General Topics
Self Assessment
- The tonsils are:
- located in the oropharynx.
- venous drainage is into the pharyngeal plexus.
- supplied by the hypoglossal nerve.
- located anterior to the internal carotid artery.
- lymphoid tissue.
- Tonsillectomy is an absolute indication in:
- upper airway obstruction.
- a family history of tonsillectomies.
- recurrent ear infection.
- acute tonsillitis.
- recurrent tonsillitis with associated febrile convulsions.
- Post-tonsillectomy bleeding:
- can be associated with the surgical technique used.
- is not an emergency.
- may require fluid resuscitation prior to induction of anaesthesia.
- a rapid sequence induction is not indicated if returning to theatre.
- requires large nasogastric tube inserted prior to induction.
- Complications following tonsillectomy:
- multimodal analgesia is unnecessary.
- non-steroidal anti-inflammatory drugs are contraindicated.
- steroids have no role in tonsil surgery.
- pain is experienced for 6-10days following tonsillectomy.
- the use of local anaesthetic is an established practice.
- Surgical techniques:
- the use of diathermy for dissection is the preferred technique.
- cold blunt dissection has worse outcomes.
- the use of diathermy is associated with increased pain post-operatively.
- a Boyle-Davis gag facilitates surgical access.
- adenotonsillectomy is an approved form of treatment for obstructive sleep apnoea.
Contents:
- Introduction
- Anatomy and function
- Indications for surgery
- Pre-operative assessment
- Intra-operative management
- Post-operative management
- Complications
- Other considerations
- Controversies and the future
Introduction
Tonsillectomy is a surgical procedure that was first described in India in 1000 BC. Although not performed as often as previously, it remains a common procedure particularly for children. The indications and methods of surgery remain a controversial issue.
Anatomy and function
Tonsillectomy is defined as the surgical excision of the palatine tonsils, which are lymphoid tissue covered in respiratory epithelium and invaginated to create crypts. The tonsils are 3 separate pieces of tissue: the lingual, the pharyngeal (adenoid) and the palatine tonsil1.
The tonsils are located in the lateral oropharynx. The tonsillar branch of the facial artery forms the main arterial blood supply. The venous drainage is via a plexus surrounding the tonsil, which drains into the pharyngeal plexus. The external palatine vein enters the tonsillar bed from the soft palate. This large vein is usually responsible for the venous haemorrhage following tonsillectomy1.
The sensory supply is from the glossopharyngeal and lesser palatine nerves. Important structures deep to the inferior pole of the tonsil are the glossopharyngeal nerve, the lingual artery and the internal carotid artery.
The tonsils are lymphoid tissue and are therefore involved in lymphocyte production and are also active in immunoglobulin synthesis. They are believed to play a role in immunity though when diseased this role is no longer thought to be significant.
Indications for surgery
The indications for surgery may be absolute or relative.
The absolute indications for surgery are:
- Upper airway obstruction, dysphagia and obstructive sleep apnoea.
- Peritonsillar abscess, which is unresponsive to adequate medical management and surgical drainage.
- Recurrent tonsillitis with associated febrile convulsions.
- The requirement for biopsy to confirm tissue pathology2.
The relative indications include:
-
- Recurrent tonsillitis that is unresponsive to medical treatment. The Royal College of Surgeons, UK suggest the following criteria need to be met prior to tonsillectomy secondary to tonsillitis:
- sore throat secondary to tonsillitis.
- more than 5 episodes of tonsillitis in one year.
- to have had the symptoms for more than one year.
- the episodes of sore throats are significantly disabling3.
-
- Persistent bad-breath and taste in mouth due to chronic tonsillitis.
- Persistent tonsillitis in streptococcus carrier, which is unresponsive to beta-lactamase-resistent antibiotics.
- Pathology thought to be neoplastic2.
Contraindications for surgery are
- Bleeding diathesis.
- Acute infection.
- Anaemia.
- Significant anaesthetic risk.
Pre-operative assessment
A full history and examination is mandatory for any patient being admitted for tonsillectomy. In all children the presence of heart murmurs must be excluded. Also particular attention should be paid to detect any evidence of obstructive sleep apnoea.
Obstructive sleep apnoea. In children, adenotonsillar hypertrophy is the most common cause of obstructive sleep apnoea. The signs and symptoms include chronic hypoxaemia manifesting itself as polycythaemia and right ventricular strain (ECG shows large P waves in leads II and VI, large R waves in VI and deep S waves in V6). The symptoms may be nocturnal, such as snoring, short apnoeic episodes followed by grunting and restlessness. The daytime symptoms include headaches, not feeling rested in the morning and excessive daytime sleeping2. The use of narcotic drugs perioperatively can impair the respiratory drive and worsen the hypoxia in spontaneously breathing patients4.
The pre-operative visit should also exclude evidence of active infection, check for loose teeth and consent for perioperative analgesia.
Pre-operative Analgesia
Consider pre-operative analgesia. These can be given orally on the ward. The following drugs and doses are appropriate for paediatric patients.
- Paracetamol 20mg/kg orally
- Ibuprofen 5mg/kg orally
Intra-operative management
Induction and maintenance of anaesthesia
- Induction of anaesthesia may be either intravenous or inhalation.
- The airway may be managed with either an endotracheal tube, preferably a pre-formed or reinforced tube, or a reinforced laryngeal mask airway (LMA).
- Inhalation induction is often challenging due to the high incidence of obstruction of the nasopharynx by the adenoids.
- An intravenous induction agent of choice may be used, such as propofol (1.5- 2.5mg/kg) or thiopentone (2-7mg/kg).
- Insertion of the airway may be done under deep anaesthesia or using a muscle relaxant.
- The choice of muscle relaxant must consider the duration of surgery and the form of ventilation that will be used.
- Ventilation may be either spontaneous or controlled.
- Most children can be intubated using suxamethonium (0.5-2.0mg/kg) or a short-acting non-depolarising agent such as mivacurium (0.1-0.2mg/kg) and then allowed to breath spontaneously via the endotracheal tube.
The positioning of patient and the surgical access
- The patient is supine.
- The neck is extended and a roll is placed under the shoulders.
- Surgical access is improved with the use of a mouth clamp, commonly the Boyle-Davis gag.
- Tonsillectomy involves a shared airway therefore always ensure that the endotracheal tube is secured in the midline.
- Ensure that the airway is not obstructed or displaced by the surgeon particularly when inserting and opening or removing the Boyle-Davis gag.
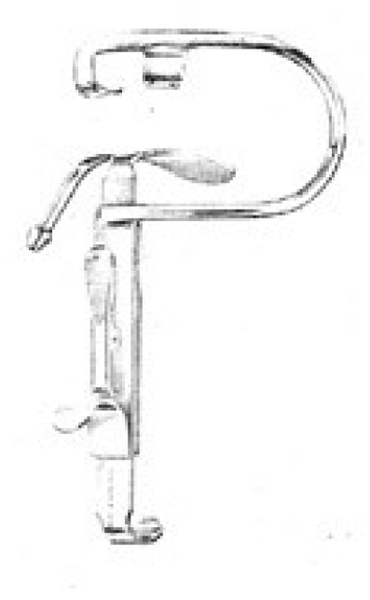
Figure 1 Boyle-Davis mouth gag
- The surgeon may use one of the following surgical techniques:
- Cold steel dissection with ties or packs for haemostasis.
- Cold steel dissection using bipolar diathermy for haemostasis.
- “hot” dissection using bipolar or monopolar diathermy (400- 600°C) for both dissection and haemostasis.
- coblation, the use of lower temperature electro-surgery (60- 70°C) for both dissection and haemostasis.
- The incidence of post-operative complications is linked to the surgical technique used
- Cold steel dissection has the lowest risk of post-operative haemorrhage.3,5
- The use of diathermy increases the risk of post-operative haemorrhage.3,5
- Extensive use of diathermy is associated with increased incidence of post-operative pain.3,5
- Intravenous access is essential though intravenous fluids are not always required (10-20mls/kg crystalloid)
- Ensure eyes are taped and protected.
Intra-operative Analgesia
Intra-operative opiates should be considered
- Morphine (0.1mg/kg)
- Fentanyl (1-5mcg/kg)
- Pethidine (0.5-2.0mg/kg, intramuscular injection)
An antiemetic should be considered
- Ondansetron (0.1mg/kg)
- Dexamethasone (0.15-1.0mg/kg in children)6a
Post-surgery and the emergence from anaesthesia
- Careful suction of the oropharynx under direct vision ensures a dry airway at the end of surgery, and limits damage to the tonsillar bed.
- Adequate spontaneous respiration is essential prior to extubation.
- Extubate the patient in left lateral position with slight head down tilt.
- Extubation should be considered once the airway reflexes have returned (ie awake extubation) and the patient is appropriate for the available skills of the recovery staff.
Post-operative management
- Administer oxygen until fully recovered.
- Post-operative analgesia
- Opiates in recovery if required. Ideally using the same drug used intra-operatively.
- Regular paracetamol.
- Regular ibuprofen.
- Observation for evidence of post-operative bleeding
- Routine observations of pulse, blood pressure, respiratory rate and pain
Complications
- Pain
- Nausea and vomiting
- Bleeding
Post-tonsillectomy bleeding
This is a serious complication, which can present in recovery or occur hours later.
Persistent swallowing is an early indicator of bleeding from the tonsil bed. The volume of blood loss cannot be measured and the patient may be hypovolaemic and need fluid resuscitation prior to induction.
The anaesthetist must consider:
- a) The patient may have a full stomach of blood and therefore is a significant aspiration risk.
- b) The intubation may be difficult due to blood in the airway and oedema from recent intubation4.
Fluid resuscitation may be necessary. The fluid status of the patient must be assessed prior to induction:
- Conscious level/Glasgow coma score
- Capillary refill time
- Pulse rate
- Urinary output
The blood pressure in young fit patients is not a good indicator of intravascular volume until the patient is profoundly hypovolaemic.
Management plan for post-tonsillectomy bleed:
- An experienced anaesthetist should be present.
- Intravenous access and fluid resuscitation prior to induction.
- A rapid sequence induction ensures quick intubation and protects the airway during induction and is the best technique. Some anaesthetists prefer an inhalation induction performed on the left side, in the head-down position.
- Use a wide bore naso/oro-gastric tube to empty the stomach. This can be inserted either before or after surgery. Ensure the stomach is empty prior to extubation
- Extubate awake in left lateral position with slight head down tilt.
- Patient must remain in recovery for an extended period to ensure the bleeding has stopped.
- Post-operative haemoglobin and coagulation screen must be checked.
Other considerations
Steroids and tonsillectomies. The use of a single dose of dexamethasone (0.15-1.0mg/kg) in children is associated with a reduced incidence of nausea and vomiting following tonsillectomy and an improved recovery as compared to placebo. This is an effective, safe and inexpensive treatment6a.
Non-steroidal anti-inflammatory agents (NSAIDs). There is no evidence that the use of NSAIDs for analgesia in tonsillectomy patients increases the incidence of bleeding. There is some evidence that there is a reduce incidence of nausea and vomiting associated with the use of NSAIDs6b.
Local anaesthetics in the tonsillar bed. There is not sufficient evidence that the use of local anaesthetic in the tonsillar bed reduces pain post-operatively6c.
Variant Creutzfeldt-Jakob disease. Prions, agents made out of protein that are variant of normal brain prion protein, accumulate in lymphoid tissue and are not reliably destroyed by surgical sterilization and therefore interpatient transmission of prion-bourne conditions is a feasible possibility. Single-use instruments were introduced in UK in 2001, however this resulted in an increase in post-operative haemorrhage. These recommendations were therefore revised it was decided to return to reusable instruments7.
Controversies and the future
- Research in tonsillectomy remains popular. The optimal technique is still not known and there is debate over whether tonsillectomy can be safely performed as a day procedure.
- Tonsillotomy using lasers for the treatment of airway obstruction secondary to large tonsils may be as effective and less painful than tonsillectomy but the effectiveness of this method has not been shown through clinical trials2.
- The indication for tonsillectomy for the treatment of recurrent sore throats is controversial. There is no current evidence that tonsillectomy reduces the incidence of sore throats in this patient group6d.
- There is insufficient evidence for adenotonsillectomy as an approved treatment for obstructive sleep apnoea in children6e.
References
- McMinn RMH. Last’s Anatomy, regional and applied. 9th ed: p 490-491
- Drake A, Carr MM. Tonsillectomy. June 2005. www.emedicine.com
- Scottish Intercollegiate Guidelines Network. Management of sore throats and indications for tonsillectomy. SIGN publication No. 34. Available at http://www.sign.ac.uk
- Allman KG, McIndoe AK Wilson IH. Emergencies in Anaesthesia: p 424
- Royal College of Surgeons. National Prospective Tonsillectomy Audit. Final report of audit carried out in England and Northern Ireland from July 2003 to September 2004.
- The Cochrane Library. Available at htpp://www.mrw.interscience.wiley.com
- 6a. Steward DL, Welge JA, Myer CM. Steroids for improving recovery following tonsillectomy in children. 2006.
- 6b. Cardwell M, Siviter G, Smith A. Non-steroidal anti-imflammatory drugs and perioperative bleeding in paediatric tonsillectomy. 2005.
- 6c. Hollis LJ, Burton MJ, Millan JM. Peri-operative local anaesthetic for reducing pain following tonsillectomy. 1999.
- 6d. Burton MJ, Towler B, Glasziou P. Tonsillectomy versus non-surgical treatment for chronic/recurrent acute tonsillectomy. 1999.
- 6e Lim J, McKean M. Adenotonsillectomy for obstructive sleep apnoea in children. 2001.
- Department of Health Press release. 14/12/2001. The re-introduction of reusable instruments for tonsil surgery. Available at htpp://www.dh.gov.uk
Answers to MCQ
-
- T
- T
- F
- T
- F
-
- T
- F
- F
- F
- T
-
- T
- F
- T
- F
- F
-
- F
- F
- F
- T
- F
-
- F
- F
- T
- T
- T



