Obstetrics Anaesthesia
MCQ QUESTIONS (True / False)
Before reading this tutorial, try to answer the following questions. The answers can be found at the end of the article.
- Non-obstetric surgery in pregnancy:-
- occurs in approximately 5%
- appendicectomy is the most common procedure performed
- is associated with increased congenital abnormalities
- is associated with increased spontaneous abortion
- laparoscopy is contraindicated
- During pregnancy:
- MAC decreases by 10%
- plasma cholinesterase levels increase
- suxamethonium has a clinically prolonged duration of action
- platelet consumption decreases
- Functional Residual Capacity (FRC) may be less than alveoli closing volume
- Concerning foetal safety during non-obstetric surgery:
- teratogenicity is the most serious risk
- hyperoxia is not dangerous
- foetal heart rate monitoring perioperatively improves foetal outcome
- ketamine is the anaesthetic drug of choice
- maternal hypercarbia should be avoided
INTRODUCTION
During pregnancy, surgery for non-obstetric procedures occurs in up to 2% of women. This figure may be considerably higher in the first trimester as pregnancy may go undetected at the time of surgery. Approximately 42% of procedures occur in the first trimester, 35% during the second and 23% during the third.
The range and incidence of procedures are similar to the non-pregnant group of young women. Acute abdominal problems are most common, with appendicectomy ranking first followed by cholecystectomy. Pregnancy predisposes to cholelithiasis and approximately 3% of pregnant women develop gallstones, however only a limited number require surgery. Other common problems include adnexal disease (e.g. ovarian cysts which may rupture or become torted) and trauma. Much less common are cardiovascular or neurological emergencies. The demands of pregnancy on the cardiovascular system can cause decompensation of valvular heart disease or precipitate aortic dissection.
Anaesthetists who care for pregnant patients undergoing non-obstetric surgery must provide safe anaesthesia for both the mother and the foetus. To maintain maternal safety the physiological and anatomical changes of pregnancy must be considered and anaesthetic techniques and drug administration modified accordingly. Foetal wellbeing is related to avoidance of foetal asphyxia, teratogenic drugs and preterm labour.
MATERNAL SAFETY
Physiological / anatomical changes
Cardiovascular changes
Maternal cardiac output increases in pregnancy by 50% and peaks by the end of the 2nd trimester. This is due to a combination of an increased heart rate (25%) and stroke volume (30%). The increase in heart rate is a reflex response to a lowered systemic vascular resistance (SVR) caused by circulating oestrogen and progesterone. Left ventricular hypertrophy and dilatation facilitate the increase in stroke volume but myocardial contractility remains unchanged.
ECG changes that occur in pregnancy and are entirely normal include left axis deviation and minor ST / T wave changes. Heart murmurs are also common due to turbulence associated with increased blood flow.
As the enlarging uterus moves out of the pelvis it can compress the inferior vena cava and the descending aorta in the supine position. The compression of the inferior vena cava causes decreased venous return and hence preload, which reduces cardiac output by up to 20%. This is known as supine hypotension syndrome. Pregnant patients compensate for hypotension by an increase in sympathetic tone causing vasoconstriction and tachycardia. This may divert blood away from organs such as the uterus, with subsequent foetal distress. The compression of the aorta can cause a further reduction in uterine blood flow. Aortocaval compression becomes clinically relevant from approximately 20 weeks gestation. It can be relieved by a left lateral tilt of 15 degrees, which is therefore essential in all pregnant patients in the supine position after 20 weeks. This is especially important to remember when a patient is under regional anaesthesia/analgesia since hypotension may be potentiated by a sympathetic block.
There is an increase in blood volume in pregnancy of between 35-50% at term. There is both an increase in plasma volume and red cell volume, but a greater increase in plasma volume which leads to a dilutional anaemia. The reduced blood viscosity aids flow through the uteroplacental circulation and the increase in volume serves as a protective measure against haemorrhage at delivery. It must be remembered that because of the increase in blood volume, along with a resting tachycardia, there may be delay in the onset of the classical symptoms and signs of hypovolaemia.
Pregnancy is a hypercoaguable state with an increase in most clotting factors. The platelet count may fall but there is actually an increase in production and consumption. Pregnancy is a significant risk factor for thromboembolism and therefore thromboprophylaxis is essential in the postoperative period when the risk is further increased by immobility and the hypercatabolic state.
Respiratory changes
The respiratory changes of pregnancy are perhaps the most important for anaesthetists to note.
There is an increased oxygen demand of up to 60% at term. This is met by an increased cardiac output and an increase in minute ventilation (MV). MV increases early due to an increase in respiratory rate and tidal volume and is up by 45% by term. This increase in MV is mediated by progesterone which acts as a respiratory stimulant. The increased MV causes a mild respiratory alkalosis (PaCO2 decreases by 1kPa). The increase in pH is limited by increased renal bicarbonate excretion. Relative hypocapnia should be maintained when artificially ventilating pregnant patients. An increase in maternal PaCO2 limits the gradient for CO2 diffusion from foetal to maternal blood leading to foetal acidosis.
The functional residual capacity (FRC) is the main oxygen reserve in the apnoeic patient and is decreased in pregnancy due to the enlarging uterus displacing the diaphragm upwards. This is further exacerbated in the supine position and increases as the pregnancy progresses.
Airway management may be challenging during pregnancy. Bag-mask ventilation may be more difficult due to increased soft tissue in the neck. Laryngoscopy can be hindered by weight gain and breast engorgement. Increased oedema of the vocal cords due to increased capillary permeability can hinder intubation and increase the risk of bleeding. This may make further attempts at intubation more difficult and increase the incidence of failed intubation. Increased maternal oxygen consumption and reduced FRC results in rapid oxygen desaturation during attempts at intubation. Smaller sized endotracheal tubes may be needed and all anaesthetists should be familiar with a failed intubation drill. Nasal intubation should be avoided due to increased vascularity of mucous membranes.
Given the combination of these changes, careful pre-oxygenation is essential prior to induction of anaesthesia. This should be confirmed if possible by monitoring the end tidal oxygen fraction. In a well pre-oxygenated patient this should be >0.9. Pre-oxygenation can be less efficient in the term parturient in the supine position because the closing volume of the alveoli may be greater than the FRC. Pre-oxygenation in a slightly head up position may help this.
Gastrointestinal changes
Circulating progesterone reduces the lower oesophageal sphincter (LOS) tone, increasing the incidence of oesophageal reflux. This is further exacerbated by anatomical changes. The gravid uterus is displaced upwards and to the left pushing the intra-abdominal part of the oesophagus into the thorax in most pregnant women. This often makes the LOS incompetent and lowers the barrier pressure. These factors, along with a lowered stomach pH, increase the risk and severity of aspiration pneumonitis under general anaesthesia.
It is recommended that from 16 weeks gestation patients undergoing general anaesthesia should be given prophylaxis against aspiration pneumonitis. This usually includes a non-particulate antacid such as sodium citrate 0.3M 30ml and an H2 receptor antagonist e.g. ranitidine 150 mg orally or 50mg intravenously. Some anaesthetists may also choose to give a prokinetic such as metoclopramide. Induction of anaesthesia should be by a rapid sequence technique with cricoid pressure and a fast acting muscle relaxant such as suxamethonium. A cuffed endotracheal tube should be used. At the end of the procedure patients should be extubated fully awake in the lateral position.
- Remember left lateral tilt to prevent aortocaval compression
- Remember meticulous pre-oxygenation to prevent hypoxia
- Remember antacid prophylaxis and rapid sequence induction to reduce risk of aspiration
Drugs: Altered pharmacokinetics / pharmacodynamics
Pharmacokinetic and pharmacodynamic profiles are altered in pregnancy and drugs should be titrated accordingly.
The minimum alveolar concentration (MAC) of volatile agents is reduced by 30% under the influence of progesterone and endogenous endorphins. There is a decrease in plasma cholinesterase levels by 25% from early pregnancy, but prolonged neuromuscular blockade with suxamethonium is uncommon due to increased blood volume causing an increased volume of distribution. Non-depolarising muscle relaxants have a prolonged duration of action. Neuromuscular monitoring with a nerve stimulator is recommended.
The increased blood volume causes a physiological hypoalbuminaemia. This alters the plasma protein binding and increases the free or unbound fraction of drugs. An example of this is local anaesthetics. As well as decreased plasma protein binding, there is also increased neural tissue sensitivity. These factors decrease the therapeutic doses and also the toxic plasma levels of local anaesthetic agents.
The volume of the epidural and subarachnoid spaces is reduced due to the gravid uterus compressing the inferior vena cava causing distension of the epidural venous plexus. This leads to a more extensive spread of local anaesthetic agents administered during central neuraxial blockade and also increases the risk of inadvertent intravascular injection. Careful aspiration prior to injection should always be performed.
FOETAL SAFETY
Prevention of foetal asphyxia
One of the most serious risks to the foetus during maternal surgery is intrauterine asphyxia. This must be avoided by maintaining maternal oxygenation and haemodynamic stability. It is extremely important to avoid hypoxia, extreme hyper and hypocarbia, hypotension and uterine hypertonus. Maternal hypoxaemia causes uteroplacental vasoconstriction and decreased perfusion, causing foetal hypoxia, acidosis and ultimately death.
There is a linear relationship between maternal and foetal PaCO2. Maternal hypercarbia limits the gradient for CO2 diffusion from foetal to maternal blood and leads to foetal acidosis. Therefore endtidal carbon dioxide monitoring should be used to guide ventilation and arterial blood gas analysis should be considered during prolonged or laparoscopic surgery. Hypocarbia is also problematic, potentially causing uteroplacental vasoconstriction and foetal acidosis, although the mild hypocapnia that occurs with the physiological changes of pregnancy should be maintained (PaCO2 around 4kPa).
Uteroplacental circulation is not autoregulated and hence perfusion is entirely dependant on the maintenance of an adequate maternal blood pressure and cardiac output. Hypotension can be caused by anaesthetic drugs, central neuraxial blockade, hypovolaemia or aortocaval compression. Maternal hypotension needs to be treated aggressively by ensuring left lateral tilt and boluses of IV fluids. Additional vasopressors may be required and currently it is felt alpha agonists such as phenylephrine and metaraminol produce a better foetal acid balance than indirect sympathomimetic agents such as ephedrine. Ephedrine also has a relatively slow onset and long duration of action and tachyphylaxis can occur making titration difficult.
Drugs and teratogenicity
Teratogenicity is defined as the observation of any significant change in the function or form of a child secondary to prenatal treatment. The teratogenicity of a drug depends upon the dose administered, the route of administration, the timing of foetal exposure and the species administered to. During the first two weeks of human gestation the teratogens have an all or none phenomenon; the foetus is lost or is preserved fully intact. The period from the 3rd to the 8th week of gestation, represents the most important time for organogenesis during which drugs can exert their most serious teratogenic effects. After this, drug exposure should not cause organ abnormalities, but foetal growth retardation may occur.
Although most anaesthetic drugs are known teratogens in certain species, most agents are safe in humans. The foetus is at more risk from asphyxia than the teratogenic effect of anaesthetic drugs. Studies looking at the outcomes of women who underwent surgery during pregnancy suggest no increase in congenital anomalies in their offspring but an increase in foetal loss, growth restriction and low birth weight attributed to the requirement for surgery (not anaesthetic administration). There is some concern from animal and epidemiological studies that exposure to general anaesthetic agents may cause neurodevelopmental delay in infants. It is difficult to extrapolate animal findings to humans and in epidemiological studies it is difficult to distinguish the potential confounding effects of anaesthesia, reason for surgery and underlying medical conditions.
Nitrous oxide inhibits methionine synthetase, and therefore there is concern it could affect DNA synthesis in the developing foetus. It has also been shown to be teratogenic during peak organogenesis in rodents, but there is no evidence in humans. Anaesthesia can be safely delivered without nitrous oxide and therefore many would avoid its use during non-obstetric surgery in the pregnant woman.
Another drug of concern is ketamine. This causes increased uterine tone and foetal asphyxia and should not be used in the first two trimesters. The effect is not seen in the third trimester.
Benzodiazepines have been associated with a cleft lip and palate in animal studies. The association in humans is controversial. A single dose has not been associated with teratogenicity. Long term use should be avoided as neonatal withdrawal may occur. Single doses may be useful to provide anxiolysis preoperatively.
Prevention of pre-term labour / foetal monitoring
Surgery during pregnancy increases the risk of spontaneous abortion, preterm labour and preterm delivery. This risk is increased with intra-abdominal procedures. Uterine manipulation should be kept to a minimum and drugs that increase uterine tone (e.g. ketamine) should be avoided. Prophylactic tocolytic therapy is controversial as there are associated maternal side effects and efficacy during nonobstetric surgery has not been proven.
Perioperative foetal monitoring is also an area of controversy. From 18-22 weeks foetal heart rate (FHR) monitoring is feasible and from 25 weeks heart rate variability can be observed. Continuous monitoring may be technically difficult during abdominal operations or in cases of maternal obesity. Anaesthetic agents reduce both baseline FHR and FHR variability and therefore interpretation is difficult and may lead to unnecessary interventions. Anaesthetic agents do not cause decelerations or persistent foetal bradycardia and these changes may indicate foetal distress. Monitoring may enable swift action to be taken such as the optimisation of maternal haemodynamics, oxygenation and ventilation.
Although perioperative foetal monitoring has not been shown to improve foetal outcome, a sensible approach would be to use cardiotocography (CTG) monitoring where possible and practical when the foetus is of a viable age. The obstetricians and neonatologists should be informed, appropriately trained personnel available to interpret the CTG and a prior action plan in place for when there is evidence of foetal distress unresponsive to conservative measures.
If the foetus is not of a viable age or perioperative CTG monitoring is not possible / practical, FHR monitoring should occur pre and post-operatively and staff should be alert to the signs of premature labour.
LAPAROSCOPIC SURGERY
There were previous concerns regarding foetal safety during laparoscopic surgery. These included fears of direct uterine and foetal trauma, foetal acidosis due to absorbed carbon dioxide and decreased maternal cardiac output secondary to the increased intra-abdominal pressure and positioning with a subsequent decrease in uteroplacental perfusion.
There are advantages to laparoscopic surgery for both the mother and the foetus such as decreased post-operative pain (and therefore less need for analgesics), shorter recovery times and a lower risk of thromboembolic events.
A Swedish study compared laparotomy and laparoscopy performed in pregnancy in over 2 million deliveries. Premature delivery, growth restriction and low birth weight were more common in both groups compared to the general population but there were no differences between the laparotomy and laparoscopy groups.
Pregnancy should therefore not be seen as a contraindication to laparoscopic surgery if surgery is required. Certain precautions should be taken. Pneumatic stockings should be used to promote venous return and the lowest pressure pneumoperitoneum (<12mmHg) should be used where possible. Aortocaval compression should be avoided and changes in position should be undertaken slowly. PaCO2 should be closely monitored by the routine use of end tidal carbon dioxide monitoring and consideration of arterial blood gas analysis in selected cases. FHR monitoring may be advisable to detect foetal compromise early allowing optimisation of maternal haemodynamics. FHR changes may indicate the need for temporary deflation of the pneumoperitoneum.
POSTOPERATIVE CARE
As previously stated pregnancy induces a hypercoaguable state and the risk of thromboembolic disease is further increased by postoperative venous stasis. Attention to thromboprophylaxis is therefore essential. This should include early mobilisation, maintaining adequate hydration, TED stockings and other calf compression devices and consideration of pharmacological prophylaxis (for example subcutaneous low molecular weight heparin).
Analgesia
Adequate analgesia is important as pain will cause increased circulating catecholamines which will impair uteroplacental perfusion. Analgesia may mask the signs of early preterm labour and therefore tocometry is useful to detect contractions. This will enable tocolysis to be administered without delay. If a pregnancy continues beyond the first postoperative week the incidence of premature labour is no higher than the non-surgical pregnant patient.
The FDA (United States Food and Drug Administration) introduced a classification system in 1979 of drug risk to the foetus. This runs from Category A (safest) to Category X (known danger).
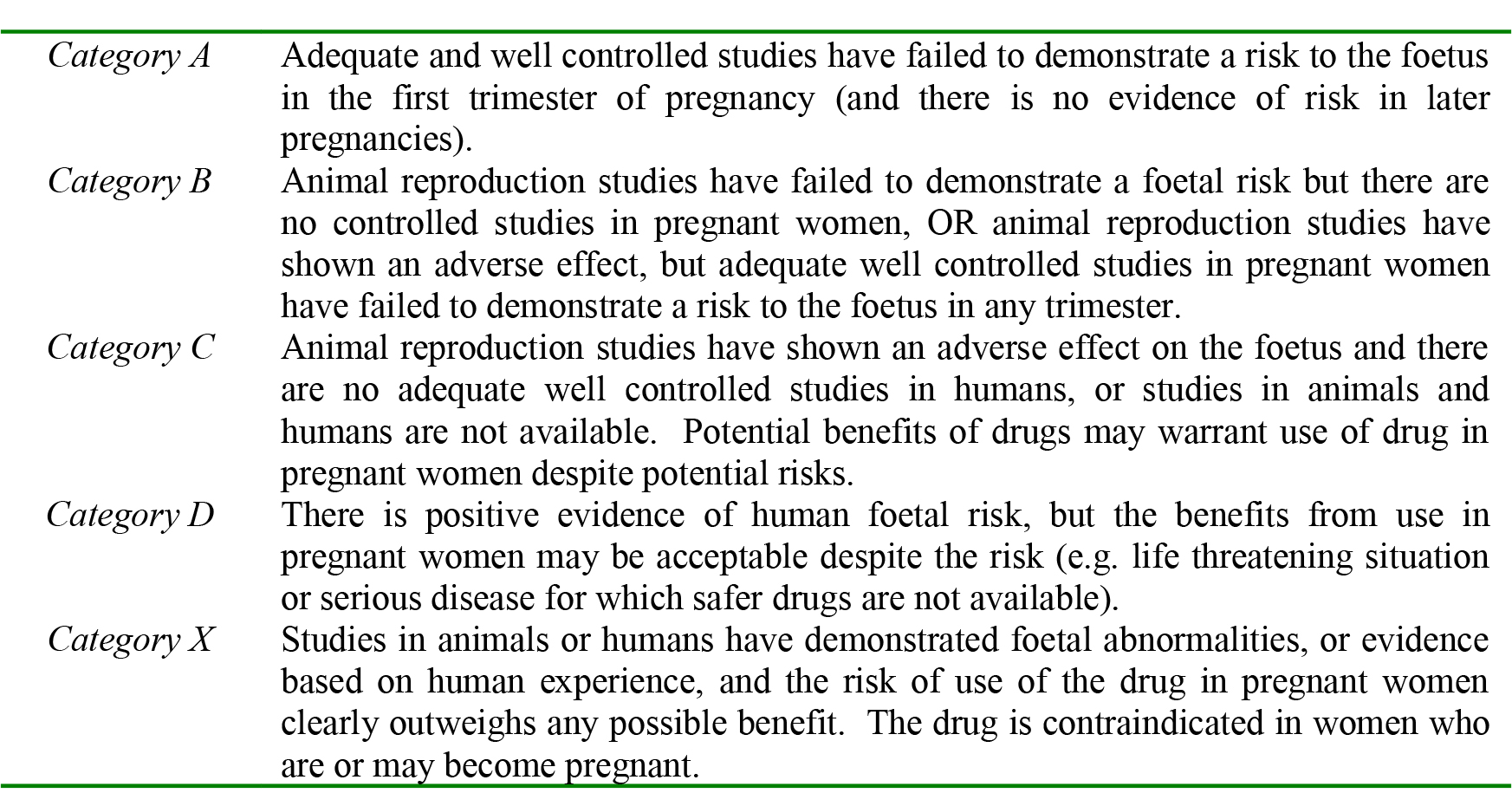
Table 1. FDA classification of foetal harm risk from drugs.
There are other classification systems from other countries. The FDA requires a relatively large amount of high quality data for a drug to be classified as Category A. As a result many drugs classified as Category A in other countries are classified as Category C by the FDA.
The table below shows how many of the common analgesic drugs used are classified by the FDA and their safety in breastfeeding.
PUERPERIUM
The puerperium covers the 6 week period following childbirth during which time the various changes that occurred during pregnancy revert to the non pregnant state. The cardiovascular system and blood volume return to normal by the end of 2 weeks. After delivery of the placenta the uterus is the size of a 20 week pregnancy and decreases by 1 finger breadth each day, so that by day 12 it is no longer palpable. It is wise to avoid elective surgery in the initial 6 week post partum period to allow the body to return to its normal physiological function.
If anaesthesia is undertaken in this time or for operative delivery of the foetus women may wish to know the effects on breastfeeding. Administration of drugs to the breastfeeding mother can inhibit lactation or cause direct harmful effects to the infant due to excretion in breast milk. For many medications there is insufficient evidence available to provide accurate guidance on drug safety during breastfeeding. When prescribing or administering drugs consider:
- Is the medication really needed?
- Minimise drug exposure by administering just after breastfeeding.
- Breastfeeding is the gold standard for infant nutrition. Balance the risk of drug excretion in milk with advantages of continued breastfeeding
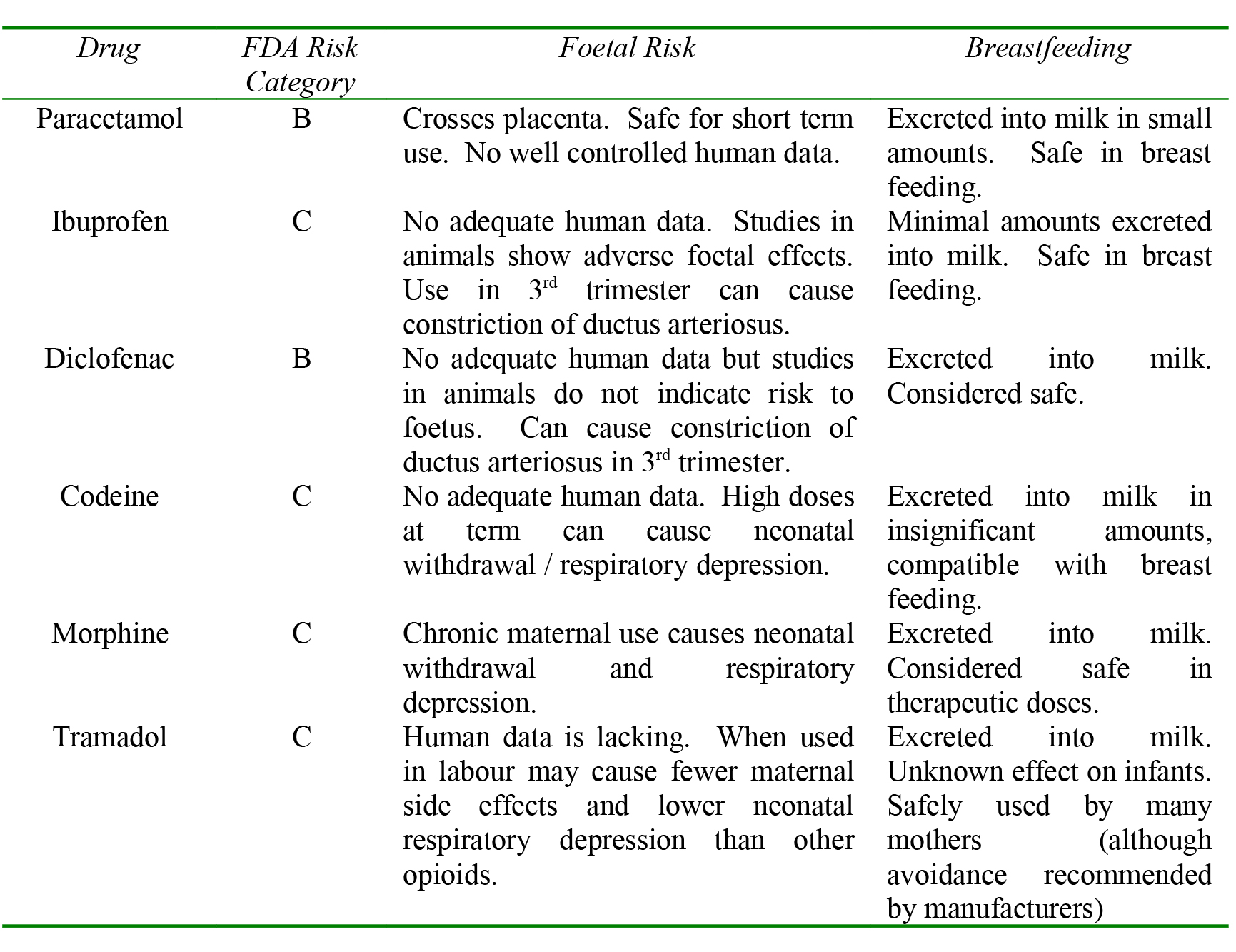
Table 2. Common analgesics used in pregnancy / puerperium.
Breast milk production is dependant on adequate maternal hydration and regular stimulation (either by the baby feeding or by the mother expressing). If scheduled for anaesthesia / surgery encourage the mother to breastfeed as near as possible to the procedure.
General anaesthesia
Propofol and thiopentone are found in breast milk in insignificant amounts, as are levels of volatile agents. As neuromuscular blocking agents are large, ionised and water soluble they are not excreted into breast milk. After general anaesthesia women can be advised to express and discard the first sample of milk and to resume infant feeding after this. Many argue that no portion of milk needs to be wasted. All of the commonly used antiemetics are advised to be used ‘with caution’ or ‘only if essential’ by manufacturers.
Regional anaesthesia
Local anaesthetics are not excreted into breast milk in amounts sufficient to be harmful. Therefore breast feeding can continue as normal after regional anaesthesia.
Analgesics
See above table for commonly used analgesics. The American Academy of Pediatrics (AAP) published a statement on drug transfer into human milk and possible effects on the infant. The AAP considers paracetamol, most non-steroidal anti-inflammatory drugs and morphine compatible with breastfeeding.
SUMMARY
Non-obstetric surgery during pregnancy is not uncommon and anaesthetists should be aware of the implications for management. The physiological changes of pregnancy need to be considered, especially the avoidance of aortocaval compression, antacid prophylaxis and adequate preoxygenation. The airway needs careful evaluation preoperatively.
The main risk to the foetus is asphyxia. This can be avoided by ensuring adequate maternal oxygenation and ventilation, avoiding hypotension and avoiding drugs that increase uterine tone. This should ensure adequate uteroplacental perfusion. Perioperative foetal heart rate monitoring may be useful if trained staff are available and it is practically possible. Regional anaesthesia is likely to have benefits over general anaesthesia. Attention should be paid to thromboprophylaxis, analgesia and signs of preterm labour in the postoperative period.
When caring for pregnant ladies undergoing non-obstetric surgery a multidisciplinary team is essential. This should include surgeons, anaesthetists, obstetricians, midwives, nurses and neonatologists where available. Elective surgery should be postponed until 6 weeks postpartum when possible. Nonelective surgery should be delayed until the 2nd trimester when organogenesis has occurred and the risk of teratogenicity decreases but this may not always be possible.
- Remember the physiological and anatomical changes of pregnancy
- Prevent foetal asphyxia by maintaining maternal oxygenation, ventilation and haemodynamic stability
- Remember postoperative thromboprophylaxis
ANSWERS TO QUESTIONS
1. FTFTF
2. FFFFT
3. FTFFT
REFERENCES / FURTHER READING
- Mhuireachtaigh RN, O’Gorman DA. Anesthesia in pregnant patients for nonobstetric surgery. Review Article. Journal of Clinical Anesthesia 2006; 18: 60-66.
- Van de Velde M, De Buck F. Anesthesia for non-obstetric surgery in the pregnant patient. Minerva Anestesiologica 2007; 73: 235-40.
- Walton NKD, Melachuri VK. Anaesthesia for non-obstetric surgery during pregnancy. Continuing Education in Anaesthesia, Critical Care and Pain 2006; 6: 83-85.
- Rosen MA. Management of Anesthesia for the Pregnant Surgical Patient. Anesthesiology 1999; 91: 1159-63.
- Heidemann BH, McClure JH. Changes in maternal physiology during pregnancy. Continuing Education in Anaesthesia, Critical Care and Pain 2003; 3: 65-68.



