General Topics
KEY POINTS
- Robotic-assisted surgery is now being used in a variety of different surgical specialties including urological surgeries.
- It is associated with a reduction in blood loss, postoperative pain, and hospital stay and also allows for better visualisation of the surgical field when compared to standard laparoscopic surgery.
- Use of a robotic system limits access to the patient intraoperatively, so meticulous anaesthesia planning is essential.
- Pneumoperitoneum and the steep Trendelenburg position used in robotic surgery cause a variety of physiological changes and require special anaesthesia considerations.
INTRODUCTION
The benefits of minimally invasive surgery have led to its increasing use over the last few decades. The most notable of these benefits include smaller surgical incision, reduced pain, reduced blood loss, quicker surgical recovery, and shorter hospital stay. However, these techniques require additional surgical training and there can be complications related to the limited range of instrument motion or access and a suboptimal 2-dimensional view (Table 1).1,2
To counter this, interest has increased in robotic surgical systems. Robots are designed to allow the surgeon to control their instruments from a distance with a higher degree of precision and with better visualisation of tissues than is possible with standard laparoscopic techniques.
The most commonly used system is the da VinciTM surgical robot (Intuitive Surgical, USA) This consists of 3 main components: a master console, a robotic surgical manipulator, and a visualisation tower. Seated in the master console, the surgeon has the ability to control the surgical manipulator (Figure 1). The console allows the surgeon to visualise the surgical field in 3 dimensions, which is not possible with standard laparoscopic procedures. The surgeon has control of 2 actuators that control the robot’s arms and foot pedals to allow control of the camera, instruments, and diathermy.3
With the surgeon in the master console, a surgically scrubbed assistant is still required to insert and change instruments through the endoscopic ports. Communication can be difficult between the members of the team so noise levels in the theatre are kept to a minimum. Microphones within the console and speakers within the video towers are used to enhance the surgeon’s voice.
Despite its costs (approximately £500,000), its large size, and the steep learning curve, there are many advantages to the use of a robotic system. The 3-dimensional image allows the surgeon to appreciate and judge depth in the operative field. The system automatically filters the natural hand tremor of the surgeon and can scale movements for fine precision work. The design of the robotic arm allows for an approximation of a normal human wrist allowing the surgeon to accurately control the arm to reach around and beyond tissues in a manner that could never be achieved using a nonrobotic technique. All these features enable surgery that ultimately results in reduced surgical blood loss and a reduction in pain and shorter hospital stay.3,4
The robotic system has been used in a range of specialist areas, including bariatrics, general surgery, and cardiothoracic and urological surgeries. For this article we will focus on the anaesthetic considerations for robotic-assisted surgery for prostatectomies (RALP) and cystoprostatectomies.
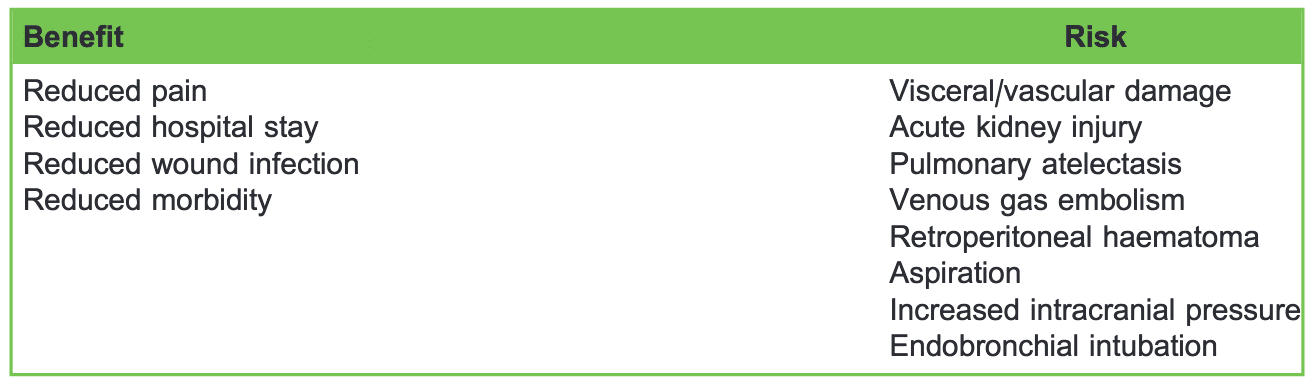
Table 1. Risk and Benefits of Laparoscopic Surgery

Figure 1. Master console where the surgeons are controlling the robotic operating system at a distance from the patient in the theatre. The console can also be used for training purposes.
ROBOTIC UROLOGICAL PROCEDURES AND THE ANAESTHETIST
The issues encountered by the anaesthetist can be divided into anaesthetic, surgical, and patient factors.
Anaesthetic Factors
- Spatial restriction reduces access to the patient.
- Ensuring complete immobility of the patient during the robotic procedure is essential.
- Physiological response to laparoscopic surgery (ie, pneumoperitoneum) must be addressed.
- Pain management is required.
Surgical Factors
- Robotic docking requires the patient to be positioned correctly for accurate use of the robotic arms.
- Bulky robotic arms can cause damage to surrounding structures.
- Major haemorrhage can be insidious.
- Communication can be difficult whilst the surgeon is in the master console.
Patient Factors
- Steep Trendelenburg position for prolonged duration can raise intracranial pressure and cause facial and orbital oedema.
- Risk of regurgitation is increased whilst in the steep Trendelenburg position.
- Risk of renal injury must be evaluated.
These factors can be addressed with a systematic approach to conducting the anaesthetic during the preoperative assessment, intraoperative management, and postoperative period.
PREOPERATIVE
Following a standard assessment, high-risk patients should be identified. Urinary tract infections should be treated preoperatively and a urine dipstick should be performed on admission. The robotic procedure usually requires a steep Trendelenburg position and pneumoperitoneum, which can have potential adverse effects on the patient’s physiology. Absolute contraindications are rare but patient comorbidities such as morbid obesity, severe ischaemic or valvular heart disease, significant respiratory disease, or increased intracranial pressure are considered relative contraindications to using the robotic system and these patients should be considered for open procedures. The additional risk of reduced renal perfusion and injury during the procedure should be considered in those with impaired renal function.
INTRAOPERATIVE
As with any anaesthetic, a systematic approach to patient care should be implemented. Prior to starting any anaesthetic, the World Health Organisation (WHO) surgical safety checklist should be carried out for every patient.
Airway
Endotracheal intubation is mandatory for robotic procedures to protect the airway from the risk of aspiration due to the increased intra-abdominal pressure and steep Trendelenburg position. It also allows for better control of ventilation intraoperatively.
Breathing
The Trendelenburg position combined with the pneumoperitoneum causes diaphragmatic splinting and cephalad movement of the abdominal contents. It can cause endobronchial migration of the endotracheal tube resulting in collapse of the nonventilated lung and hypoxaemia.
Physiologically the positioning combined with a pneumoperitoneum causes a reduction in functional residual capacity and lung compliance. In susceptible patients, this can lead to hypoxia so an appropriate ventilation strategy is required. We recommend the application of positive end-expiratory pressure to prevent atelectasis and achieving tidal volumes of 6 to 8 mL/kg. Pressure controlled ventilation has been found to result in greater dynamic compliance and lower peak inspiratory airway pressure, compared with volume-controlled ventilation.5
Circulation
Large-bore venous access should be secured, as large-scale blood loss can be a rare complicating feature, and fluids should be attached to a fluid warmer. Intravenous access should be secured with extensions prior to starting the procedure as access to the patient is limited during surgery. Urethral catheterisation is a must and a catheter should be inserted prior to the start of the procedure, usually by the urological surgical team.
Full routine monitoring is required and invasive blood pressure monitoring should be used for accurate measurements and to allow monitoring of blood gases and haemoglobin as major blood loss may be insidious. Bradycardia and, potentially, cardiac arrests can occur upon initiating the pneumoperitoneum, so this should be anticipated and any bradycardia should be treated promptly with antimuscarinic drugs such as atropine. Central venous access is not usually required unless patient comorbidities warrant its use.
The cardiovascular system is also affected by patient positioning and the application of a pneumoperitoneum results in an increase in central venous pressure, pulmonary artery pressure, and pulmonary capillary wedge pressure, with a compensatory decrease in heart rate. While the Trendelenburg position increases venous return and may increase cardiac output, the compression of the aorta by the pneumoperitoneum causes an increase in systemic vascular resistance. Cardiac output is therefore reduced due to an increase in systemic vascular resistance and reduction in stroke volume. This leads to an increase in myocardial oxygen demand and therefore caution is needed in patients with a reduced cardiac reservoir or impaired baroreflex (refer to Table 2). In some patients the physiological derangement may be such that it is necessary to convert the procedure to an open approach or abandon it completely.6
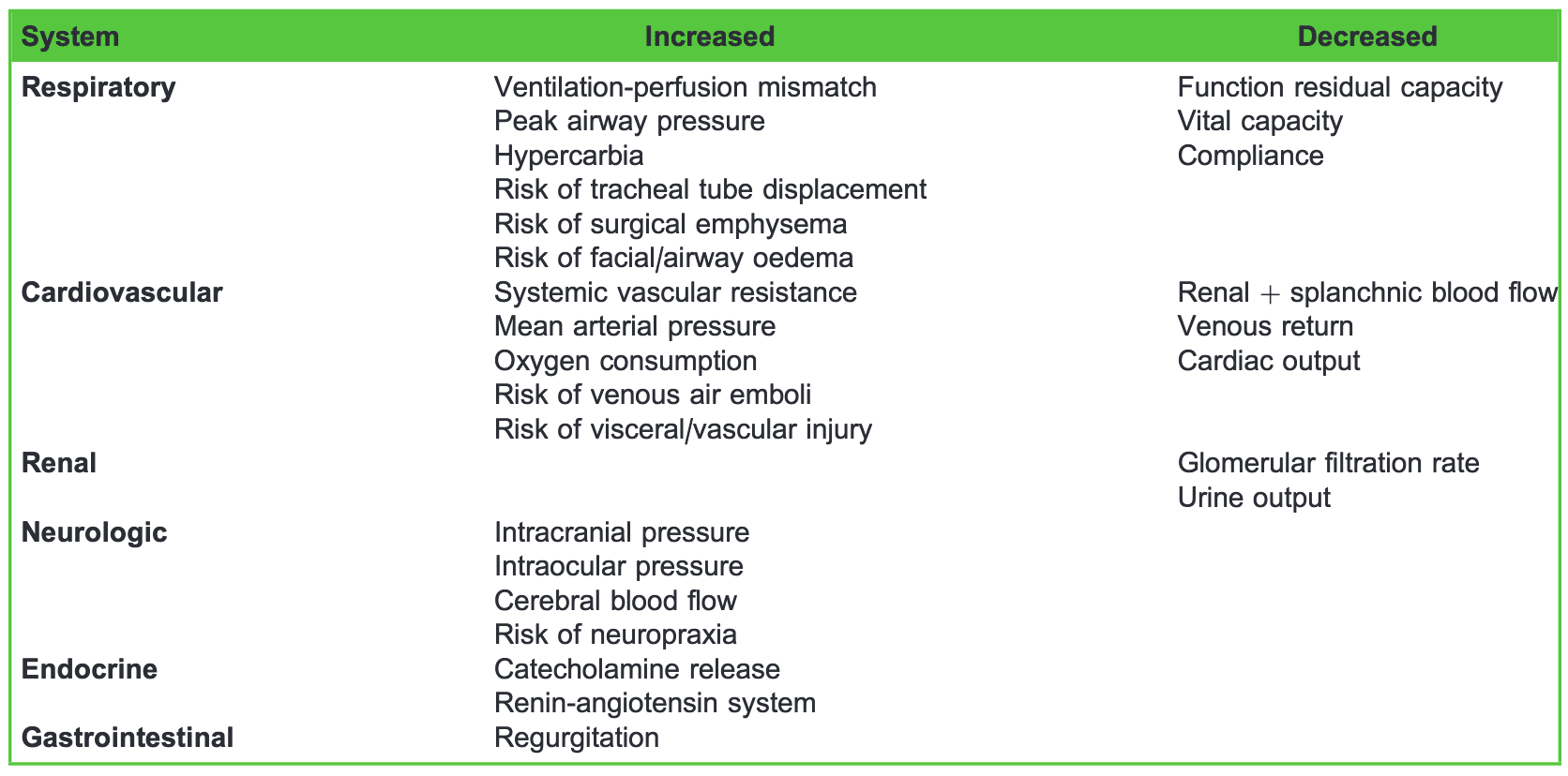
Table 2. Physiological Effects of Pneumoperitoneum
Disability (Maintenance of Anaesthesia and Analgesia)
Intracranial and intraocular pressures are also increased due to reduced venous drainage and steep Trendelenburg position, which may result in decreased cerebral perfusion and facial or orbital oedema. Patients with known increased intraocular or intracranial pressures, such as those with glaucoma or hydrocephalous, should be managed appropriately. These measures may include controlled ventilation to avoid hypercapnia or discussion with surgeon to lower insufflation pressure, or choosing other surgical technique for the procedure.
Suitable anaesthetic maintenance may include volatile agents such as sevoflurane or desflurane, with its rapid recovery profile. However, total intravenous anaesthetic using propofol may be considered as an alternative given its favourable profile in oncological surgery.7
In addition to general anaesthesia, a multimodal approach to analgesia should be implemented. As well as intravenous analgesia, local anaesthetic techniques such as surgical local infiltration, transverse abdominis plane block, or similar techniques should be utilised. Other institutions, such as ours, use techniques such as caudal analgesia immediately postinduction of general anaesthesia to provide effective postoperative pain relief.8
For cystoprostatectomies, epidurals may be utilised and are inserted prior to induction. Epidural analgesia has been found to lower peak inspiratory airway pressure, enhance dynamic compliance, and allow better oxygenation and lower concentrations of lactate. Postoperatively, systemic opioid use is decreased and there is a reduction in gastrointestinal complications such as ileus and constipation. Lower limb venous thrombosis rates are also reduced. However, use of epidurals intraoperatively may result in a high block due to the extremes of positioning and later patient mobilisation may be delayed due to the potential of motor block from epidural blockade.9
Environment (Everything Else)
A nasogastric tube is not essential for RALP procedures but may reduce the risk of gravity-induced passive regurgitation and gastric acid injury to the eyes whilst in steep Trendelenburg position. However, its use in cystoprostatectomies is warranted due to the increased risk of postoperative gastric ileus.10
Vulnerable areas should be adequately padded and limbs should not be positioned at extreme angles. Neurological complications are rare but potentially devastating. Injuries can include brachial plexus injury, especially if shoulder straps are used, and lateral femoral cutaneous neuropathy from the lithotomy position. Prolonged hypotension should also be avoided as it can exacerbate pressure sores and neurological injuries. Corneal abrasions are the most common ocular complication, so eyes should be taped and padded and care should be taken to avoid orbital oedema by potentially restricting intravenous fluids and minimising the Trendelenburg position.11

Figure 2. Patient positioned in steep Trendelenburg position within the anaesthetic room prior to transferring to the theatre. Pressure areas are padded and arms are wrapped with lines outside the padding to prevent sores.
Patient arms should be wrapped snugly to their sides, ensuring that all lines are first padded to prevent pressure injuries. Patients should be placed on a nonslip mat to prevent them sliding down the table during the procedure. Shoulder brace and straps may be required. Antiembolic stockings and intermittent pneumatic compression should be used intraoperatively to prevent deep vein thrombosis. A forced-air warming blanket should be applied.
As a final check of appropriate positioning, the patient should be placed in a steep head-down position prior to docking the robot to confirm that the preparation has been adequate and that the patient is not seen to move during this simulation of surgical positioning (see Figure 2).
In the theatre, the patient is carefully positioned and the robot is wheeled into position between the patient’s legs. The scrubbed assistant places the trocar for the camera via an umbilical incision and induces the pneumoperitoneum. The patient is placed in the lithotomy position with a steep Trendelenburg of up to 30 to 45 degrees, with the steeper position for RALP procedures. The less extreme positioning may offer the best balance between surgical facilitation and physiological compromise of the patient.
After the robot has been docked (see Figure 3), any movement or coughing from the patient could lead to tearing or puncturing of the viscera. For this reason, either meticulous muscle relaxation or remifentanil infusion should be considered, as it is critical for the patient to remain absolutely still. Table position should not be changed until surgical instruments have been disengaged. As discussed earlier, good communication between the theatre staff is vital for good outcomes in patient care. Microphones and speakers within the robotic system allow for the surgeon’s voice to be heard by all members of the team. Those involved with robotic surgeries should be aware of dealing with emergencies such as undocking the robotic arms in a cardiac arrest and these drills may be practiced in simulation scenarios.
Intraoperative fluid should be restricted to reduce facial and airway oedema and urine production, which can impact the surgical field before urethral anastomosis. Hypertension should be managed to help control blood loss and prevent obscuring the visual field. Following the formation of the anastomosis, intravenous fluids can be given as required and analgesia should be given in preparation for extubation.

Figure 3. Robot docked, showing the limited access to the patient. Space within the theatre is also reduced.
POSTOPERATIVE
Upon removal of the robotic arms, any neuromuscular blockade should be reversed. Cerebral and laryngeal oedema should be noted and extubation should only be undertaken if safe to do so, after testing for the presence of a leak with deflation of the endotracheal tube cuff.
Postoperative complications are rare and are normally dictated by the patient’s comorbidities. Patients undergoing cystoprostatectomy should ideally be managed in high-dependency units, or with a similar level of care. The most common surgical complication is a gastric ileus. Delayed return of gastrointestinal motility may result in pain, abdominal distension, nausea, and vomiting and has to be managed immediately to prevent further complications. Management includes gastric decompression via a nasogastric tube, intravenous fluid hydration with electrolyte replacement, and, in a very small number of cases, surgical intervention if abdominal perforation occurs.
Blood transfusion is not normally required as intraoperative blood loss is very low but significant haemorrhage may be insidious and any drain output should be monitored. Intraoperative fluid restriction and reduced renal blood flow due to increased intraabdominal pressures can predispose patients to postoperative renal injury. Patients should therefore receive intravenous fluid hydration overnight and be monitored for haemorrhage and deteriorating renal function during the postoperative period.
Pain is comparable to conventional laparoscopic surgery but deep pelvic pain remains an issue. Multimodal analgesia (utilising the WHO step ladder) should be administered. Nonsteroidal anti-inflammatory drugs are usually avoided due to the risk of postoperative renal injury. A small percentage of patients require opioids. The use of regional anaesthesia such as spinal or caudal analgesia for RALP patients has led to less systemic opioid use postoperatively.
There have been reports of ischaemia-induced lower limb compartment syndrome after prolonged lithotomy due to decreased blood pressure and flow. This warrants the need to assess the compartments postoperatively and prevent intraoperative hypotension.3
Low-molecular-weight heparin should be administered as the patients are considered at higher risk for postoperative thromboembolic events.
Surgical drains, nasogastric tubes, and urinary catheters should be removed after review by the surgical team. Oral analgesia should be initiated as soon as the enteral route is available and analgesia from epidurals, if used, is no longer required. It is vital that patients have opened their bowels and this should be monitored. Laxatives may be required upon advice from the surgical team. Patients should be encouraged to mobilise as soon as possible to enhance their recovery and potentiate a safer discharge from the hospital.
SUMMARY
- Robotic-assisted surgery involves the surgeon operating through a console distant from the patient with a scrubbed assistant by the patient.
- It is associated with reduced blood loss and pain, and a reduction in hospital stay.
- Pneumoperitoneum and a steep Trendelenburg position can cause various complications, which can be prevented through meticulous anaesthesia perioperatively and improved surgical technique.
- Good communication between the theatre staff is vital for good outcomes in patient care; for example, use of practice drills, such as that for efficient undocking of the robot in an emergency, is important.
- Multimodal analgesia is required for postoperative pain management.
REFERENCES
- Lee J. Anesthetic considerations for robotic surgery. Korean J Anesthesiol. 2014;66(1):3-11.
- Hayden P, Cowman S. Anaesthesia for laparoscopic surgery. Cont Educ Anaesth Crit Care Pain. 2011;11(5):177-180.
- Irvine M, Patil V. Anaesthesia for robot-assisted laparoscopic surgery. Cont Educ Anaesth Crit Care Pain. 2009;9(4):125-129.
- Danic M, Chow M, Alexander G, et al. Anesthesia considerations for robotic-assisted laparoscopic prostatectomy: a review of 1,500 cases. J Robot Surg. 2007;1(2):119-123.
- Choi EM, Na S, Choi SH, et al. Comparison of volume-controlled and pressure-controlled ventilation in steep Trendelenburg position for robot-assisted laparoscopic radical prostatectomy. J Clin Anesth. 2011;23:183-188.
- Naylor JM, Chow CM, McLean AS, et al. Cardiovascular responses to short-term head-down positioning in healthy young and older adults. Physiother Res Int. 2005;10(1):32-47.
- Wigmore T, Mohammed K, Jhanji S. Long-term survival for patients undergoing volatile versus IV anesthesia for cancer surgery: a retrospective analysis. Anesthesiology. 2016;124(1):69-79.
- Kao S, Lin C. Caudal epidural block: an updated review of anatomy and techniques. BioMed Res Int. 2017. doi: 10.1155/ 2017/92171459.
- Nimmo S, Harrington L. What is the role of epidural analgesia in abdominal surgery? Cont Educ Anaesth Crit Care Pain. 2014;14(5):224-229.
- Chang SS, Baumgartner RG, Wells N, et al. Causes of increased hospital stay after radical cystectomy in a clinical pathway setting. J Urol. 2002;167(1):208-211.
- Maerz DA, Beck LN, Sim AJ, et al. Complications of robotic-assisted laparoscopic surgery distant from the surgical site. Br J Anaesth. 2017;118(4):492-503.



