General Topics
QUESTIONS
Before reading the tutorial try answering the following questions. Answers can be found at the end of the text.
- Hyperthyroidism
- Can be identified by high levels T3/T4 and Thyroid Stimulating Hormone (TSH)
- Is most commonly caused by Graves disease
- Patients are prone to exaggerated hypotensive response during induction of anaesthesia
- Increases Minimum Alveolar Concentration (MAC) values
- Thyroid surgery is usually first line treatment
- Regarding superficial cervical plexus block
- C1-5 anterior primary rami form the cervical plexus
- Block can be achieved with infiltration along the posterior border of Sternocleidomastoid
- Phrenic nerve palsy is a common complication
- Could be used as a sole anaesthetic technique in a patient with a retrosternal goitre
- Can reduce postoperative morphine requirements.
- Hypocalcaemia
- Should be diagnosed by total body calcium levels
- Can cause paraesthesiae
- Is indicated by Trousseau’s sign
- Can potentiate the negative inotropic effects of volatile anaesthetics
- Reliably prolongs non-depolarising neuromuscular blocking agents
INTRODUCTION
Thyroid surgery can range from simple removal of a thyroid nodule to highly complex surgery. The presence of longstanding or large goitres can pose difficult airway management decisions whilst endocrine imbalance can have can have profound systemic manifestations that need to be considered and controlled perioperatively.
This tutorial presents some of the more common thyroid pathologies that may be encountered, reviews the anaesthetic management of thyroid surgery plus looks at some of the common postoperative complications.
THYROID PATHOLOGY AND INDICATIONS FOR SURGERY
There are many indications for thyroid surgery, including: thyroid malignancy, goitres that produce obstructive symptoms and/or are retrosternal; hyperthyroidism resistant to medical management; cosmetic and anxiety related reasons. Patients with hypothyroidism usually respond to thyroxine therapy and surgery is rarely indicated.
Hyperthyroidism
Hyperthyroidism results from excess circulating T3 and T4. The vast majority of cases are caused by intrinsic thyroid disease. Indications for surgery include:
- Grave’s disease: An autoimmune condition associated with diffuse enlargement and increased vascularity of the gland caused by IgG antibodies mimicking Thyroid Stimulating Hormone (TSH). It is the only cause of hyperthyroidism associated with eye signs and pretibial myxoedema. It can be associated with other autoimmune conditions.
- Thyroid secreting adenomas often presenting as a solitary nodule.
- Toxic Multinodular Goitre. More common in women; a goitre develops one or two nodules with hypersecretory activity.
- Other causes that may or may not be associated with goitre include: Exogenous iodine, Amiodarone, Post irradiation thyroiditis. In this group, medical management has proved unsatisfactory and radioiodine is not suitable.
Hypothyroidism
May be from intrinsic thyroid disease or failure of the hypothalamo-pituitary axis. Those associated with goitre include:
- Hashimoto’s thyroiditis. This is the commonest cause of hypothyroidism and although initially may cause gland enlargement will later lead to thyroid atrophy due to autoantibody destruction of the follicles.
- Iodine deficiency. A lack of iodine leads to thyroid hormone depletion, Thyroid Stimulating Hormone (TSH) stimulation and gland hypertrophy. Dietary iodine deficiency can be found in mountainous areas.
Malignancy
These will most commonly present as thyroid nodules and are usually minimally active hormonally (patient is euthyroid). The most common types are Papillary and Follicular carcinomas arising from the epithelium that confer a good prognosis if confined to the gland. Medullary carcinomas arising from calcitonin producing cells are associated with Multiple Endocrine Neoplasia II (MEN), which may be linked with phaeochromocytoma and primary hyperparathyroidism. Lymphomas cause diffuse swelling of the gland and carry a very poor prognosis.
ANAESTHETIC CONSIDERATIONS
It is fundamental to ensure that patients are clinically and chemically euthyroid prior to embarking on elective thyroid surgery. Although the majority of cases may be straightforward the possibility of both expected and unexpected challenging airway situations should be anticipated.
Preoperative Assessment
History
This should be focused on establishing if the patient is clinically euthyroid and assessing for airway compromise. The symptoms of hyper and hypothyroidism can occur insidiously and a collateral history from family may be useful.
It is important to establish the pathological nature, position and size of the goitre to appreciate the complexity and potential complications that may occur. A large goitre that has been present for some time may be associated with tracheomalacia postoperatively. Symptoms of dysphagia, positional breathlessness with a difficulty lying flat, change in voice or stridor may alert the anaesthetist to possible difficulties with airway compromise on induction. Evidence of other systemic disease, cardiorespiratory compromise and associated endocrine or automimmue disorders should also be sought. For example, medullary thyroid cancer associated with phaeochromocytoma.
Examination
The patient should be assessed for signs of hyperthyroidism or hypothyroidism (Table 1).
An examination of the goitre or nodule should be performed to assess size and extent of the lesion. A fixed hard nodule suggests malignancy with possible tethering to surrounding structures and limited movement. An inability to feel the bottom of the goitre may indicate retrosternal spread. The trachea should be examined to check for any deviation or compression. Retrosternal or large goitres can compress surrounding structures and may elicit signs of superior vena cava (SVC) obstruction, Horner’s Syndrome, pericardial or pleural effusions. A mandatory detailed airway examination would also include assessment of atlantoaxial flexion and extension, thyromental distance, Mallampatti, mandibular protrusion and incisor distance.
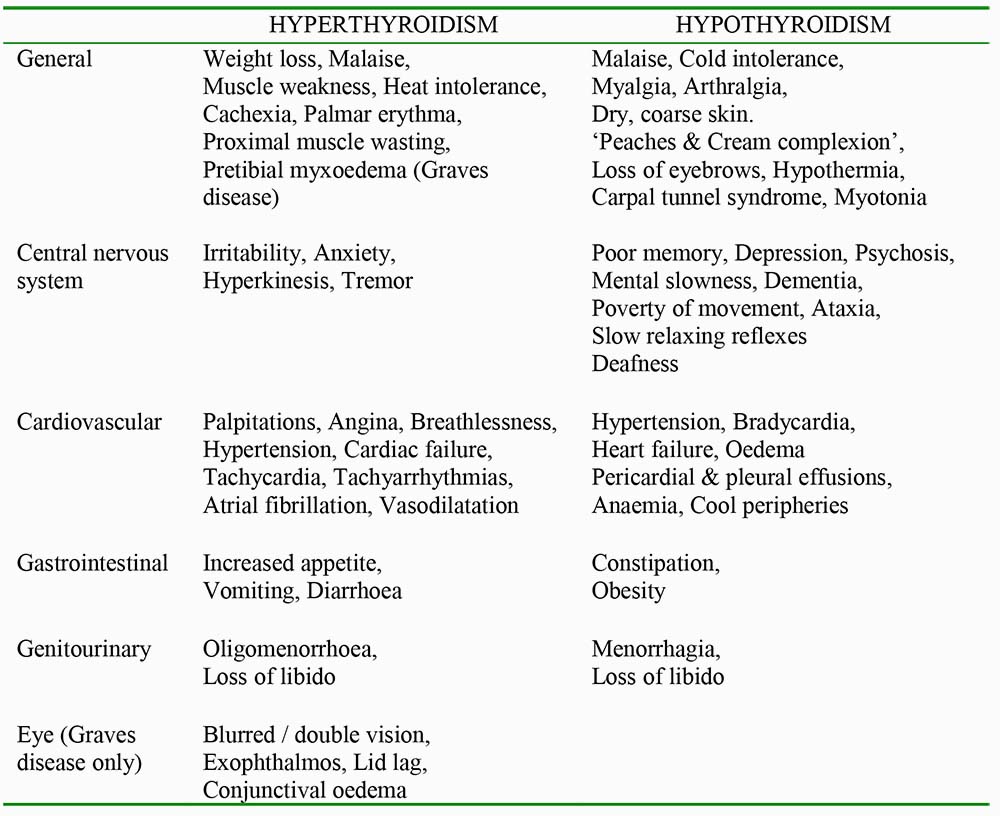
Table 1. Clinical features Hypothyroidism / Hyperthyroidism
Investigations
- Routine blood tests include Full Blood Count (FBC), electrolytes, thyroid function and corrected calcium levels. It is imperative to ensure the patient is euthyroid prior to surgery to avoid complications of a thyroid storm or myxoedema coma in the perioperative period. FBC is essential due to the potential for blood loss during the procedure plus to detect any serious adverse haematological effects of concurrent antithyroid medications. (Table 2)
- A CXR may be useful to assess the size of goitre and detect any tracheal compression or deviation. Lateral thoracic inlet views may also help to assess retrosternal extension and the tracheal anteroposterior diameter.
- If there are any concerns regarding airway compromise, a CT scan is performed to determine the extent and location of tracheal narrowing or detect tracheal invasion.
- Nasendoscopy is often performed preoperatively by ENT to document vocal cord function. This is an invaluable tool for the anaesthetist to assess the laryngeal inlet and any deviation from normal anatomy.
- Respiratory flow volume loops may show fixed upper airway obstruction but performed routinely are rarely useful
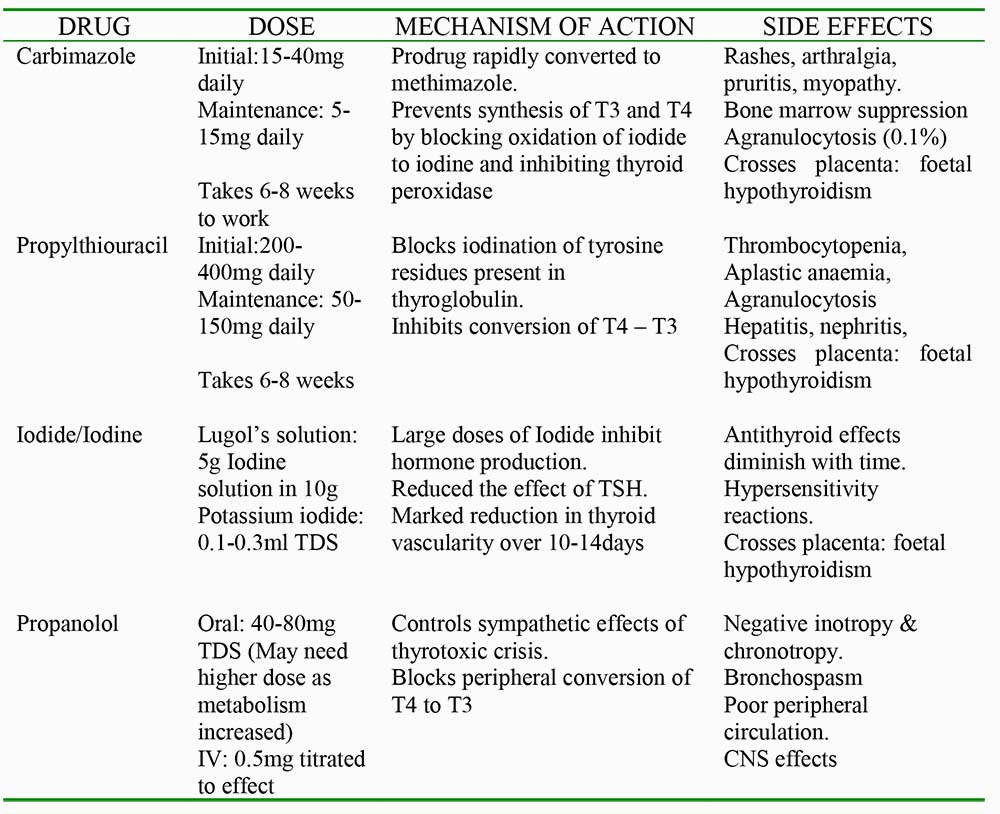
Table 2. Anti-thyroid drugs
Optimisation
Elective work should be postponed until the patient is euthyroid. On the day of surgery, usual antithyroid medications should be administered except for Carbimazole as it increases the vascularity of the gland. Benzodiazepines may be administered for anxiolysis but should be avoided if there is any airway concern. Anticholinergics may be helpful to dry secretions if an inhalational or fibreoptic technique is planned.
In emergency surgery, it may not be possible to render those patients with uncontrolled thyroid disease euthyroid. In these circumstances, hyperthyroid patients should have immediate control of symptoms with beta blockade (e.g. propanolol, esmolol), intravenous hydration and active cooling if necessary. Severely hypothyroid patients are at risk of perioperative myxoedema coma and should be treated with intravenous T3 and T4.
Intraoperative Management
Historically thyroid surgery was performed under local anaesthesia. General anaesthesia is now the preferred technique but regional anaesthesia can still have a place either as a sole technique with or without sedation or alongside general anaesthesia to enhance analgesia.
Regional Anaesthesia
Regional anaesthesia for thyroid surgery is seldom used in the UK but has been successfully employed as the sole anaesthetic technique particularly in areas with limited resources. To achieve the most successful results a multidisciplinary team approach needs to be employed with appropriate patient selection, excellent patient education and modification of surgical technique.
A commonly used technique is bilateral C2-C4 superficial cervical plexus block performed under full monitoring with or without sedation. Conscious sedation can be achieved via increments of Midazolam or a Target Controlled Infusion (TCI) of Propofol. Bilateral deep cervical plexus blocks have a higher incidence of complications including vertebral artery and subdural injection, and notably bilateral phrenic nerve palsy, which may not be tolerated in some patients.
The nerves supplying the anterolateral part of the neck emerge from the posterior border of sternocleidomastoid (SCM) as the anterior rami of C2-C4, which divide into greater auricular, transverse cervical, lesser occipital and supraclaviclar nerves (Figure 1).
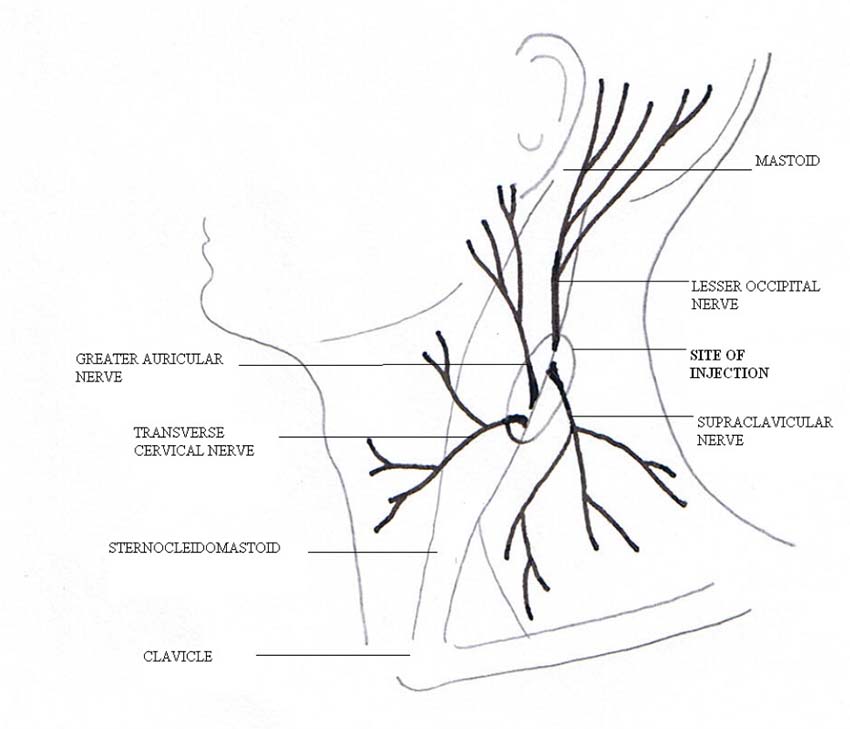
Figure 1: Superficial Cervical Plexus Block
To perform the superficial cervical plexus block, the patient should be positioned with their head extended to the opposite side, the midpoint of the posterior border of SCM visualised. 15-20mls of local anaesthetic (e.g. lidocaine and/or bupivacaine with adrenaline) is injected in a superficial wheal deep to the first fascial layer in caudad and cephalad directions along the posterior border of SCM (Figure 1). For thyroidectomy, bilateral blocks should be performed. A midline field block can be achieved by a subcutaneous injection from the thyroid cartilage to the suprasternal notch. This is a useful addition to prevent the pain from surgical retractors on the medial aspect of the neck.
Regional anaesthesia avoids the risks of a general anaesthetic, allows intraoperative voice monitoring and provides excellent postoperative analgesia. The technique may be suited to medically compromised patients (including complicating thyrotoxicosis), or those with obstructive symptoms secondary to large goitres to avoid the risks of a general anaesthetic. However, these techniques do have a number of complications including local anaesthetic toxicity, haematoma, pneumothorax, and require excellent patient cooperation.
General Anaesthesia
A variety of techniques can be employed for general anaesthesia. In most cases, the patient can be given an intravenous induction and intubated with a reinforced tube. It is advisable to demonstrate manual ventilation prior to giving a non-depolarising muscle relaxant. Care should be taken to avoid overinflating the tube cuff (or use a cuff manometer) to minimise anaesthesia related cord/tracheal damage. In our institution, we spray the vocal cords with lidocaine prior to intubation, which may help reduce coughing on emergence.
If there are any concerns regarding airway patency or distorted anatomy alternative options should be considered. Further information on managing predicted and unpredicted difficult airways can be found on the Difficult Airway Society website.
- Inhalational induction. The technique includes good preoxygenation and gradual induction with Sevoflurane. Airway adjuncts and difficult airway equipment should be immediately available if the airway is lost during induction.
- If there is concern regarding distorted anatomy or that the airway may be lost altogether on induction, an awake fibreoptic intubation may be used. This technique should be avoided in those patients with marked symptoms of airway obstruction as complete obstruction may be provoked.
- If either of these options are not suitable, a tracheostomy under local anaesthetic by the surgeons may be appropriate.
- Ventilation through a rigid bronchoscope can be used if attempts at passing an endotracheal tube fail or if there is subglottic tracheal compression.
- The Laryngeal Mask Airway (LMA) can be used for thyroid surgery but should be avoided in those with airway compromise or distorted anatomy. The use of an LMA has the advantage of allowing the assessment of the vocal cords intraoperatively via a fibreoptic scope with stimulation of the recurrent laryngeal nerve. It does not provide a definitive airway, and relies on close cooperation between the surgeon and anaesthetist to avoid displacement during surgery.
Intravenous or inhalation agents can be used for maintenance of anaesthesia. Good muscle relaxation is paramount and neuromuscular function should be monitored. Remifentanil infusion is commonly used as it reduces the need for muscle relaxation allowing for intraoperative electrophysiological testing of the recurrent laryngeal nerve in complicated cases. It can also be titrated against the blood pressure to assist in producing a bloodless surgical field during dissection, yet allow return to normal (supranormal) pressures prior to closure to check haemostasis. This may also require the use of a vasopressor such as phenylephrine boluses.
Positioning
For optimal surgical access the head is fully extended and rested on a padded ring with a sandbag between the scapulae. The eyes should be adequately padded and particular attention paid to those with exophthalmos. Access to the airway will be limited during the procedure so the endotracheal tube should be taped securely. Neck ties should be avoided. A head up tilt is preferable to allow venous drainage although care must be taken to ensure arterial pressure is not compromised. As the arms are extended by the patient’s side, long extension leads on the drips are useful.
Retrosternal goitres can usually be removed via the cervical route. However, a few may require a sternotomy.
Analgesia
The surgeon will usually infiltrate local anaesthetic and adrenaline subcutaneously prior to incision that confers some analgesic effect into the postoperative period. Regular paracetamol, non-steriodal antinflammatories (NSAIDs) plus weak opioids are usually adequate to ensure the patient is comfortable but morphine maybe required. Bilateral superficial cervical plexus blocks can significantly reduce pain and morphine requirements in the postoperative period. Administration of antiemetics is important as these patients are at high risk of postoperative nausea and vomiting. We use a combination of ondansetron and/or cyclizine with dexamethasone, which may also help reduce postoperative airway oedema.
Emergence
At the end of the procedure the surgeon may request a Valsalva manoeuvre to check for haemostasis. If there have been any concerns regarding the integrity of the recurrent laryngeal nerve, then the vocal cords are visualised with either a laryngoscope, or a fibreoptic scope via an LMA (if in place or sited post deep extubation).
Neuromuscular blockade should be fully reversed, the patient sat up and endotracheal tube cuff deflated to ensure a leak prior to extubation. In our institution, we extubate our patients awake. It is important to minimise airway manipulation and head and neck movement during emergence, to prevent coughing and straining. If the vocal cords have been sprayed with lidocaine at intubation, this may also help to achieve a smooth emergence. Alternative techniques include extubation at a deep level of anaesthesia or intravenous lidocaine (1.5mg/kg). Steroids (e.g. dexamethasone 8mg) may help to reduce airway oedema if the procedure has been long or difficult.
Postoperative Considerations
Haemorrhage
Postoperative bleeding can cause compression and rapid airway obstruction. Signs of swelling or haematoma formation that is compromising the patient’s airway should be immediately decompressed by removal of surgical clips. Clip removers should be kept by the patient’s bedside. If there is time to return to theatre, reintubation should be performed early.
Laryngeal oedema
This is an uncommon cause of postoperative respiratory obstruction. It can occur as a result of traumatic tracheal intubation or in those who develop a haematoma that can cause obstruction to venous drainage. It can usually be managed with steroids and humidified oxygen
Recurrent Laryngeal Nerve (RLN) Palsy
Trauma to the recurrent laryngeal nerve can be caused by ischaemia, traction, entrapment or transection of the nerve during surgery and may be unilateral or bilateral. Unilateral vocal cord palsy will present with respiratory difficulty, hoarse voice or difficulty in phonation whilst bilateral palsy will result in complete adduction of the cords and stridor. Bilateral RLN palsy requires immediate reintubation and the patient may subsequently need a tracheostomy.
Hypocalcaemia
Unintended trauma to the parathyroid glands may result in temporary hypocalcaemia. Permanent hypocalcaemia is rare. Signs of hypocalcaemia may include confusion, twitching and tetany. This can be elicited in Trousseau’s (carpopedal spasm precipitated by cuff inflation) or Chvostek’s sign (facial twitch on tapping parotid gland) Calcium replacement should be instituted immediately as hypocalcaemia can precipitate layngospasm, cardiac irritability, QT prolongation and subsequent arrhythmias
Tracheomalacia
The possibility of tracheomalacia should be considered in those patients who have had sustained tracheal compression by large goitres or tumours. A cuff leak test just prior to extubation is reassuring but equipment should be available for immediate reintubation if it occurs.
Thyroid Storm
Characterised by hyperpyrexia, tachycardia, altered consciousness and hypotension this is a medical emergency. Although less commonly seen now as patients are rendered euthyroid prior to surgery it can still occur in patients with hyperthyroidism when they sustain a stress response such as surgery or infection. Management is supportive with active cooling, hydration, beta blockers and antithyroid drugs. Dantrolene 1mg/kg has also been successfully used in the treatment of thyroid storm.
SUMMARY
- Patients should be clinically and chemically euthyroid prior to thyroid surgery
- Perioperative airway complications are common and the expected or unexpected difficult airway should be anticipated.
- Postoperative complications of haematoma formation, recurrent laryngeal nerve palsy, hypocalcaemia and tracheomalacia can all cause airway compromise and must be acted upon quickly.
- Thyroid storm although less common than it used to be, is a medical
ANSWERS TO QUESTIONS
- FTTFF – Thyroid function tests classically reveal high levels of T3 and T4 but low levels of TSH suppressed by the negative feedback on the pituitary. The commonest cause is Grave’s disease. These patients can be chronically hypovolaemic and vasodilated and therefore do show exaggerated response to induction. Hyperthyroidism does not increase anaesthetic requirements. Thyroid surgery is considered after medical or radioiodine treatment.
- FTFFT – Cervical plexus is formed from C1-C4. Phrenic nerve palsy is a common complication of deep cervical plexus block. A sole regional technique would not be appropriate in a patient with retrosternal goitre
- FTTTF – Hypocalcaemia should only be diagnosed on the basis of plasma ionised calcium concentration, i.e. corrected for plasma albumin concentration. Paraesthesiae and Trousseau’s sign can occur. Decreased cardiac contractility will occur and potentiaton of negative inotropes should be expected. The response of NMBA is inconsistent.
REFERENCES
- Kumar P, Clark M. Clinical medicine 4th ed. W. B Saunders 1999. 932-941
- Farling P.A. Thyroid disease. British Journal of Anaesthesia 2000; 85(1):15-28
- Malhotra S, Sodhi V. Anaesthesia for thyroid and parathyroid surgery. Continuing Education in Anaesthesia Critical Care and Pain 2007; 7(2): 55-58
- Spanknebel K, Chabot JA, DiGeorgi M, Cheung K, Lee S, Allendorf J, LoGerfo P. Thyroidectomy Using Local Anaesthesia: A Report of 1,025 Cases over 16 Years. Journal of American College of Surgeons 2005;201(3): 375-385
- www.NYSORA.com
- Dieudonne N, Gomola A, Bonnichon P, Ozier Y. Prevention of Postoperative Pain After Thyroid Surgery: A Double-Blind Randomised Study of Bilateral Superficial Cervical Plexus Blocks. Anesth Analg 2001;92:1538-42
- www.DAS.uk.com



