Paediatric Anaesthesia
SELF-ASSESSMENT QUESTIONS
Before reading the tutorial consider the following questions and discuss them with your colleagues
- What are the symptoms and signs of raised intracranial pressure?
- What are the causes of hydrocephalus in children?
- What mechanisms regulate cerebral blood flow?
- What is the relationship between intracranial pressure and cerebral perfusion pressure and how can we manipulate this therapeutically?
- What additional considerations are there if the patient is a neonate?
INTRODUCTION
This article aims to look at anaesthetic techniques which can be employed for the insertion of ventriculoperitoneal (VP) shunts. It will also address the basic principles of neurophysiology which are required to treat patients with raised intracranial pressure. Prior to shunting being introduced as a treatment for hydrocephalus in the 1940s, those children affected had a poor prognosis. Only 20% of those who did not receive surgery reached adulthood and 50% of the survivors were brain damaged. The development of valved and then silicone shunt systems have dramatically improved the outlook for these patients.
INTRACRANIAL PRESSURE (ICP) AND CEREBRAL PERFUSION PRESSURE (CPP)
Successful management of patients undergoing VP shunt insertion is dependent on understanding the relationship between ICP and CPP and how this is affected by any disease process, anaesthetic agents and surgery.
The cranial contents consist of brain tissue (80%), blood (10%) and cerebrospinal fluid (10%). The volume of the cranial vault is fixed once the sutures of the skull have become fused, normally by 2 years of age. However, in the neonate, even though the volume of the vault can expand if the increase in intracranial contents occurs gradually, such as in congenital hydrocephalus, this accommodation has a maximum limit which once exceeded will lead to an increase in ICP. Any changes in the volume of the individual cranial contents can lead to an alteration in ICP and this has both pathological and therapeutic implications.
Cerebral blood flow (CBF) determines cerebral blood volume and is higher in children compared to adults (100 vs 50 ml/100g/min). It is coupled to the metabolic demands of the normal brain and regulated via oxygen requirement, PaCO2 and intracerebral acidosis. Autoregulation allows for a relatively constant blood flow across a wide range of arterial pressures which can be as low as 40 mmHg in small children. This mechanism is not available to premature neonates or during some pathological processes (e.g. infection) where the relationship between CBF and arterial pressure is more linear. Reducing PaCO2 causes vasoconstriction of the cerebral vessels, reducing CBF and hence blood volume and ICP but at the expense of oxygen delivery. Therefore hyperventilation should only be used as a short-term measure when ICP is dangerously high, prior to more definitive treatment.
Cerebrospinal fluid (CSF) is continuously produced by the choroid plexus, and after circulating through the ventricles is absorbed at the arachnoid villi. In children the rate of production of CSF is 0.2-0.4 ml/min with around 250 ml produced and absorbed per day and at any given time around 70 mls is present in the head. Any interruption to normal flow, increased production or decreased reabsorption of CSF can manifest itself as hydrocephalus which may lead to raised ICP. The classical distinction between obstructive and communicating hydrocephalus is less useful clinically as the cause of reduced absorption of CSF in communicating hydrocephalus is usually functional obstruction at the arachnoid villi (e.g. by blood or protein).
Brain tissue, the largest component of the cranial contents, may be pathologically enlarged by the presence of a space occupying lesion which if of insidious onset may lead to a gradual increase in ICP.
Cerebral perfusion pressure is defined as the difference between the mean arterial pressure (MAP) and the sum of intracranial pressure and the central venous pressure (CVP).
CPP = MAP – (ICP + CVP)
The normal range of ICP in neonates is 2-4 mmHg (7-15 mmHg in adults). Increased ICP gives rise to such symptoms and signs as: vomiting, irritability, drowsiness, bulging fontanelle (if still present), increasing head circumference, downward gaze of the eyes (“setting sun” sign), Cushing’s response (hypertension and bradycardia). At ICP > 20mmHg focal ischaemia occurs and at >50 mmHg global ischaemia occurs if CPP remains constant (this is the reason MAP is raised therapeutically with the use of vasoconstrictors in some cases of raised ICP). Long term increases in ICP can impair neurological development, whilst in the acute setting, high ICP can cause distortion and displacement of the cerebral contents through the foramen magnum – “coning” – leading to coma, respiratory arrest and death. Most anaesthetic agents cause a reduction in MAP but this potentially deleterious effect is usually offset by the corresponding reduction in the cerebral metabolic demand for oxygen (CMRO2).
THE INDICATIONS FOR SHUNTING
There are several causes of hydrocephalus which may necessitate the insertion of a VP shunt (see Box 1). VP shunts are therefore required for a wide range of patients from newborns to older children with the potential for a number of co-morbidities. The shunt provides a route for the CSF to drain and decreases ICP. The proximal end is placed in the ventricle and the distal end at a site where the CSF can be absorbed (most commonly peritoneum but atria and pleura are also used). The complications associated with VP shunts include blockage, infection and over drainage, all of which may necessitate revision surgery.
Endoscopic third ventriculostomy (ETV) is an alternative treatment for hydrocephalus in carefully selected patients. A neuroendoscope is used to make a hole in the floor of the third ventricle to facilitate CSF drainage. The technique was originally developed in the 1900s but was abandoned due to severe complications, most likely attributable to poor anaesthesia and surgical equipment. Developments in optics, image processing and improvements in anaesthesia have enabled ETV to be used safely with comparable results to VP shunts as Warf et al have demonstrated in their series from Mbale, Uganda. ETV has the benefit of avoiding the long-term complications of VP shunts and the attendant costs of follow up and revision surgery, which has enormous implications for developing countries with limited resources.
The incidence of infantile hydrocephalus is estimated at 3-5 cases per 1000 live births. The peak ages of presentation include the first weeks of life, 4-8 years and early adulthood. An estimated 750,000 people have hydrocephalus, approximately 160 000 ventriculoperitoneal shunts are inserted worldwide each year, with over 56 600 children under 18 years thought to have a shunt in place. Depending on the indication for VP shunt insertion, the procedure may be urgent or an emergency with additional attendant risks (full-stomach, abnormal electrolytes, hypovolaemia, precipitously high ICP).
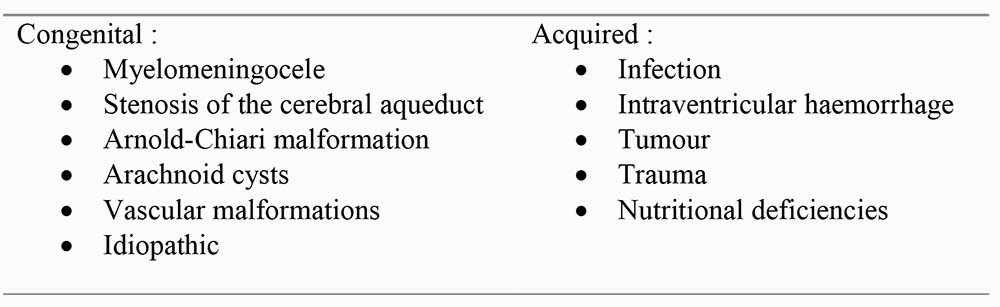
Table 1: Causes of hydrocephalus
PREOPERATIVE ASSESSMENT
The preoperative visit is an essential component of any anaesthetic technique. This should include the standard anaesthetic history of problems with previous anaesthetics, family history of reactions to anaesthesia, past medical history, current medication (e.g. anticonvulsants, acetazolamide,furosemide), allergies and last oral intake. Particular attention should be paid to the possibility of co-morbidities including problems with the cardiovascular (e.g. congenital cardiac disease) and respiratory systems (e.g. bronchopulmonary dysplasia, kyphoscoliosis, recurrent respiratory infections secondary to neurological dysfunction).
Examination should include assessment of the airway, cardiorespiratory and neurological systems, which in cases of raised ICP may demonstrate reduced level of consciousness (LOC) and therefore increased risk of pulmonary aspiration. Volume status should be determined as prolonged vomiting and dehydration may necessitate intravenous fluid preoperatively.
Blood results should be reviewed to ascertain the level of haemoglobin and clotting function so that appropriate blood products can be ordered as indicated. Urea and electrolytes should be checked if medical problems or drug treatment suggest that they may be abnormal and require attention perioperatively.
The preoperative visit is an opportunity to apply topical anaesthesia over a suitable vein if intravenous induction is planned. Sedative premedication should be considered carefully as it may exacerbate or mask signs of neurological dysfunction – conversely, an anxious combative patient may have a detrimental rise in ICP during induction. The patient should be carefully monitored whilst awaiting surgery for signs of neurological deterioration as this can occur rapidly. If the preoperative assessment reveals a patient with multiple co-morbidities, such as an ex-premature infant with chronic lung disease, the need for additional respiratory support in the postoperative period should be considered and organised in advance.
PREPARATION, EQUIPMENT AND MONITORING
Prior to induction all anaesthetic equipment and drugs should be checked to ensure they are available and in good working order. This should include a means of delivering oxygen and volatile anaesthetic agent, suction, a tilting trolley and monitoring. Equipment such as facemasks, oropharyngeal airways, tracheal tubes and laryngoscopes should be available in a range of sizes appropriate for the patient. A weight appropriate breathing circuit should be checked for correct configuration and patency. Standard monitoring should include pulse oximetry, electrocardiogram, non-invasive blood- pressure, oxygen concentration, and capnography.
INDUCTION OF ANAESTHESIA
The method of induction is determined by the circumstances of the case and the preference of the patient and the anaesthetist.
Intravenous induction allows for rapid control of the airway in emergency situations if the patient is not fasted and if no difficulties with the airway have been anticipated. This may be achieved using a suitable induction agent in a carefully titrated sleep dose. (proprofol 2-4 mg/kg, thiopentone 3-5 mg/kg) Hypotension should be avoided because of the risk of decreasing CPP in the face of raised ICP. Ketamine should not be used as itcan increase ICP. Muscle relaxation can be achieved with the use of a neuromuscular blocking agent (NMB). Suxamethonium can be used if the risk of aspiration outweighs the problems of transient increases in ICP, otherwise non-depolarising NMB are preferable.
Gaseous induction is an acceptable alternative with a non-irritant volatile anaesthetic agent such as sevoflurane or halothane. A rapid gaseous induction is preferable to prolonged attempts at cannulation in a distressed and unwell child. Once anaesthetized, intravenous access should be established quickly to allow the use of a NMB to facilitate control of the airway. Hypercarbia should be avoided as it causes cerebral vasodilation and may worsen raised ICP especially in combination with laryngoscopy and airway manipulation. The airway should be secured by intubation of the trachea with an appropriate sized tracheal tube. This should be a reinforced (armoured) tube if available but a standard tube can be used providing this information is communicated to the surgeon, as the tube will be more likely to kink during positioning. The tube should be firmly secured with waterproof tape and dressing and the eyes should be padded and taped.
The patient should be positioned to allow good access for the surgeon and to avoid any undue pressure on vulnerable areas. Consideration should be given to optimizing venous drainage to increase CPP, reduce venous bleeding and improve the surgical field. The core temperature of the patient should be monitored (rectal or oesophageal) and warming devices (e.g. warm air blankets) used as required to maintain normothermia.
MAINTENANCE OF ANAESTHESIA
Anaesthesia can be maintained with a volatile agent and a mixture of oxygen and air. The aim is to maintain CPP until the raised ICP is relieved by positioning of the VP shunt. To do this hypotension should be avoided and minute ventilation controlled to maintain normocarbia (end tidal CO2 4 4.5 kPa) to optimise CPP and avoid increases in ICP. Positive end-expiratory pressure (PEEP) should be minimised to avoid venous congestion in the head but may be used if there are difficulties in maintaining oxygenation.
The most stimulating parts of the surgery include the initial incision and tunnelling under the skin. A short acting opioid, such as fentanyl (1-3 mcg/kg) or remifentanil (1 mcg/kg), or increased depth of anaesthesia, can be used to attenuate the increase in heart rate and ICP. Post-operative analgesia can be provided by a combination of infiltration of local anaesthetic such as bupivicaine 0.25% (0.5-0.75 ml/kg) and paracetamol (15 mg/kg) either intravenous or per rectum. High doses of long acting opioids should be avoided because of potential detrimental effects on conscious level.
POSTOPERATIVE MANAGEMENT
At the end of the procedure neuromuscular blockade can be antagonized using neostigmine (50 mcg/kg) combined with an anticholinergic (e.g. atropine 25 mcg/kg). Most patients can be extubated once awake, avoiding hypercarbia, and with a technique which minimizes the risk of aspiration (lateral or sitting). Analgesia can be achieved with a combination of paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs) if not contra indicated with additional oral opioid for breakthrough pain. The patient should be monitored in a suitable environment by those familiar with paediatric neurosurgical cases and able to carry out regular neurological observations.
THE NEONATAL PATIENT
A reasonable proportion of patients requiring VP shunt insertion are neonates (8% in a series from California). Neonates are physiologically immature and so present additional considerations for the anaesthetist. Many of these patients are premature, with a low birth weight, with congenital hydrocephalus needing urgent surgical treatment in the first days of life. This group are more likely to have complications with their VP shunts and so return more frequently for further surgery to correct these problems.
Preoperative assessment should look for problems associated with neonates and prematurity such as anaemia, coagulopathy, jaundice, respiratory disease and congenital cardiac problems. Additional investigations such as an echocardiogram may therefore be indicated. Blood and any other required products should be readily available prior to surgery.
Gaseous induction of anaesthesia with sevoflurane provides good cardiovascular stability. Neonates are a more technically challenging group of patients and particular attention must be paid to securing tracheal tubes and intravenous cannulae as endobronchial intubation and extravasation are commonly encountered problems. Congenital hydrocephalus may have distorted the anatomy of the skull which can make management of the airway more difficult. Often a pillow placed under the body of the neonate can facilitate laryngoscopy. The use of a naso-gastric tube is an important component of managing the neonatal airway and ventilation. Handling should be careful and minimal to reduce the risks of complications (e.g. pneumothoraces).
Neonates have a high surface area to volume ratio and so lose heat quickly and their mechanisms for maintaining thermal homeostasis are poorly developed. Core temperature must be recorded and active measures taken to maintain body heat. These include, increasing the ambient temperature, warm air blankets, overhead heaters, heat-moisture exchangers to warm inspired gases, warming intravenous fluids and covering of exposed areas.
Drug metabolism is different in neonates with an immature liver but a relatively higher volume of distribution. Paracetamol, local anaesthetics, volatile anaesthetic agents and opioids are all used in relatively lower doses. Careful attention must be paid to fluid balance as renal function is also immature in the neonate. An infusion of 10% glucose may be required to maintain blood glucose within the normal range but hypo and hyperglycaemia should be avoided. Regular monitoring of blood glucose and electrolytes allows for adjustment of fluid regimens as required.
Postoperatively some neonates will require further respiratory support (especially pre-term infants with bronchopulmonary dysplasia). Patients that can be extubated will need apnoea monitoring for 24-hour hours postoperatively in addition to regular neurological observations.
CONCLUSION
Anaesthesia for the insertion of VP shunts requires an understanding of neurophysiology and the relationship between ICP and CPP in both normal and disease states and preparation to provide anaesthesia across the entire paediatric age range from premature neonates to post pubertal children. The application of sound basic anaesthetic principles will allow for the safe conduct of surgery in this varied and challenging population of children.
ANSWERS TO SELF-ASSESSMENT
- Symptoms and signs include headache, vomiting, irritability, drowsiness, bulging fontanelle, increasing head circumference, downward gaze of the eyes, and later Cushing’s response (hypertension and bradycardia), coma and reduced respiratory rate.
- Any process that either increases production, reduces absorption or interferes with circulation of CSF, see box 1.
- CBF is regulated via oxygen requirement, PaCO2, intracerebral acidosis and hormonal influences and is coupled to metabolic demand. Autoregulation keeps blood flow constant over a range of pressures. (See also TOTW Cerebral Blood Flow and Intracranial Pressure Parts 1 and 2)
- See equation in text. We can increase CPP by either increasing MAP (with fluids, vasoconstrictors or inotropes) or by reducing ICP (hyperventilation, mannitol, sedation and analgesia) and reducing CVP (head up position, head midline, avoiding obstruction of venous drainage of neck with central lines or tight endotracheal tapes)
- See explanation in text (and also TOTW Neonatal Anaesthesia 1: physiology)
REFERENCES AND FURTHER READING
- Paediatric and Neonatal Anaesthesia: Anaesthesia in a Nutshell 2004 Black A and McKewan A, Butterworth Hinemann.
- Neuroanaesthesia: Anaesthesia in a Nutshell 2002 Dinsmore J and Hall G, Butterworth Hinemann
- Wu Y et al. Ventriculoperitoneal Shunt Complications in California: 1990 TO 2000. Neurosurgery 2007, 61:557–563 www.neurosurgery-online.com
- Warf B, Hydrocephalus in Uganda: the predominance of infectious origin and primary management with endoscopic third ventriculostomy. J Neurosurg 2005, 102:1–15
http://www.ifglobal.org/uploads/documents/articleBenWarf_ETV%20(JNP).pdf - Engelhard HH, Hydrocephalus eMedicine 2007 http://www.emedicine.com/med/TOPIC2884.HTM
- Kramer LC, Management of Spina Bifida, Hydrocephalus and Shunts eMedicine 2007 http://www.emedicine.com/ped/TOPIC2976.HTM
- Mohammed IS, Neonatology Considerations for the Pediatric Surgeon 2006 http://www.emedicine.com/ped/TOPIC2982.HTM
- Hill L, Cerebral Blood Flow and Intracranial Pressure. Parts 1 and 2 Tutorial of the week. www.worldanaesthesia.org
- Walker I and Wouters K, Neonatal Anaesthesia 1: physiology. Tutorial of the week. www.worldanaesthesia.org



