Intensive Care Medicine
KEY POINTS
- Endovascular thrombectomy is indicated for anterior circulation stroke caused by large-vessel occlusion.
- Rapid assessment is vital: treatment should begin within 6 hours.
- ‘Time is brain’ is the mantra in treatment of acute ischaemic stroke.
- Arterial pressure should be monitored carefully during the procedure with hypotension treated aggressively.
- The ideal anaesthetic technique is currently an area of debate and research.
- Current focus is with the development of multidisciplinary thrombectomy pathways to improve workflow, safety, and rapid access to treatment.
INTRODUCTION
Acute ischaemic stroke is a life-threatening, devastating, disabling condition and is the world’s second-leading cause of death, estimated to cost the UK health service £3 billion per year with a further estimated £4 billion lost to the economy in productivity, disability, and informal care.1
Approximately 30% of patients die within a year of a stroke, with 50% of survivors experiencing a long-term disability. An analysis of patients from the third International Stroke Trial (IST-3) showed that just over one-third were alive and independent at 6 months.2 Patients presenting with a proximal, large-artery, occlusive stroke (30%-50%) account for a high proportion of the disability burden.
Among strokes, 85% are ischaemic as opposed to haemorrhagic. Vessel occlusion reduces perfusion and nutrient supply and causes hypoxia, leading to cell death. Treatment aims to achieve reperfusion by recanalising the occluded vessel. Evidencebased therapies include intravenous thrombolysis within 4.5 hours, aspirin therapy within 48 hours, hemicraniectomy in cases of malignant infarction, and dedicated management within an acute stroke unit.3
Unfortunately, only 20% of patients with ischaemic stroke are suitable for intravenous thrombolysis: contraindications include recent surgery, anticoagulation, and delayed presentation.1 Large-artery occlusion accounts for approximately 40% of ischaemic strokes, and these patients often present with extensive thrombus unresponsive to intravenous thrombolysis,
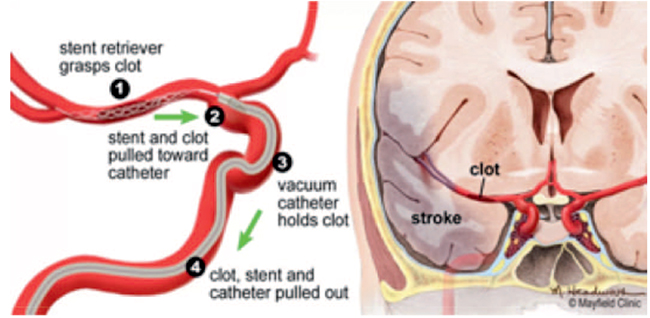
Figure 1. Endovascular thrombectomy illustration. Note the clot in the middle cerebral artery. A stent retriever mesh is embedded in the clot and then used to pull the clot out of the artery and into the vacuum catheter. Used with permission from MayfieldClinic.com. Image accessed at https://mayfieldclinic.com/pe-Stroke.htm.
increasing the probability of a large stroke and severe disability. In these cases, the success rate of intravenous thrombolysis has been quoted at less than 30%.4
Earlier trials focused on the use of interventional methods, such as catheter-directed thrombolysis, balloon angioplasty, and locally infused antispasmodic drugs, to treat strokes unresponsive to intravenous thrombolysis.5 No benefit was shown in ischaemic stroke.
More recent evidence demonstrates efficacy and establishes mechanical endovascular thrombectomy as the standard of care for acute ischaemic stroke causing large-vessel occlusion in the anterior circulation6 (Figure 1). One meta-analysis showed proportions of patients achieving an independent functional outcome as 46% in those who received mechanical thrombectomy versus 26% of those who received best medical treatment.4 Advances in retrievable stent technology (Figure 2), the universal use of vascular imaging (computed tomography [CT] angiography), and improvements in workflow patient selection leading to rapid door-to-recanalisation times might be responsible for this improvement.6
Patients with proximal occlusion of the internal carotid or middle cerebral arteries are most likely to benefit from endovascular thrombectomy. Of every 5 patients presenting with occlusion in the anterior cerebral circulation who undergo endovascular thrombectomy, one more will function independently at 3 months than if they had received intravenous thrombolysis alone and 1 in 3 will be less disabled (defined as being 1 point less on the modified Ranking disability scale).1
Rapid treatment is important: ‘time is brain’ in acute stroke treatment. One study identified a fall in benefit of 3.4% to 3.9% for every 1 hour of delay.1
The following tutorial describes the anaesthetic concerns and management of patients presenting with ischaemic stroke for endovascular thrombectomy.
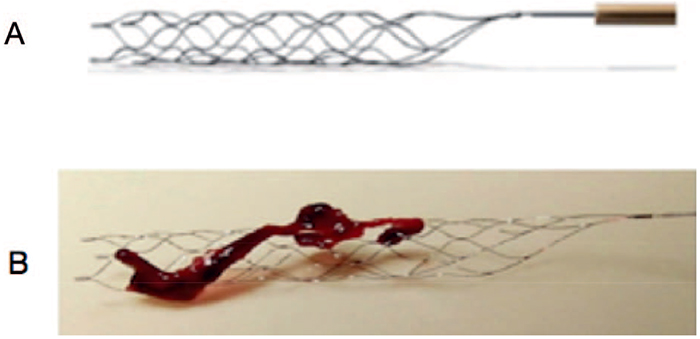
Figure 2. Third-generation stent retrieval devices. (A) Solitaire (Covidien). (B) Thrombus in stent strut. Images obtained under creative commons license reference: Kang, D. and Park, J. (2017). Endovascular Stroke Therapy Focused on Stent Retriever Thrombectomy and Direct Clot Aspiration : Historical Review and Modern Application. Journal of Korean Neurosurgical Society, 60(3), pp.335–347.
INDICATION
Indications for endovascular thrombectomy are likely to broaden in the future. The ESCAPE7 and REVASCAT8 trials included those patients presenting late for thrombectomy but with favourable profile on CT angiography. These trials suggest treatment may still be appropriate up to 24 hours after stroke onset in selected cases.
International guidelines recommend endovascular treatment as the standard of care for patients presenting with acute ischaemic stroke caused by large-vessel intracranial occlusion identified on vascular imaging.9
Intracranial vascular imaging in the form of CT with angiography is recommended for decision making and is useful for assessing collateral flow. Tandem occlusions such as extracranial internal carotid artery occlusion are often identified. Whilst there are no explicit recommendations for their management, interventional radiologists may choose to perform angioplasty or stent them at the time of thrombectomy to treat the primary lesion. Magnetic resonance imaging may play a future role in assessing ischaemic volume and salvageable tissue.4
The National Institute of Health Stroke Scale is a tool to quantify impairment caused by a stroke. It is composed of 11 items, each scoring between 0 and 4. Individual scores from each item are added to gain the total. A score of 0=no stroke symptoms, 1 to 4 = minor stroke, 5 to 15 = moderate stroke, 16 to 20 =moderate to severe stroke, and 21 to 42 = severe stroke.10
The UK National Clinical Guideline for Stroke (fifth edition, 2016) recommends the following:
- Patients should be considered for intra-arterial clot extraction (using stent retriever and/or aspiration techniques, with prior intravenous thrombolysis unless contraindicated), if they have a proximal intracranial large-vessel occlusion causing a disabling neurological deficit (National Institutes of Health Stroke Scale [NIHSS] score of 6 or more), and the procedure can begin (arterial puncture) within 5 hours of known onset.9
- Patients with acute ischaemic stroke causing a disabling neurological deficit (NIHSS score of 6 or more) may be considered for intra-arterial clot extraction (using stent retriever and/or aspiration techniques, with prior intravenous thrombolysis unless contraindicated) beyond an onset-to-arterial puncture time of 5 hours if:
- the large artery occlusion is in the posterior circulation, in which case treatment up to 24 hours after onset may be appropriate
- a favourable profile on salvageable brain tissue imaging has been proven, in which case treatment up to 12 hours after onset may be appropriate9 (now up to 24 hours may be appropriate post DAWN trial11)
Absolute contraindications to acute thrombectomy include the following12:
- Known severe iodinated-contrast allergy
- Severe coagulopathy
- Suspected subarachnoid haemorrhage
- Technical difficulty as determined by the neurointerventionist (e.g., tortuous vessels, unable to access the clot, location of the clot, chronic carotid occlusion
Relative contraindications include:
- Significant prestroke morbidity (not functionally independent or expected life expectancy > 6 months)
- Vascular access difficulty such as known large abdominal aortic aneurysm, aorto-iliac or femoro-popliteal bypass
- Greater than 6 hours since onset of symptoms to groin puncture (however, clinician discretion if favourable imaging profile)
- Therapeutic anticoagulation increases the risk of the procedure
- Renal disease—the use of contrast can worsen condition
The example below shows the revascularising effect of mechanical thrombectomy on middle cerebral artery occlusion (Figure 3).
PREPROCEDURAL ASSESSMENT
Thrombectomy is an emergency procedure, requiring rapid communication and smooth coordination between the stroke team, interventional radiologist, and anaesthetist. The anaesthetist may be part of the team from the outset or may be asked to assist in the event of a procedural complication.13,14
Preprocedural anaesthetic considerations include the following:
- Rapid and relevant preoperative assessment including level of consciousness, fasting status, allergies, airway assessment, and haemodynamic stability
- Advance planning in the event of an intraoperative complication, which may require intubation and/or transfer to the operating theatre
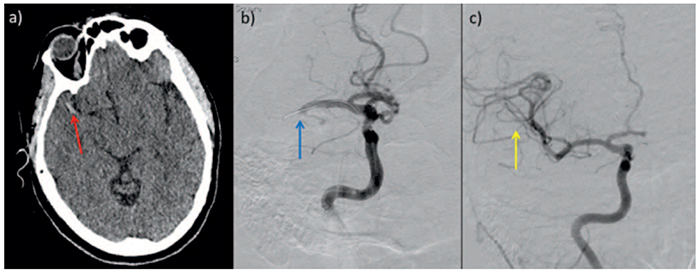
Figure 3. (a) Prethrombectomy. (b) Digital subtraction angiogram in a 49-year-old woman with sudden-onset left hemiparesis. (c) Postthrombectomy. The red arrow shows a hyperdense clot in the right middle cerebral artery (MCA). The blue arrow shows occluded right MCA with catheter passing through. The yellow arrow shows improved filling of the MCA. Postprocedure, the patient showed complete resolution of neurological symptoms.4 Image obtained under creative commons licence reference: Evans M, White P, Cowley P. et al. Revolution in acute ischaemic stroke care: a practical guide to mechanical thrombectomy. Pract Neurol 2017; 17: 252–265.
- Haemodynamic monitoring and vasopressor support to achieve blood pressure targets
- The anaesthetist also needs to consider the relatively less familiar location of the interventional radiology suite, the limitations in terms of both physical space and range of anaesthetic equipment, and medications and the need for protective lead clothing13,14
As mechanical thrombectomy is an emergency procedure that requires precise and rapid cooperation between several specialties, clear and accurate communication is vital to procedural success. The preprocedure safety checklist is an important component of this. This could be a modified World Health Organization checklist, although some units have developed their own (Figure 4).
THROMBECTOMY PROCEDURE
Endovascular thrombectomy is a catheter-based intervention using stent retriever devices that are self-expanding and resheathable. They are able to firmly engage the clot in a straight position. They avoid the disadvantages associated with permanent stent implantation such as risk of stent thrombosis, stenosis, and requirement for dual antiplatelet therapy.15
Stent retrievers vary in terms of material and design of the proximal and distal stent opening (e.g., closed basket-like ends).
More modern devices show better revascularization and reduced intracranial haemorrhage when compared with the earlier examples.15
An example of an approach to the procedure is shown in figure 5.
Although there is little evidence to guide management in cases in which a stenosed carotid artery makes access to the clot difficult, the neurointerventionalist may need to perform angioplasty to circumvent this problem.4
If a stent is left in the carotid artery, current recommendations are for dual antiplatelet therapy for 3 to 6 months, the timing of which is coordinated by the stroke team.14 Dual antiplatelet therapy could exacerbate haemorrhagic complications, but this is offset by the higher recanalisation rates and reduced mortality that have been reported in cases in which stents have been deployed for this purpose.4
PERIOPERATIVE ANASTHESIA MANAGEMENT
Standard anaesthetic monitoring comprising electrocardiogram, noninvasive blood pressure, and pulse oximetry is established. Temperature monitoring is routine if general anaesthesia is required. A urinary catheter is not essential and may delay the procedure start time.
Haemodynamic Goals
Invasive arterial blood pressure monitoring to target haemodynamic goals is useful, but placement must not delay the thrombectomy procedure. The femoral sheath (inserted by the interventional radiologist) waveform can be transduced if one is being used.
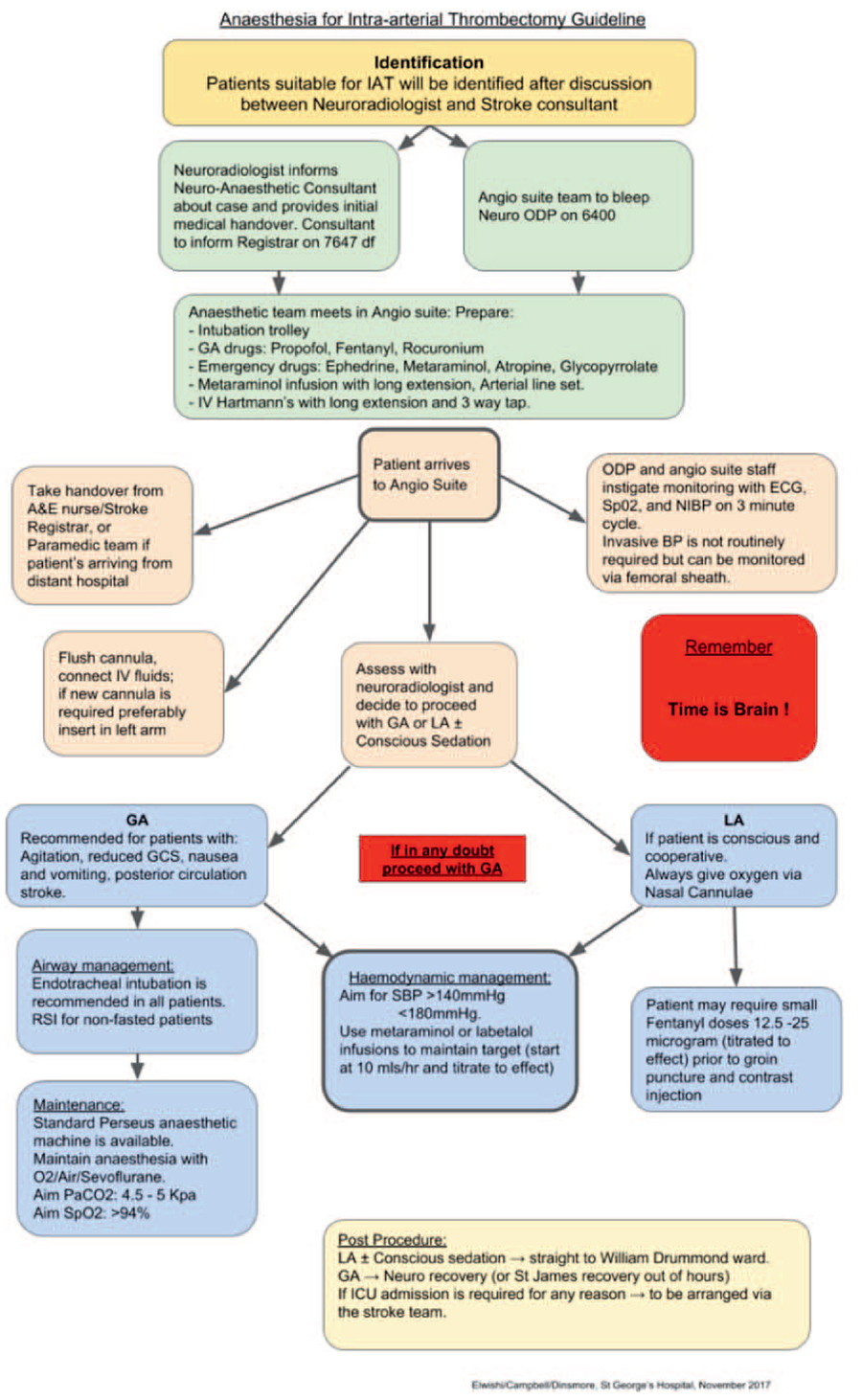
Figure 4. Example an algorithm that details a checklist and suggested workflow for patients undergoing endovascular thrombectomy. ODP, operating department practitioner. Reproduced with permission from St George’s University Hospital NHS Foundation Trust, London.
Sixty percent of patients present with elevated arterial pressures. This may be due to existing essential hypertension, the neuroendocrine stress response, or a Cushing response to cerebral oedema or ischaemia.
Both high and low blood pressures are associated with higher rates of death and dependency. A balance exists between excessive hypertension contributing to an increased intracranial haemorrhage risk and cerebral oedema versus compromised cerebral perfusion to the ischaemic penumbra with an inappropriately low mean arterial pressure.13
Initial haemodynamic goals aim to maintain the patient’s systolic blood pressure above 140 mm Hg with fluid and vasopressors. A paper by Whalin in 2017 suggested aiming for a target of within 10% of the patient’s normal mean arterial pressure.16 Systolic blood pressure should be kept at less than 180 mm Hg with or without the administration of intravenous thrombolysis. Diastolic
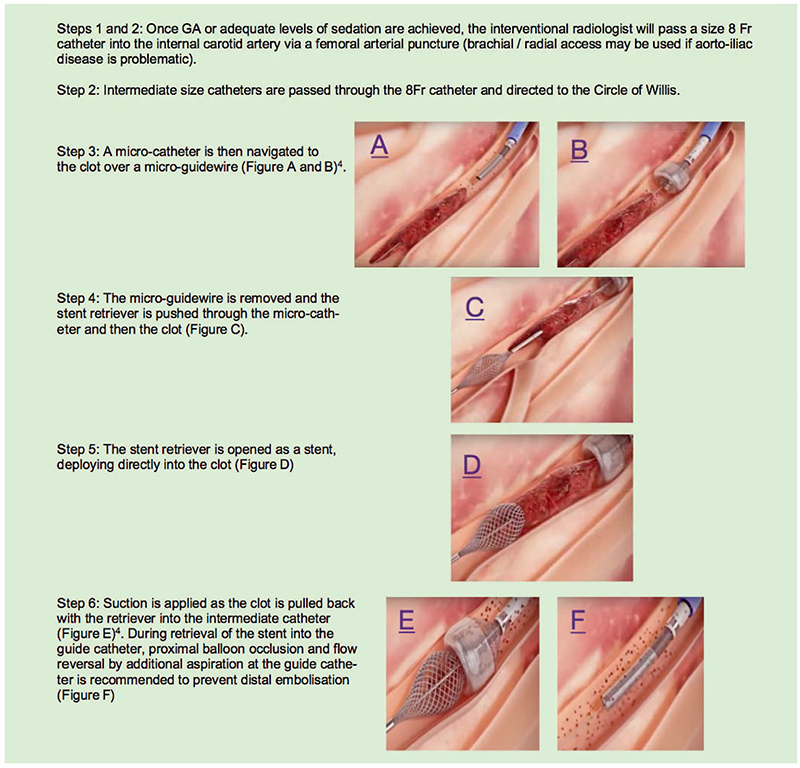
Figure 5. Endovascular thrombectomy illustration using the Megavac system: steps 1 to 4, initial wire placement using the delivery system, passage of catheter, and stent retriever through thrombus with deployment of stent retriever into thrombus. Step 5, retrieval of thrombus and stent into guide catheter applied with suction. Step 6, restoration of blood flow in vessel. Images obtained under creative commons license from Capture vascular http://www.capturevascular.com. Accessed at Link: https://www.youtube.com/watchv=9Yxu4L2klHQ&t=13s.
pressure should be kept at less than 105 mm Hg. After recanalization, blood pressure targets can be adjusted to prevent haemorrhagic transformation. If the procedure is unsuccessful, the systolic blood pressure should be maintained at greater than 140 mm Hg.12
General Versus Local Anaesthesia
The procedure can be performed under general or local anaesthesia. General anaesthesia provides patient immobility for the operator, control of pain and agitation, plus definitive airway protection. However, most procedures can be performed under local anaesthesia with or without conscious sedation, which allows continuous monitoring of neurological changes with smoother haemodynamics and perceived reduction in ‘door-to-needle’ time.4,13,14
The downsides to local anaesthesia are the lack of airway protection and uncontrolled pain and agitation should the procedure time be longer than 1 to 2 hours. Indications for general anaesthesia include the following4,13,14:
- Reduced level of consciousness
- Inability to protect airway, evidence of aspiration, or hypoxia
- Signs of brainstem dysfunction
- Bulbar palsy
- Agitation or inability to lie flat due to cardiac or respiratory disease2
Anaesthetic technique is currently an area of debate. Previous studies have shown general anaesthesia to be associated with increased case fatality and length of stay when compared with local anaesthesia.17 It is important to note that this is an association rather than proven causation: a study in 2010 documented higher NIHSS scores in patients who went on to receiving general anaesthesia.18 General anaesthesia (or perhaps the need for it) was cited as an independent predictor of poor outcome. Local anaesthesia without sedation was associated with a 60% chance of good outcome as opposed to 15% in the general anaesthesia group. Good outcomes were associated with a systolic blood pressure greater than 140 mm Hg, whilst a correlation was noted between low systolic blood pressure and general anaesthesia.
As with many other procedures performed in ill patients, it can be difficult to attribute general anaesthesia as an independent predictor of adverse outcome when looking at retrospective studies. In most studies, comparison is binary: simply comparing general versus local anaesthesia without looking at varying practice in terms of sedation depth or conversion to general anaesthesia as a result of complications. Bias is easily introduced in retrospective studies via local policy and operator preference.
It is important to also note that general anaesthesia maybe selected in the ‘sicker’ patients presenting with severe neurological dysfunction, hypotension, or signs of aspiration. These patients had higher baseline NIHSS scores with low baseline arterial pressures.18 General anaesthetic patients were also observed in one centre to take longer to arrive in theatre, with lower arterial pressure and fluctuations noted throughout the procedure.13
More recent evidence has shown no difference in early outcomes, in relation to NIHSS scores, from general anaesthesia with intubation versus conscious sedation. In 2017, the GOLIATH and ANSTROKE studies reported general anaesthesia and conscious sedation to be equally safe.4
Continued improvement in procedure technique, patient pathways, stent retriever technology, and experience of clinical teams may influence future outcomes. There are ongoing trials of general anaesthesia versus conscious sedation that aim to guide best practice. Until then, a technique tailored to the individual patient and clinical circumstances is probably the most prudent.
For general anaesthesia, induction and choice of maintenance agent depend on the anaesthetist. Analgesic requirements for the procedure are low because of the minimally invasive nature, and long-acting opioids are avoided to aid a rapid neurological assessment after emergence.13,14 Maintenance can be via inhalational agents (where scavenging facilities are available) or total intravenous anaesthesia. Both result in rapid recovery, which is important for postprocedure neurological assessment.
For a local anaesthetic technique, wound infiltration can be accompanied by incremental fentanyl and midazolam as required for sedation. Low-dose target-controlled infusions of propofol, remifentanil, or dexmedetomidine are suitable alternatives for conscious sedation. Some patients complain of a headache during the procedure, which may be due to movement of the catheter, distension of vascular structures at clot retrieval, or injection of contrast. Low-dose remifentanil can provide a powerful analgesic effect and has the advantage of maintaining conscious level and having a rapid offset.
Postoperative Care
Ultimately, neurological recovery is dependent on recanalization, and if successful, neurological recovery is often immediate once sedation is reduced. If neurological function is acceptable postprocedure, most patients can recover in the hyperacute stroke unit following an uncomplicated intervention under local anaesthesia with minimal sedation.12 The patient is likely to require level 2 or 3 care if general anaesthesia has been required or if the procedure has been prolonged or complicated. Emphasis is likely to be on a prompt sedation hold and early extubation where possible. There may be ongoing vasopressor requirements or the need for antihypertensive drug infusions such as labetalol to achieve haemodynamic goals.13,14 Patients can restart enteral antihypertensive medication within 48 to 72 hours.14
Postoperative care should include regular inspection of the arterial puncture site. A repeat head CT should be organised within the first 24 hours to exclude haemorrhage. Aspirin and low-molecular-weight heparin are withheld for 24 and 48 hours, respectively. If a stent has not been used and there is no intracranial haemorrhage on follow-up CT, 300 mg of aspirin is given for up to 2 weeks and then continued as secondary prevention.4 If a stent is left in situ, dual antiplatelet therapy with clopidogrel and aspirin is started and continued for 3 to 6 months with a single agent used for long-term secondary prevention.4 Other oral anticoagulants may be considered where indicated (eg, atrial fibrillation). The stroke team will generally direct acute and ongoing administration of antiplatelets or oral anticoagulation.
If the procedure is successful, blood pressure targets can be allowed to relax toward their normal range: 140 to 160 mm Hg is acceptable. If recanalisation is unsuccessful, blood pressure should be maintained at greater than 140 mm Hg and less than 180 mm Hg, and vasopressor or labetalol infusions maybe required to achieve this.12
CONCLUSIONS
Endovascular thrombectomy is considered the gold standard treatment for acute ischaemic stroke caused by large-vessel occlusion in the anterior circulation. Stent technology and experience with the technique continue to progress with expansion of hyperacute stroke services. Indications for the procedure are likely to broaden in the future.
Knowledge surrounding indications for the procedure is valuable and relevant to the anaesthetist and neurointensivist providing emergency perioperative care in neurosurgical centres.
Because of the current geographical locations of neurosurgical services in the United Kingdom, an urgent transfer model analogous to that for neurosurgical emergencies is likely to develop.4 As availability of CT angiography increases, anaesthetists and intensivists outside tertiary centres may be required to intubate, stabilise, and start thrombolysis for patients who present with severe neurological disability prior to transfer. Knowledge of the referral pathways involved is useful to ensure patients are transferred in a timely manner.
Debate continues about appropriate anaesthetic technique. Until more evidence is available, the technique most suitable to the individual patient based on risk assessment should be chosen. Focus should remain on rapid workflow with aggressive management of haemodynamic goals.
Mechanical thrombectomy is an innovative, time-sensitive, multispecialty procedure with real potential to improve patient outcomes. The anaesthetist has a vital role in ensuring adequate and safe intraoperative and perioperative care of these patients.
REFERENCES
- NHS England. Evidence review: mechanical thrombectomy for acute ischaemic stroke in the anterior cerebral Circulation. https://www.engage.england.nhs.uk/consultation/clinical-commissioning-consultation-may-2017/user_uploads/mechanicalthrombectomy-policy-proposition.pdf. Accessed on Nov 3, 2017.
- The IST-3 Collaborative Group. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6h of acute ischaemic stroke (the third International Stroke Trial [IST-3]): a randomized controlled trial. Lancet. 2012;379:2352-2363.
- National Institute for Health and Clinical Excellence. Mechanical Clot Retrieval for Treating Acute Ischaemic Stroke. Interventional Procedures Guidance. London, UK: National Institute for Health and Clinical Excellence. https://www.nice.org.uk/guidance/ipg548/chapter/3-The-procedure. Accessed July 14, 2017.
- Evans M, White P, Cowley P, et al. Revolution in acute ischaemic stroke care: a practical guide to mechanical thrombectomy. Pract Neurol. 2017;17:252-265.
- Higashida R, Halbach V, Tsai F, Dowd C, Hieshima G. Interventional neurovascular techniques for cerebral revascularization in the treatment of stroke. Am J Roentgenol. 1994;163(4):793-800.
- Boyle K, Joundi RA, Aviv RI. An historical and contemporary review of endovascular therapy for acute ischemic stroke. Neurovasc Imag. 2017;3(1):1.
- Goyal M, Demchuk AM, Menon BK, et al; ESCAPE Trial Investigators. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019-1030.
- Molina CA, Chamorro A, Rovira A, et al. REVASCAT: a randomized trial of revascularization with Solitaire FRt device vs. best medical therapy in the treatment of acute stroke due to anterior circulation large vessel occlusion presenting within eight-hours of symptom onset. Int J Stroke. 2013;10:619-626.
- Royal College of Physicians, Intercollegiate Stroke Working Party. National Clinical Guideline for Stroke. 5th ed. 2016. https://www.strokeaudit.org/SupportFiles/Documents/Guidelines/2016-National-Clinical-Guideline-for-Stroke-5t-(1).aspx. Accessed August 10, 2017.
- Wikipedia. National Institutes of Health Stroke Scale (NIHSS). https://en.wikipedia.org/wiki/ National_Institutes_of_Health_Stroke_Scale#cite_note-SST-3. Accessed July 10, 2017.
- Nogueria RG, Jadhav PA, Haussen DC, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378:11-21.
- White PM, Bhalla A, Dinsmore J, et al. Standards for providing safe acute ischaemic stroke thrombectomy services. Clin Radiol. 2015;72:175e1-175e9.
- Anastasian ZH. Anaesthetic management of the patient with acute ischaemic stroke. Br J Anaesth. 2014;113:9-16.
- Dinsmore J, Elwishi M, Kailainathan P. Anaesthesia for endovascular thrombectomy. BJA Educ. 2018;18(10):291-299.
- Morasini P, Subler C, Schroth G, Gralla J. Thrombectomy for acute ischaemic stroke treatment: a review. EJMINT. 2012:1238000077. http://www.ejmint.org/invited-review/1238000077. Accessed June 20, 2017.
- Whalin MK, Halenda KM, Haussen DC, et al. Even small decreases in blood pressure during conscious sedation affect clinical outcome after stroke thrombectomy: an analysis of hemodynamic thresholds. Am J Neuroradiol. 2017;32:294-298.
- Bekelis K, Missios S, MacKenzie TA, et al. Anaesthesia techniques and outcomes of mechanical thrombectomy in patients with acute ischaemic stroke. Stroke. 2017;48(2):361-366.
- Jumaa MA, Zhang F, Ruiz-Ares G, et al. Comparison of safety and clinical and radiographic outcomes in endovascular acute stroke therapy for proximal middle cerebral artery occlusion with intubation and general anaesthesia versus the nonintubated state. Stroke. 2010;41(6):1180-1184.



