, which can then be stopped for the duration of surgery.
Transurethral resection
This is commonly used for BPH, but requires specialised surgical equipment. It is also not suitable for very large prostates (more than about 80 grams) The patient is placed in the lithotomy position. A resectoscope (a modified cystoscope) is inserted into the urethra and slices of prostate are removed using a bare wire and cutting diathermy. Bleeding vessels are coagulated using a roller ball diathermy instrument. The field is continuously irrigated with warmed fluid to distend the bladder and wash away blood and dissected prostatic tissue. The prostatic chips may be collected and examined histologically for any evidence of malignancy.
An irrigating catheter is often left in place post-operatively to wash away any bleeding and prevent clot retention of urine. This may be removed once the effluent fluid is clear of blood. Hospital stay is usually 1 to 2 days, although there have been reports of same day discharge.
Complications
TURP Syndrome. Irrigating solution will be absorbed through the large prostatic venous sinuses. The extent to which this occurs depends on the height of the irrigating solution container above the surgical table (resulting in hydrostatic pressure driving the fluid into the sinuses) and the resection time. Electrolyte solutions cannot be used as they are highly ionised and facilitate dispersion of the high frequency diathermy current. Distilled water has been used, although absorption of large quantities of water leads to red blood cell haemolysis and hyponatraemia. Isosmotic solutions of non-electrolytes are now used, most commonly glycine and Cytal (a combination of mannitol and sorbitol). Excessive absorption of these solutions will lead to circulatory overload, pulmonary oedema, cardiac failure and even cardiac arrest. Hyponatreamia may still occur to a limited extent, and can cause central nervous system (CNS) effects such as agitation, confusion, convulsions and coma. High blood levels of glycine may also cause CNS symptoms, most commonly transient blindness, as it is an inhibitory neurotransmitter. Glycine is also metabolised to ammonia and high blood levels of ammonia have been associated with delayed awakening after TURP.
Preventative measures include limiting the height of the irrigating solution container to 60cm above the patient, limiting the volume of irrigant used and restricting resection time to 60 minutes. The risk is also reduced by having more experienced surgeons who will have better surgical technique and shorter operative time.
Specific treatment consists of fluid restriction and loop diuretics such as furosemide. Hypertonic saline is no longer used due to its CNS complications. Cardiac failure and CNS effects are managed supportively according to their severity. Ventilation may be required in extreme cases.
Bladder perforation. This may occur in up to 1% of cases. Most are extraperitoneal, and cause periumbilical or suprapubic pain in the awake patient under regional anaesthesia. Intraperitoneal bladder perforation leads to generalised abdominal pain, which may be referred from the diaphragm to the chest or shoulder. It may also be associated with pallor, sweating, hypotension and nausea and vomiting.
Bleeding may be substantial, and depends on the size of the prostate, length of surgery and surgical technique. It may be difficult to estimate due to dilution with irrigating fluid. Rough estimates of blood loss include 2-5mL per minute of resection time, and 20-50mL per gram of prostate resected. Monitoring of the patients vital signs and haematocrit level are probably the best way to assess blood loss and the need for transfusion
Abnormal bleeding may be due to the release of plasminogen activator from the prostate, which results in fibrinolysis. This occurs in less than 1% of cases and may be treated with aminocaproic acid.
Other. Significant heat loss may can result from the use of cold irrigating fluid.
Perforation of the rectum may occur, which requires a defunctioning colostomy.
Open Prostatectomy
These operations are associated with a longer hospital stay of up to 1 week. A urinary catheter is usually placed and removed on day 4 to 6.
Retropubic (Millin) prostatectomy. This operation is used for BPH. The prostate is approached through a Pfannenstiel incision with the patient supine. The capsule of the prostate is incised and the lobes of the prostate are enucleated. The bladder neck is then repaired. Bleeding may be profuse during enucleation of the prostate, but is usually short-lived.
Supraprapubic transvesical prostatectomy. The prostate is approached through an incision in the bladder and is then enucleated. The skin incision may be Pfannensteil or midline, below the umbilicus. The bladder is usually irrigated with saline during the procedure, although the operation can be done without this. Bleeding may occur, but is usually easy to control. Postoperatively a suprapubic catheter may also be used.
Perineal prostatectomy. With the patient in the lithotomy position, an incision is made between the rectum and scrotum. The prostate is approached through the ischio-rectal fossa. Again, bleeding may occur.
Radical prostatectomy. These operations are for malignant disease, and involve removal of the entire prostate gland and local lymph nodes. The prostate may be approached through the retropubic, suprapubic or perineal routes. If the patient is placed in the supine trendelenberg position with the pubis above the head, venous air embolism may occur. Massive blood loss is the major complication, and most patients require transfused blood. As with any long operation, careful patient positioning and methods to reduce heat loss are important. Thromboembolic events and wound infection may occur post-operatively, and the operation carries a mortality of around 0.2%.
Anaesthesia
Regional anaesthesia may be used for prostatic surgery. A surgical block to the level of T10 is required, and the caudal, subarachnoid (spinal) or epidural routes may be used. The addition of short acting opiates (for example fentanyl) may reduce the dose of local anaesthetic needed to provide an adequate block. Approximate doses for these blocks are shown in table 1. Due to the long operative time for a radical prostatectomy, a single shot technique may not be of sufficient duration. Epidural or combined spinal and epidural anaesthesia with an epidural catheter is the best regional method, with the advantage that the epidural may be used post-operatively for pain relief.
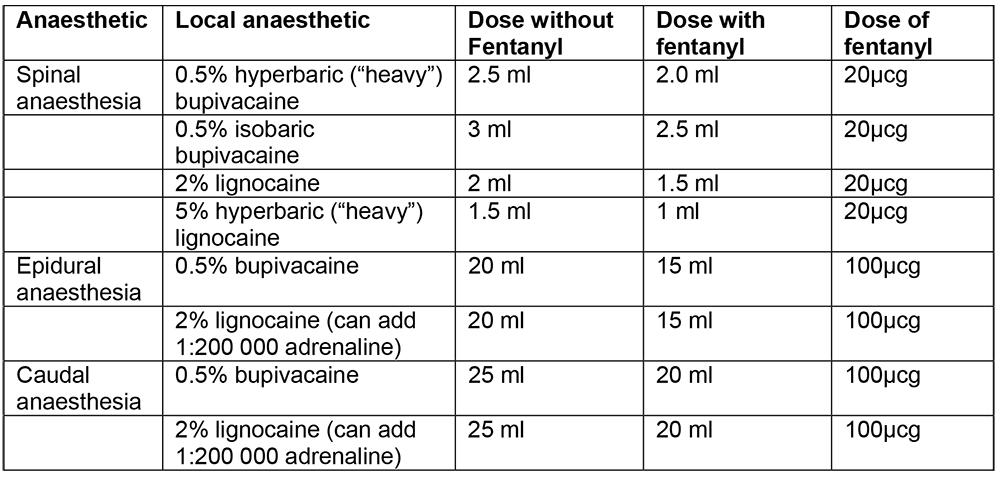
Table1. Approximate doses of local anaesthetic for regional block.
Regional techniques may be better tolerated in the elderly, avoiding the cardiovascular and respiratory depressant effects of general anaesthesia, provided there are no contra-indications. The advantages of regional anaesthesia include reduced blood loss and possibly less thromboembolic events. With regard to TURP, regional techniques also aid the earlier diagnosis of TURP syndrome and bladder perforation. The sympathetic block and vasodilatation caused may reduce the effects of intraoperative fluid overload, although symptoms may then occur as theblock wears off.
Positioning should also be considered as patients with severe cardiac or respiratory disease may not easily tolerate the lithotomy position with slight trendelenburg tilt. Raising the patients head and shoulders may help, and carefully administered sedation may be used. Careful positioning is important as the lithotomy position may result in injuries to the common peroneal, femoral and sciatic nerves.
Some patients may become restless intra-operatively during a regional block. This can be due to many causes which must be considered first as administering sedation in some cases may only serve to increase agitation. Pain may be either due to an inadequate block, or to bladder or rectal perforation. In both cases, additional analgesia and possibly conversion to general anaesthesia will be necessary. Confusion may be the first sign of TURP syndrome. Other early features, such as bradycardia and hypertension followed by hypotension should be sought. Measures should be taken to stop surgery as soon as possible. Patients with underlying cardiac or respiratory problems may develop symptoms such as angina or wheezing and coughing during the operation. These should be treated accordingly.
Contraindications to regional blockades include an unwilling or uncooperative patient (including those with dementia or learning difficulties), infection around the site of needle insertion, raised intracranial pressure, impaired coagulation, fixed cardiac output state (e.g. aortic stenosis). Failure to insert a regional block, which may be more likely in those with anatomical abnormalities of the spine such as scoliosis or ankylosing spondylitis, or inadequate block for surgery after insertion are also indications for general anaesthesia. General anaesthesia may be administered using either spontaneously respiration, or positive pressure ventilation.
The prostate harbours many bacteria, particularly in those with an indwelling urinary catheter. Bacteraemia may occur peri-operatively, but is usually asymptomatic. Septicaemia occurs in up to 7% of patients undergoing TURP. All patients should be given pre-operative antibiotic cover for gram positive and gram negative organisms, such as intravenous gentamicin or oral ciprofloxacin. These may also be used if septicaemia does occur.
Intravenous fluids are usually used, and are essential if regional techniques are given. Normal saline is the most appropriate choice for TURP to decrease any effects of dilutional hyponatreamia. Fluids should be given cautiously as these are usually elderly patients who are more at risk of fluid overload. This is particularly true for those with impaired renal function. It should be remembered that those undergoing a TURP will also absorb irrigation fluid during surgery.
Excessive blood loss is a potential complication for all types prostatic surgery. Methods to reduce this risk should be considered, particularly for radical prostatectomy, or for very large prostates. Isovolaemic haemodilution may be used to reduce the use of allogenic blood. Prostatic tissue contains many alpha receptors, and so alpha adrenergic agonists (eg. Methoxamine) may be used to decrease blood loss.
Thromboprophylaxis should be considered for those undergoing radical prostatectomy, and for any patients who may have difficulty in mobilising post-operatively.
New Techniques
Laser therapy to the prostate produces coagulation and vaporisation of prostatic tissue. Laser prostatectomy involved minimal blood loss and minimal fluid absorption. Its use is increasing in developed countries, particularly for patients considered too ill to undergo TURP. Open prostatectomy may be performed laparoscopically, and both the transperitoneal and extraperitoneal routes may be used.
Summary
The prostate is at risk of either benign or malignant enlargement with increasing age. Many patients present with urinary symptoms and may need surgery. Many different surgical techniques may be used and choice depends on local facilities. The prostate is a very vascular organ and all surgery carries a risk of excessive bleeding. Regional anaesthetic techniques may reduce this risk and also carry other benefits. General anaesthesia may also be used.
Further reading
- Malhotra V and Diwan S. Anesthesia and the Renal and Genitourinary system. In: Miller RD (Ed) Anesthesia. (5th Ed) Chapter 53; pg 1934-1959. Churchill Livingstone, Philadelphia.
- Okeke LI. Day case transurethral prostatectomy in Nigeria. West Afr J Med. 2004; 23:128-30.
- Condie JD Jr, Cutherell L, Mian A. Suprapubic prostatectomy for benign prostatic hyperplasia in rural Asia: 200 consecutive cases. Urology. 1999; 54:1012-6.
- Fichtner J, Mengesha D, Hutschenreiter G, Scherer R. Feasibility of radical perineal prostatectomy under spinal anaesthesia. British Journal of Urology International 2004: 94; 802-4.
- Ahmed AA. Transvesical prostatectomy in Tikkur Anbessa Hospital, Addis Ababa. East Afr Med J. 1992; 69: 378-80.
MCQ Answers
- Question 1
- (a) False (b) False (c) True (d) True (e) False
- (a,b) The incidence of BPH increases with age, but may be treated with drug therapy. (c) There is no good correlation between prostate size and symptoms. (d) Renal impairment may be due to recurrent infections or chronic urinary obstruction. (e) BPH does not spread and is always confined to within the prostatic capsule.
- Question 2
- (a) False (b) True (c) False (d) False (e) False
- (a)TURP is not suitable for very large prostates. (b,d) Electrolyte solutions cannot be used for irrigation as diathermy is used. (c) The patient is placed in the lithotomy position. (e) Bladder perforation is a relatively common complication (about 1%).
- Question 3
- (a) True (b) False (c) True (d) False (e) True
- (a) Glycine is an inhibitory neurotransmitter and may cause CNS symptoms. (b,e) Use of regional anaesthesia may lead to earlier diagnosis, but fluid overload may only present as the block wears off. (d) Irrigating fluid is absorbed through the prostatic venous sinuses.
- Question 4
- (a) True (b) False (c) True (d) False (e) False
- (b,d) Radical prostatectomy is used for malignant disease and may involve major blood loss.
- (c,e) Regional anaesthesia is suitable and may reduce the risk of thromboembolic events.
- Question 5
- (a) True (b) True (c) True (d) True (e) False
- (b) α-adrenergic receptors are abundant in prostatic tissue and so the use of agonists may reduce blood loss. (e) Reducing the height of the irrigating fluid reduces the amount of fluid absorbed, but does not affect blood loss.



