General Topics
QUESTIONS
Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation.
- Concerning Special Care Dentistry:
a. Patients always require a general anaesthetic
b. The majority of work is performed in the day-case setting
c. When a patient lacks capacity and has no next of kin, the dentist acts in best interests
d. Special care dentistry includes patients with a phobia of dentistry - Premedication:
a. Intra-muscular ketamine is preferably avoided
b. Midazolam is the favoured sedative premedication
c. Effects of sedative medication are predictable in this group
d. When premedicating patients with sedatives, deep sedation should be the target for compliance with induction of anaesthesia - Intraoperative considerations:
a. A MAC of > 1.5 is advisable intraoperatively
b. Suctioning of the oropharynx under direct vision is recommended prior to emergence
c. Patients usually require opiates intraoperatively
d. Use of the WHO checklist is not required for dental surgery - Post operative care:
a. Use of a bite block is recommended with both a laryngeal mask and endotracheal tube
b. Provision for overnight stay must be available
c. Carers must be provided with written and verbal post operative instructions and contact numbers in the event of complication
d. Intravenous cannulae should be removed prior to discharge to recovery as patients may find this distressing
INTRODUCTION
Disability is known to disadvantage patients, particularly adults, in accessing health care and is associated with poorer health outcomes than the rest of the population [1]. Its prevalence is not accurately known, in part due to the subjective nature of reporting disability, but it is thought that around 15% of the working-age population in Europe are limited in their daily activities by physical or mental health problems, illness or disability [2]. Within the World Health Organisation’s International Classification of Functioning, Disability and Health [3], people requiring Special Care Dentistry (SCD) are those with a disability or activity restriction that directly or indirectly affects their oral health.
SCD includes oral care for adults who require a general anaesthetic (GA) for dental treatment. Many of these patients are vulnerable adults, who are not able to independently access and consent to dental treatment. SCD is concerned with the provision and delivery of oral care for people with an impairment or disability defined in the broadest of terms [4]:
“The improvement of oral health of individuals and groups in society, who have a physical, sensory, intellectual, mental, medical, emotional or social impairment or disability or, more often, a combination of these factors”
The medical, social, physical and mental needs of individuals who benefit from SCD vary widely. The community dentist may be able to meet some of these. For others, a more comprehensive and holistic approach is required when planning and conducting dental care. This group includes those living at home, in residential care, in mental health units and the homeless.
A robust multi-disciplinary approach is needed when evaluating the risk versus benefit of proceeding with GA for delivery of dental treatment. In order to comprehensively plan these cases, it is important to consider factors that apply to all dentistry under GA, such as the implications of a shared airway. Additional factors that are particularly relevant for this group of patients are the specific issues of capacity assessment and consent, as well as a thorough understanding of the individual’s medical, social and behavioural issues.
This paper includes a discussion on the practical considerations and requirements for the delivery of GA for special care patients and explores the perioperative management strategies for this patient group.
DIVERSE PATIENT GROUP
The patient group accessing SCD is a diverse one. Examples of patients who may not comply with dental treatment in the dental chair and may require GA include:
- Patients with severe learning difficulties
- Patients with anxiety and phobias
- Patients with severe psychiatric disorders
- Patients with physical disability and movement disorders
- Patients with significant co-morbidity, such as those with congenital disorders, in whom sedation may not be safe and perioperative monitoring is required
PRACTICAL CONSIDERATIONS
Planning visits for pre-assessment and for surgery itself present some practical challenges:
- Hospital transport to and from the hospital may be required.
- The location must allow access for wheelchairs and use of equipment such as hoists.
- The location should also have adequate space for escorts to be present.
- Ideally, additional services such as radiology, phlebotomy and electrocardiogram (ECG) should be in close proximity.
- Adequate time should be available due to the higher case mix complexity and potential challenges in acquiring information.
- Education and training in the welfare of vulnerable adults is required for all staff involved in the patient’s pathway.
- Appointment of a lead consultant anaesthetist, with experience in Special Care Dentistry promotes good liaison with the dentist and development of an effective service.
- The anaesthetist should be present at the dental pre-assessment clinic so that an appropriate risk assessment can be undertaken and care appropriately planned.
- The majority of work is performed as day-case surgery. A minority of patients will require an in-patient stay due to pre-existing medical conditions. Although unplanned overnight admissions (due to complications of surgery or anaesthesia) are unusual, provision for this should be available in a hospital setting with overnight facilities.
- The patient pathway may be prolonged due to issues with consent and the need to seek additional information from other clinicians, old medical records or investigations.
PRE-ASSESSMENT CLINIC
Pre-operative assessment by the anaesthetist who will be conducting anaesthesia is an important requirement to plan appropriate care. This may also reduce cancellations on the day. The following factors need to be considered:
History
A sensitive approach, checking the patient’s level of communication, understanding and mobility is imperative.
History should include evaluation of general medical health, including a detailed drug history, and details of chronic conditions such as epilepsy, and recent illness. Anticipation of communication needs prior to the preoperative visit is helpful and may require the use of aids such as Makaton, visual aids and voice boxes.
Information may not always be easily available from the patient. Collateral history from carers or relatives may be required. This can subsequently be supplemented by requests for information from other health professionals involved in the patient’s care. Information regarding previous GAs should specifically be sought.
Information regarding social circumstances and any behavioural issues is essential in planning care. This allows factors such as appropriate escorts and overnight care to be addressed.
Consideration should be given to performing additional procedures or investigations that may be required by other specialties during the same GA. Examples of these include podiatry, ENT assessment / treatment and blood tests.
Examination
Examination should be performed as permitted by the patient and often may be poorly tolerated. If formal examination is not possible, the patient’s response to strangers and physical contact such as handholding is one of the most valuable aspects of determining future anaesthetic care. This allows the anaesthetist to gauge the level of cooperation and compliance, which in turn determines the need for a sedative premedication.
Basic observations, airway assessment (as tolerated) and an assessment of ease of venous access are important. A formal (or estimate) of height and weight measurement is helpful.
Limited patient cooperation may also limit the dentist’s ability to undertake an oral examination. The dentist may not be able to identify the specific dental treatment needs until the patient is actually anaesthetised.
Investigations
Patients may be unable to cooperate with investigations. Preoperative tests such as ECG, echocardiogram and venepuncture may be impossible. A pragmatic approach from the anaesthetist works best, as it is not always possible to undertake all indicated tests.
Screening for MRSA (methicillin resistant staphylococcus aureus) colonisation should be carried out in accordance with local guidelines, given the higher incidence of infection in residential care. If testing is not possible, one should consider managing the patient as if they are MRSA positive.
As many patients are unable to communicate any physical symptoms that they experience, it is important to have a low threshold for screening investigations, specifically blood tests including full blood count, renal function and thyroid function. Polypharmacy is also an issue for many SCD patients so drug levels for anti-epileptic medication and lithium should be monitored where appropriate.
Consent
The best interests of the patient must remain at the forefront of decision-making processes.
The dentist responsible for the patient’s oral heath must make a balanced judgment on the treatment best suiting the patient, taking into account their behavioural capabilities, cognitive function and general health. This will be done in partnership with the patient (if possible) and the next of kin or guardian of the patient.
It is important that the dentist is able to convey an estimation of the extent of anticipated treatment and its chance of success. In those instances when a patient lacks capacity and does not have a next of kin, appropriate local procedures must be followed. In the UK, an IMCA (independent mental care advocate) must be appointed in accordance with the Mental Health Act [5]. When general anaesthesia is planned, both dentist and anaesthetist should be involved in the consent process to determine the risks and benefits of treatment.
Written instructions
Written and verbal information is imperative as the patient may have a varied number of carers who may need to refer to this information.
Instructions for patients and carers (both verbal and written) should include the following:
- Preoperative fasting advice
- Premedication anticipated (anxiolysis, antacids, sedatives)
- Advice on which routine medications should be taken/omitted on the day of surgery
- Arrival times in designated areas
- Transport/Escort
- Parking facilities
- Overnight bag with clothing and medication in the event of unplanned overnight stay
- Advice on postoperative recovery, analgesia and establishment of routine diet and medications
- Contact numbers for surgical and anaesthesia related-questions and management of complications.
ON THE DAY OF SURGERY
Premedication
The anaesthetist should meet with the patient and carer/relative on the day of surgery and prescribe relevant premedication. Sedative premedication is commonly use in this population. It is worth remembering that these patients often require multiple general anaesthetics throughout their lifetime for both dental care and other medical interventions. As such, it is important to lay down good experiences of anaesthesia for the patient, promoting compliance in the future.
Minimal (anxiolysis) to moderate (conscious) sedation should be the target for compliance with induction of anaesthesia, where patients are able to respond purposefully to verbal commands or light tactile stimulus. Maintenance of own airway and adequate ventilation are clearly imperative preoperatively, when the level of clinical supervision and the environment are unsafe for deeper planes of sedation and the dangerous consequences of respiratory depression.
The effects of sedative medication may be variable and patients may already take a number of medications with depressant effects on CNS activity. Our experience is that doses smaller than those typically advocated by most formularies are often successful for premedication and improved compliance at induction. Ideally, the anaesthetist conducting the list should be present, or nearby, to observe the effects of sedation.
Patients may refuse to consume all or some of the dose prescribed, in which case alternative strategies or routes of administration need consideration. Unpleasant tastes can be masked with the use of limited amounts of sweet drinks. Surgery is rarely stimulating as the dentist is able to provide an adequate field of anaesthesia with local anaesthetic administration. Therefore, sedatives with prolonged half-lives and systemic effects likely to delay discharge should be avoided.
Midazolam is most commonly prescribed as an oral preparation (0.1-0.4 mg/kg) and an incremental dosing strategy can be more effective in titrating to effect. This dose is smaller than that with which many anaesthetists are familiar, but our experience is that patients typically require a lower total dose. This population may be more sensitive to the respiratory depressant effects of benzodiazepines, and in addition, polypharmacy with agents such as antiepileptics and sedative drugs, may contribute to oversedation, and less predictable effects than seen in the general population. After review by the anaesthetist a second dose of midazolam may on occasion be required, (not exceeding the total dosing range described above). Sedation may be inadequate, or the patient may have been poorly compliant with accepting the whole amount originally prescribed. This titrating policy avoids the potentially harmful effects of over-sedation in this population. Should the patient be unwilling to take oral medication, other routes of administration may be sought, namely the intranasal route for midazolam (0.05-0.2 mg/kg) or intranasal ketamine (3-5mg/kg). Only as a last resort (in our experience) should intramuscular ketamine (1-2 mg/kg) be used and extra restraint may be required to administer sedation by this route. Emphasis should always be placed on a sympathetic and non-threatening approach. If tolerated, topical local anaesthetic cream (EMLA or Ametop) is applied in preparation for obtaining venous access.
Intranasal midazolam
The intranasal route of administration of midazolam is a useful alternative when oral premedication is not accepted or is insufficient. A carer or family member may be able to administer the intranasal midazolam, with the avoidance of distress that may be precipitated with intramuscular routes. A mucosal atomisation device (MAD) fitted to the hub of a syringe provides good aerosolisation of drug to the nasal mucosa. The addition of lignocaine to midazolam for atomisation by the intranasal route has been shown to reduce the stinging effect [6].
An understanding of the differences in pharmacokinetics and pharmacodynamics of midazolam given intranasally is important, as this will affect timing of administration and dosing. The bioavailability of intranasal midazolam is approximately 70% [7]. Intranasal midazolam reaches plasma concentrations sufficient for conscious sedation rapidly. Authors studying the pharmacokinetic profile of intranasal midazolam in adults showed that maximal blood concentrations are achieved twenty-five minutes (mean) after intranasal midazolam (0.25mg/kg), though time to reach a threshold adequate for conscious sedation was significantly shorter, and closer to ten minutes [8].
A large multi-centre audit conducted in the United Kingdom demonstrated good levels of compliance in adults with learning disability who were unable to accept intravenous cannulation or inhalational sedation [9]. Intra-nasal midazolam (4-15mg range), followed by intravenous cannulation and incremental doses of IV midazolam as required, provided adequate conditions for dental treatment in 91.4% (n=203) of this group. Just 8.5% (n=19) were unable to tolerate treatment with this strategy of sedation. One patient required supplemental oxygen to correct an episode of desaturation.
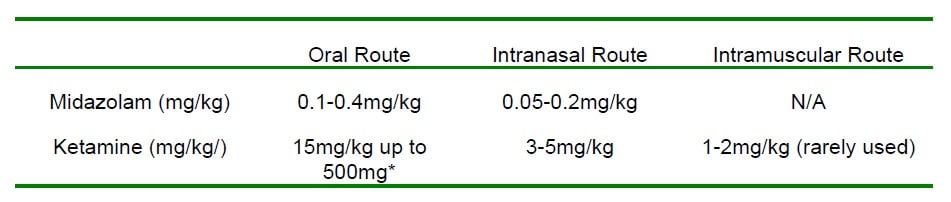
Table 1. Table showing dosage ranges for midazolam and ketamine given as premedication prior to GA in special care dentistry patients.
* Should be given in conjunction with midazolam to reduce ketamine side effects.
NB Whilst other drugs including barbiturates and clonidine, with sedative and analgesic effects are used in paediatric anaesthesia, we have not found these necessary for anaesthesia in special care dentistry. The prolonged side-effect profile of many of these drugs do not make them a favourable choice in the day-case setting for SCD, where local anaesthetics with simple analgesics form the mainstay of pain relief.
The anaesthetic plan will be re-visited on the day of surgery with the patient and carer, mindful of a degree of flexibility that needs to be in-built to this plan. The decision as to whether induction of anaesthesia is intravenous or inhalational will depend on a number of factors and, as with paediatric anaesthesia, the plan will remain dynamic, assessing which is likely to be better tolerated by the patient.
Induction
Induction via inhalational or intravenous routes is conducted, ideally in the presence of carer/guardian and dentist, who may be able to offer support and assistance. Emphasis on preparation of drugs and equipment cannot be over-stressed. A sensitive approach to the needs of the patient is important in preparing the anaesthetic room. Reducing potential stressors may be helpful. This may include removing needles from sight and dimming ambient lights, especially if the patient is lightly sedated and may waken on transfer to a brightly lit anaesthetic room. These patients may be able to undergo inhalational induction without being woken. Any intervention with clinical holding at induction of anaesthesia must be in accordance with local legislation on consent and intervention and should have been discussed with the next of kin and carer at the preoperative assessment.
In suitable cases, allowing a patient to hold their own mask (or even administer their own IV medication) can make the process more tolerable for them.
Clinical Holding
Clinical holding in SCD may on occasion be necessary in order to provide safe care for the patient.
The British Society for Disability and Oral Health has developed this term and its associated guidelines [10] in order to prevent abuse and safeguard vulnerable adults. It is defined as:
‘The use of physical holds (clinical holding), to assist or support a patient to receive clinical dental care or treatment in situations where their behaviour may limit the ability of the dental team to effectively deliver treatment, or where the patient’s behaviour may present a safety risk to themselves, members of the dental team or other accompanying persons’
Clinical holding should be avoided in all but the most challenging of behaviours. Its use should be communicated to a patient’s relatives and carers in anticipation of such a requirement, as well as to all members of the team involved in the patient’s care. Every effort should always be made to preserve patient dignity and safeguard their best interests.
POINTS TO CONSIDER FOR DENTAL ANAESTHESIA
- Shared airway
- Nasal tube commonly required
- Throat pack
- Vasoconstrictor (e.g. Co-phenylcaine)
- Eye care (lubricant/padding)
- Risk of laryngospasm
- Analgesia
- PONV
Airway Management
A nasal tube provides the best surgical field for the dentist and this is the most frequent airway used. On occasion the dentist may request that a particular nostril is used in order to improve surgical access and intra-oral imaging.
A vasoconstrictor, such as co-phenylcaine should be used to reduce the risk of trauma and epistaxis. Carer and patient should be warned, at the preoperative visit, of the possibility of sore throat and nosebleed. A thorough airway assessment may not have been possible preoperatively and as such the anaesthetist should adopt a low threshold for preparing additional equipment, such as a fibreoptic scope, video-laryngoscope and laryngeal mask airways in the event of encountering difficulties. If a laryngeal mask is used, the flexible variety is preferable as the tube may be positioned away from the surgical field, whilst maintaining a good seal for adequate ventilation.
Discuss your airway management plan with the dentist, who may have access difficulties with a laryngeal mask in-situ and may wish the device to be secured in a specific way to optimise the surgical field. It is very important to continue to assess the adequacy of ventilation after repositioning on the operating table and following commencement of the case, as a laryngeal mask can become displaced with manipulation of the airway or during transfers.
A throat pack may be used and its insertion highlighted to the theatre staff.
The anaesthetist should be aware of congenital syndromes with recognized difficult airways, e.g. Treacher Collins and Cornelia de Lange Syndrome, and plan accordingly, with a back-up plan should the initial plan fail. The Difficult Airway Society (DAS) has established algorithms to follow in the event of unanticipated difficult airway [11].
Both the anaesthetist and the dentist must be aware of poor or loose dentition with the inherent risk of tooth dislodgment.
Monitoring
Following induction, standard monitoring should be maintained throughout. Full monitoring may not be practical for induction and a saturation probe will suffice in most cases. In our experience, the use of depth of anaesthesia monitoring is helpful and often allows the anaesthetist to be conservative with intra-operative anaesthesia. A MAC of 0.5 is often adequate in pre-medicated patients as the local anaesthetic used by the dentist means that the surgery involves minimal stimulation.
Maintenance of Anaesthesia
Maintenance of anaesthesia should reflect the day-case setting, avoiding agents that may contribute to post-operative nausea and vomiting (PONV) and respiratory depression. Sevoflurane and desflurane are first line volatile agents and a total intravenous anaesthesia technique with propofol may also help to reduce PONV.
Administration of two antiemetic agents, ondansetron and dexamethasone (0.1mg/kg) may mitigate the need to administer further antiemetic agents in recovery. Antimicrobial and thromboembolic prophylaxis may be indicated, depending on trust policy and the needs of the patient, and should be discussed prior to surgery and addressed at the time of the WHO checklist sign in.
Analgesia
Simple analgesia with paracetamol and a non-steroidal analgesic is usually adequate for dental procedures. The dentist will infiltrate with local anaesthetic prior to commencement of surgery and a long acting local anaesthetic is often used at the end of surgery when dental extractions have been undertaken. Should opioids be deemed necessary, short-acting drugs should be chosen that will not delay discharge with prolonged sedative and respiratory depressant effects.
Positioning
Care and attention must be paid when positioning patients for surgery. This group may be more likely to have pre-existing fixed flexion deformities and are vulnerable to pressure-related injuries. Protection of the eyes during surgery is the responsibility of the anaesthetist and is of particular importance during shared airway cases, when the operative field is in close proximity.
Types of dental procedures
A large and varied number of procedures are performed under general anaesthesia and will vary from patient to patient. As discussed previously, in some patients in whom it is in their best interests to avoid multiple general anaesthetics, extractions may be favoured over restorative work with poor chances of success and maintenance of good dental hygiene. This will have been discussed with the patient and carer and reiterated explicitly at the time of consent.
The dentist in some instances may opt to leave the theatre, once an assessment has been made under general anaesthetic, to discuss with the relative or carer the extent of disease, and planned treatment. This approach promotes a good working relationship between dentist and next of kin, especially when extractions are recommended.
Typical procedures include thorough examination of teeth, dental hygiene and periodontal treatment (scaling) and performing radiographs to assess extent of dental disease. Interventions include restorative work to damaged teeth, filling dental caries and extractions.
Emergence and extubation
Important points to consider in the shared airway are the increased likelihood of blood and debris in the oropharynx and hypopharynx. If not suctioned carefully this can cause laryngospasm, airway obstruction, aspiration and swallowed blood, stimulating vomiting. Under direct vision with a laryngoscope, suction the oropharynx with care. The dentist may have left dental packs in situ and clear communication must be made regarding packs and specifically the removal of the throat pack. Ensure neuromuscular blockade is antagonised.
The decision as to whether to extubate awake or deep will depend on the skills and experience of the anaesthetist and on patient characteristics. Nasal tubes are usually well tolerated and awake extubation is unlikely to precipitate excessive coughing and increases in venous pressure, which can cause bleeding. A deep extubation, exchanging the endotracheal tube for a laryngeal mask or oropharyngeal airway, provides good airway conditions for smooth emergence. Always use a bite block with the laryngeal mask to avoid biting down on the tube, precipitating occlusion of the tube and airway obstruction. The caveat to deep extubation must always be that the anaesthetist is immediately available to deal with any airway complications should they occur during emergence and should not begin the next case alone.
POSTOPERATIVE MANAGEMENT
Recovery
Once dental treatment has been completed and vigilant attention paid to the (documented) removal of any throat pack followed by suctioning under direct vision of the oropharynx, the patient may be safely extubated. As with all shared airway cases, the risk of laryngospasm is higher [12] and the anaesthetist needs to be mindful of this. Do not commence another case until you are satisfied that protective reflexes are fully recovered. The presence of a carer or guardian in the recovery room will provide reassurance to the patient and this should be encouraged as soon as it is safe to do so.
Recovery staff should be informed of the patient’s usual level of communication and receive a full handover from the anaesthetist. This should include any limitations on movement as well as handling and positioning advice. If challenging or aggressive behaviour is anticipated, this should be addressed. Pre-emptively bandaging the cannula prior to the patient waking fully avoids distress and accidental decannulation.
Analgesia
Simple analgesia should be prescribed for the patient to go home with.
Safe discharge
All patients should be seen and reviewed by the anaesthetist and dentist prior to discharge. The majority of patients will fulfil discharge criteria for safe discharge home on the same day, though a small proportion will require overnight stay, be it planned or unplanned. The dentist and anaesthetist will need to arrange surgical cover overnight and liaise with medical and psychiatric teams accordingly if their input and expertise is required.
Carers should be given both written and verbal instructions for postoperative care, including analgesia as well as advice on resuming usual medications and diet. Contact information, including 24-hour emergency telephone numbers, must be provided in the event of concerns or complications. Discharge documentation should accompany the patient home in addition to being sent to the patient’s own general practitioner.
Although many of these patients live in sheltered or residential care, these facilities are unlikely to have medical provision and it is important not to make such an assumption. Check the level of supervision that the patient usually receives and ensure that a competent adult will accompany the patient overnight, following general anaesthesia.
SUMMARY
Adults with disability and special needs commonly encounter barriers in accessing healthcare. The provision of a specialty branch of dentistry dedicated to these patients’ needs reduces these inequalities. General anaesthesia for dental procedures forms an important part of special care dentistry and demands a close working relationship between dentist, anaesthetist and other multi-disciplinary teams involved in these patients care.
Establishing a successful special care dentistry anaesthetic service in hospitals requires an understanding of specific perioperative challenges in this group as well as experience in the management of shared airways, implications of consent for adults who lack capacity and a sympathetic and pragmatic approach in partnership with patient and carer.
PRACTICAL TIPS FOR ANAESTHESIA FOR SPECIAL CARE DENTISTRY
Preoperative care
- Engage with the primary caregiver on communication needs and behavioural characteristics of your patient.
- Have a low threshold for requesting old notes and new investigations. Patients frequently have many co-morbidities
- Review and assess adequacy of sedation before induction
- Addition of lidocaine to intranasal midazolam reduces pain on administration
Intraoperative care
- Encourage support of carer and dentist in anaesthetic room for induction
- Conceal sharps and equipment that the patient may find distressing
- Patient may prefer not to wear a hospital gown and prefer to remain in their own clothes for induction
- Tolerate minimal monitoring for induction – even Sp02 monitoring may not be tolerated
- Addition of lidocaine to propofol for intravenous induction reduces pain on injection
Postoperative Care
- Give recovery staff a thorough handover of clinical interventions and describe communication needs and behaviours
- Encourage carer into recovery area
- Bandage cannula prior to emergence
Planning Safe Discharge
- Always review your patient before discharge home
- Ensure written and verbal instructions for aftercare are provided and 24-hour telephone contact numbers, in the event of emergency
ANSWERS TO QUESTIONS
- FTFT
SCD provides for a wide variety of patients who are unable to accept routine dental care because of physical, intellectual, medical, emotional, sensory, mental or social impairment, or a combination of these factors. A general anaesthetic is not always warranted, though patients are likely to have failed treatment in the community and require specialist multi-disciplinary input in their care. In those instances when a patient lacks capacity and does not have a next of kin, an IMCA (independent mental care advocate) needs to be appointed in accordance with the Mental Health Act. - TTFF
Minimal (anxiolysis) to moderate (conscious) sedation should be the target for compliance with induction of anaesthesia. Midazolam (oral or intranasal routes) provides safe and effective conscious sedation in patients and is the most commonly used sedative premedication in SCD. Effects of sedative premedication are less predictable in this group and it may be more difficult to judge the level of sedation in patients who are unable to respond well to verbal communication. Patients’ usual level of communication should be maintained for conscious sedation techniques. - FTFF
Opiates are very rarely required intraoperatively. Surgery is minimally stimulating, reducing requirement for MAC and opiates. Local anaesthetic infiltration is almost always performed by the dentist prior to commencing treatment. - TTTF
Intravenous cannulae should be left in situ until the patient is fully recovered. Information regarding aftercare arrangements and emergency contacts must always be provided to carer and next of kin.
REFERENCES and FURTHER READING
- WHO World Report on Disability 2011.
http://www.who.int/disabilities/world_report/2011/en/index.html accessed 5th October 2012 - European Foundation for the Improvement of Living and Working Conditions Illness, Disability and Social Inclusion Luxembourg: Office for Official Publications of the European Communities 2003. http://www.eurofound.europa.eu/pubdocs/2003/35/en/1/ef0335en.pdf accessed 5th October 2012
- World Health Organisation’s International Classification of Functioning, Disability and Health http://www.who.int/classifications/icf/en/ accessed 5th October 2012
- Joint Advisory Committee for Special Care Dentistry (2003a) Training in Special Care Dentistry; London JACSCD.
- The Mental Capacity Act HMSO, 2005
- Chiaretti A, Barone G, Rigante D, Ruggiero A. Intranasal lidocaine and midazolam for procedural sedation in children. Arch Dis Child 2011;96 (2):160-3
- Wermeling D, Record K, Archer S, Rudy A. Pharmacokinetics and pharmacodynamics of a new intranasal midazolam formulation. Anesth Anal 2006; 103:344-349
- Burstein AH, Modica R, Hatton M, Forrest A, Gengo F. Pharmacokinetics and pharmacodynamics of midazolam after intranasal administration. J Clin Pharmacol 1997;37:711-718
- Manley M, Ransford N, Lewis D, Thompson S, Forbes M. Retrospective audit of the efficacy and safety of the combined intranasal/intravenous midazolam sedation technique for the dental treatment of adults with learning disability. British Dental Journal 2008;205: E3
- http://www.bsdh.org.uk/guidelines/BSDH_Clinical_Holding_Guideline_Jan_2010.pdf Accessed
5th October 2012 - Henderson JJ, Popat MT, Latto IP, Pearce AC. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia 2004; 59: 675-94
- Visvanathan T, Kluger M, Webb R, Westhorpe R. Crisis management during anaesthesia: laryngospasm. Qual Saf Health Care 2005; 14:e3



