Regional Anaesthesia
KEY POINTS
- Classically, the brachial plexus originates from five ventral rami, C5-T1, which then form trunks, division and cords before terminating into individual nerves to supply the upper limb.
- It is not clear whether a soft tissue sheath surrounds the brachial plexus and if so, the nature and composition of the sheath.
- Anatomical variation of the brachial plexus is common and can influence the conduct of regional anaesthesia.
INTRODUCTION
The brachial plexus (BP) consists of a network of nerves whose function is to provide the motor, sensory and sympathetic innervation of the upper limb. In 1884 Halstead first reported the use of cocaine to block the BP.1 Successful BP blockade requires thorough knowledge of the anatomy and variations of the brachial plexus. As Alon Winnie, a prominent anaesthesiologist, once said regional anesthesia is ‘an exercise in applied anatomy.’ In this tutorial, the classical anatomy of the BP will be described. Anatomical variations of the BP will be subsequently explored and the associated clinical implications discussed.
EMBRYOLOGICAL DEVELOPMENT
In the fourth week of development, the first differentiation of the mesenchyme takes place.1 The primordia of the dorsal nerves ends up at the height of the distal end of the humerus in the sheath of the forming primordia arm muscles. On day 32, extensions of nerves from C5-T1 are formed and on day 33, the nerves merge and begin forming the BP. Between the 39th and 40th day, the median, radial and ulnar nerves reach the level of the hand. A similar arrangement and orientation of the BP to that in adults is observed on the 49th and 50th day.
CLASSICAL ANATOMY OF THE BRACHIAL PLEXUS
The BP originates just outside of the intervertebral foramina at the lower cervical region as five roots, formed from the five ventral rami of C5-8 and T1 spinal nerves (Figure 1).2,3,4 Near the medial border of the middle scalene muscle, the C5 and C6 rami unite to form the superior trunk, the C7 ramus continues as the middle trunk and the C8 and T1 rami unite to form the inferior trunk. The roots and trunks pass through the interscalene groove, a palpable surface anatomical landmark situated between the anterior and middle scalene muscles (Figure 2).3
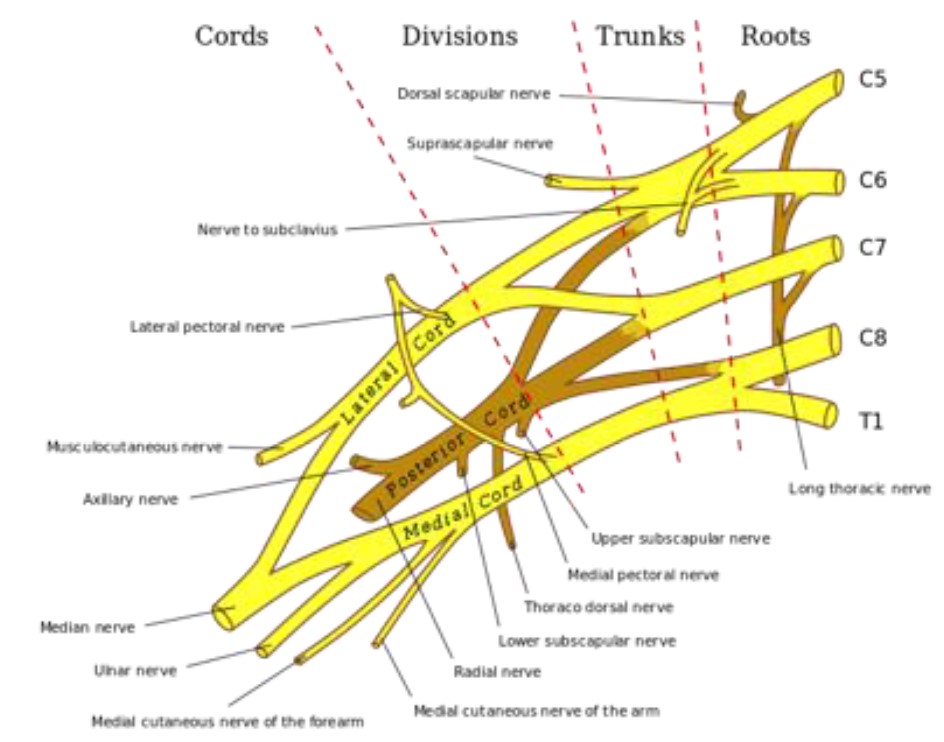
Figure 1. Anatomical illustration of the brachial plexus. Adapted from Gray’s Anatomy, taken from Wikipedia.
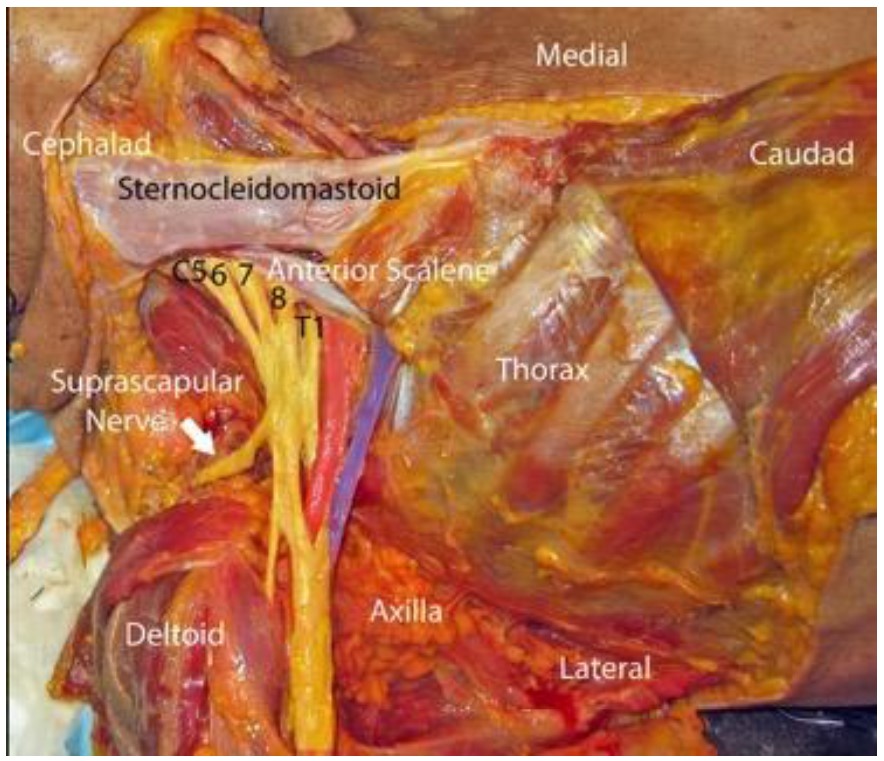
Figure 2. Dissection of cadaver which demonstrates the brachial plexus (yellow) exiting behind the anterior scalene muscle. The subclavian artery and vein are highlighted in red and blue, respectively. From Grant SA, David BA. Ultrasound guided regional anesthesia. 2nd edn. New York: Oxford University Press, 2016. Copyright © 2016 by Oxford University Press. By permission of Oxford University Press, USA. This image is not covered by the terms of the Creative Commons license of this publication. For permission to reuse, please contact the rights holder.
As the trunks pass posterior to the clavicle, each trunk bifurcates into an anterior (flexor) and posterior (extensor) division at the lateral border of the first rib. Divisions then reunite into cords, which are defined by their spatial relationship to the second part of the axillary artery.3 The lateral cord is formed by the anterior divisions of the superior and middle trunks, the medial cord is formed by the anterior division of the inferior trunk and the posterior cord is formed by the posterior divisions of all three trunks. Functionally, the lateral cord is the cord of the proximal flexors, the medial cord is the cord of the distal flexors of the forearm, wrist and hand and the posterior cord supplies all the extensor muscles of the upper limb.
In the lower part of the axilla, the cords divide and give rise to the five terminal branches of the plexus. The lateral cord splits into the musculocutaneous nerve (C5-7) and the lateral ramus of the median nerve and the medial cord splits into the ulnar nerve (C8-T1) and medial ramus of the median nerve. Both the lateral cord and medial cord thus form the median nerve (C5-T1). Last, the posterior cord splits into the axillary nerve (C5, 6) and the radial nerve (C6-T1).2,4 In the base of the axilla, the axillary artery is positioned in a characteristic location relative to the terminal nerves of the BP, anterior to the radial nerve, posteromedial to the median nerve and posterolateral to the ulnar nerve.3
PRE-TERMINAL BRANCHES OF THE BRACHIAL PLEXUS
Above the clavicle, branches of the BP are the dorsal scapular nerve (C5), suprascapular nerve (C5-6), nerve to subclavius (C5-6), long thoracic nerve (C5-7) and the branches to the longus colli and scaleni muscles (C5-8). Pre-terminal branches from the cords include the lateral pectoral nerve (C5-7) from the lateral cord; medial pectoral nerve (C8-T1), medial antebrachial cutaneous nerve (C8-T1), medial brachial cutaneous nerve (C8-T1), and upper and lower subscapular nerves (C5-6) from the medial cord; and thoracodorsal nerve (C5-7) from the posterior cord (Figure 3).4
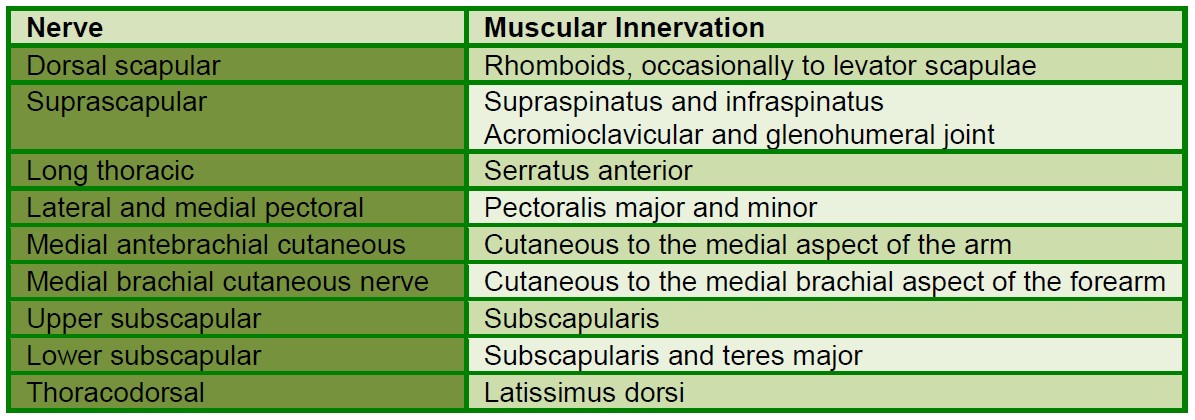
Figure 3. Innervation of the pre-terminal branches of the brachial plexus
SHEATH OF THE BRACHIAL PLEXUS: FACT OR FICTION?
Though the BP itself is well characterised, the architecture of the tissues surrounding it is not fully understood.3 Controversy still remains concerning whether a fibrous sheath or rigid anatomical tunnel exists around the BP. Multiple studies have demonstrated conflicting findings. In one, computerised axial tomography was used to examine the distribution of dye associated with catheter injection in the sciatic nerve, where it is generally agreed that there is no enveloping fibrous sheath, compared to the BP.5 No differences were found in the distribution of dye which suggested that the BP lies in the tissue plane between rigid anatomical structures that form the boundaries of the anatomical axilla: the clavicle, scapula, chest wall and humerus. Further research has demonstrated no evidence of a substantial sheath on cytomicrotome sections of the supraclavicular region.3 On the other hand, consistent with the results of other studies,6,7 systematic dissections on cadavers revealed a fibrous sheath around the neurovascular bundle of the BP which was visible to the naked eye in every dissection.8 The sheath was one to two millimeters thick, continuous from the neck to the distal end of the axilla and was filled with loose connective tissue and variable amounts of fat. Injection of saline results in expansion of the sheath which was held until the sheath was incised.
Both an enveloping fibrous sheath and a more rigid axillary tunnel are consistent with the clinical observation that local anaesthetic is more likely to spread longitudinally than circumferentially.3 Comparison of intra-plexus and peri-plexus injections for interscalene regional anaesthesia showed no difference in block onset times or quality.9 If a BP sheath were to exist, this could be explained by local anaesthetic readily diffusing across it. In the supraclavicular region, a hyperechogenic structure can be visualised on ultrasound and is thought by some authors to represent the BP sheath. Injection of local anaesthetic deep to this sheath resulted in a faster onset of surgical anaesthesia and prolonged duration of postoperative analgesia than injection superficial to the sheath.10
ANATOMICAL VARIATION OF THE BRACHIAL PLEXUS
Anatomical variations in the pattern of the BP are due to abnormal formation in the development of the trunks, divisions or cords and can be explained through neuronal growth cones.11 Guidance of developing axons is co-ordinated and regulated by the expression of chemoattractants and chemorepulsants. Any alterations in the signalling between the mesenchymal cells and the neuronal growth cones or the circulatory factors at the time of development of the BP can lead to significant variations.
Dissection of cadavers has demonstrated seven major configurations of the BP, none having more than 57% representation (Figure 4).12 Intra-individual variation also exists and right and left anatomical asymmetry was found in 61% of cadavers which correlates with clinical findings.
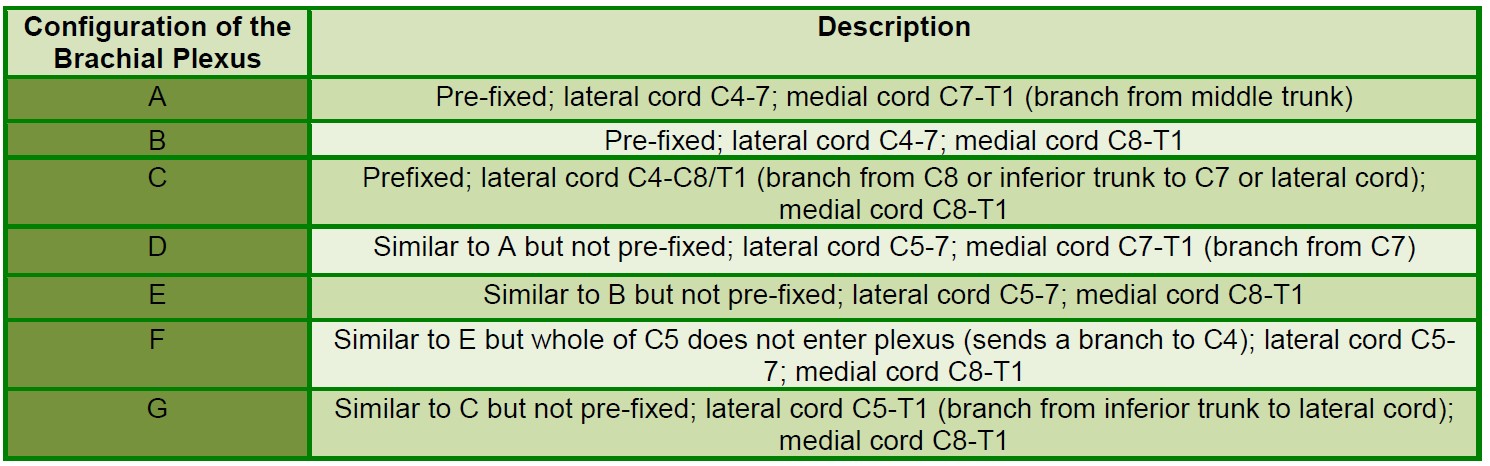
Figure 4. Description of the seven major configurations of the brachial plexus
PRE- and POST-FIXED PLEXUS
In a cadaveric study, 17.5% of the BPs examined were pre-fixed where the most superior root of the plexus is C4 rather than C5 and the plexus lies more cephalad than normal (Figure 5).13 Post-fixed BPs are more unusual and were found in 7.5% of cadavers. In a post-fixed BP the most inferior root of the plexus is T2 rather than T1 and the plexus lies more caudad than normal (Figure 6). Such anatomical variation could be clinically significant as any longitudinal shift of the BP may result in aberrant motor and/or sensory innervation of the upper limb.14 Of note however, it is not possible to identify either pre- or post-fixed BPs on ultrasound and, even if these anatomical variations were recognized, how the technique of interscalene block should be changed, if at all, is not known. In summary, it is unknown whether it significantly impacts upon the successful provision of upper extremity regional anaesthesia.3
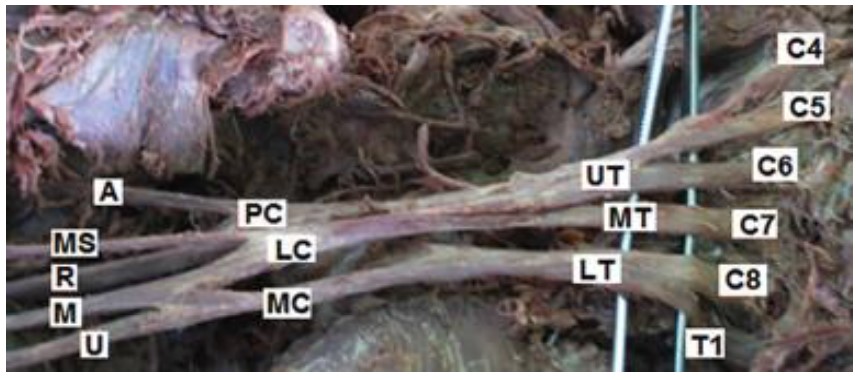
Figure 5. Cadaveric dissection showing a pre-fixed brachial plexus originating from the ventral rami of C4 to T1. From Guday E, Bekele A, Muche A. Anatomical study of prefixed versus postfixed brachial plexuses in adult human cadaver. ANZ J Surg 2016 Apr 12; doi: 10.1111/ans.13534 [ePub ahead of print]. Copyright © 2016 by John Wiley & Sons, Inc. Reprinted by permission of John Wiley & Sons, Inc. This image is not covered by the terms of the Creative Commons license of this publication. For permission to reuse, please contact the rights holder.
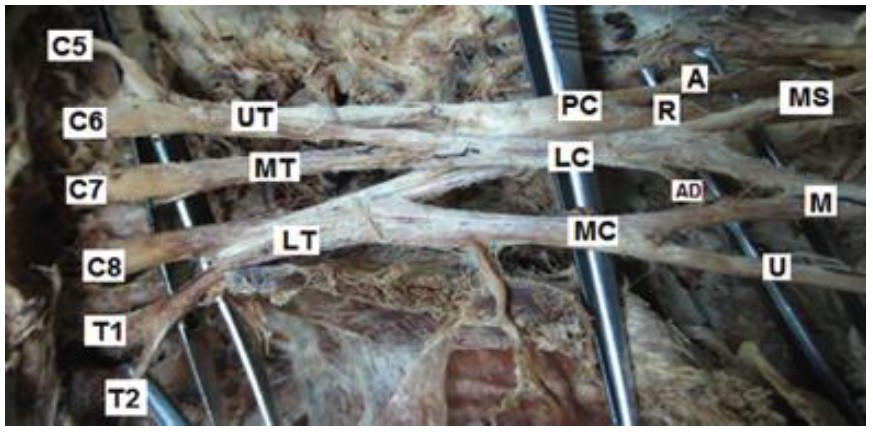
Figure 6. Cadaveric dissection showing a post-fixed brachial plexus originating from the ventral rami of C5 to T2. From Guday E, Bekele A, Muche A. Anatomical study of prefixed versus postfixed brachial plexuses in adult human cadaver. ANZ J Surg 2016 Apr 12; doi: 10.1111/ans.13534 [ePub ahead of print]. Copyright © 2016 by John Wiley & Sons, Inc. Reprinted by permission of John Wiley & Sons, Inc. This image is not covered by the terms of the Creative Commons license of this publication. For permission to reuse, please contact the rights holder.
VARIATIONS AT THE LEVEL OF THE TRUNKS
Incidence of anatomical variations at this level is between 13-35%. The ventral rami of C5 and C6 and the superior trunk are classically found in the interscalene groove but can instead pass through the anterior scalene muscle or anterior to it (25%).2,15 An inferior trunk may not form (9%) which is more frequent than the absence of the upper trunk (1%) (Figure 7). If a nerve stimulator is used to localise the BP at the interscalene level, stimulation of the phrenic nerve is usually thought to represent a too anterior orientation of the needle. An accessory phrenic nerve is present in up to 75% of individuals and runs with the nerve to subclavius.15 Stimulation of this accessory phrenic nerve could mislead the clinician in the interpretation of local anatomy. Another described variation that may have similar consequences is the phrenic nerve arising entirely from the BP.
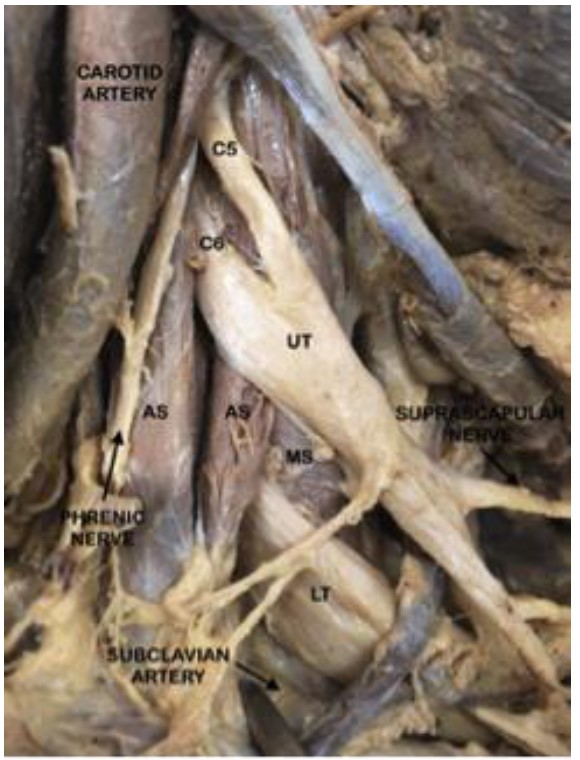
Figure 7. Cadaveric dissection showing a two trunked brachial plexus. Upper trunk (UT) is formed by the ventral rami of C5 and C6 and lower trunk (LT) by the ventral rami of C7 to T1. UT seen to emerge through anterior scalene (AS) muscle while LT passes through the interscalene groove between the AS and middle scalene (MS) muscle.
Nerve stimulation does not allow clinicians to account for and adapt to the presence of anatomical variations. Ultrasound on the other hand facilitates real-time visualisation, recognition of any anatomical variants and modification of a block technique based on the visualised anatomical variation. In the case where all the nerve roots and trunks are not found to pass between anterior and middle scalene muscles on ultrasound, the interscalene block can be successfully completed by injecting anaesthetic in the interscalene groove as well as in areas adjacent to the variant roots. In an ultrasound guided supraclavicular BP block, the superior trunk was noted to be medial to the subclavian artery whereas the middle and inferior trunks were in the usual location lateral to the subclavian artery.16 Once this had been recognised, the technique was modified by performing two injections, one medial and the other lateral to the subclavian artery with resultant complete sensory and motor block in the relevant dermatomes and myotomes.
VARIATIONS AT THE LEVEL OF THE DIVISIONS
Anatomical variations at this level are present in 33.6% of those studied, with 85% of these associated with an anterior division of middle trunk (ADMT).1 ADMT variant 1 is the most frequent (15%) and consists of an additional connection of the ADMT with the medial root of the median nerve. ADMT can connect with the medial cord, lateral or both roots of the median nerve or can give rise to the lateral root of the median nerve with no connection to the lateral cord which is then formed solely by the anterior division of the upper trunk.
VARIATIONS AT THE LEVEL OF THE CORDS
Multiple variations in the formation of the cords of the BP have been noted. The ventral ramus of T1 can fail to contribute to the posterior cord and it may provide the sole contribution to the medial cord.15 It is not uncommon for the posterior cord not to form, in which case the posterior divisions diverge to directly give rise to the branches and terminal nerves. A pair of cords, one small and one large, can replace the usual pattern of three cords. Cases of formation of a single cord have even been reported. Significant variation has been described in the origin of the branches of the BP too (Figure 8).17
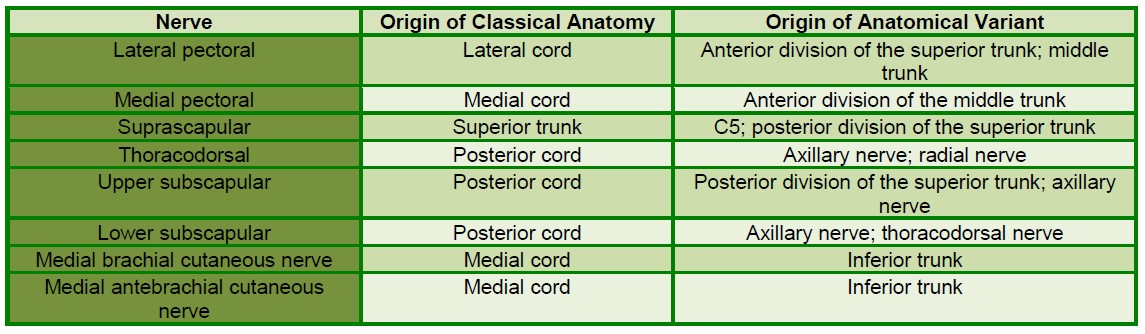
Figure 8. Anatomical variations in the origin of the branches of the brachial plexus. Adapted from Fazan VPS, Amadeu ADS, Caleffi AL, Filho OAR. Brachial plexus variations in its formation and main branches. Acta Cir Bras 2003; 18: 14-8. This content is covered by the terms of a Creative Commons Attribution License which can be found at: https://creativecommons.org/licenses/by/4.0/deed.en.
Normally, the three cords of the BP encircle the axillary artery but, in some cases, all of these cords can lie lateral to the axillary artery. Clinically, if this anatomical variation is visualised prior to an infraclavicular block, the anaesthetist could insert the needle lateral to the axillary artery and entirely avoid the artery.
VARIATIONS AT THE LEVEL OF THE AXILLA
The BP demonstrates a constant relationship to certain vessels which can be explained from a embryological perspective.18 Usually the axillary artery, for example, is considered to be the continuation of the seventh intersegmental branch of the dorsal aorta. If however it is derived from the sixth, eighth or ninth intersegmental branch of the dorsal aorta, as it sometimes is, the relationship between the axillary artery and BP is correspondingly altered.
In an ultrasound study which evaluated the arrangement of the median, ulnar, radial and musculocutaneous nerves around the axillary artery, ten different arrangements of the four nerves were found (Figures 9 and 10).19 In all cases, the four nerves were found in the same clockwise order (median, ulnar, radial and musculocutaneous) around the axillary artery. The classical anatomical picture was present in only 64.7%. An accessory axillary artery, running parallel to the axillary artery, was observed in 2.6% of patients.
Classically, the musculocutaneous nerve is described as lying in the coracobrachialis muscle or between the coracobrachialis and biceps muscles at the level of axillary block. Ultrasound has been used to demonstrate that, in fact, the musculocutaneous nerve is atypical in position in 22% of axillary blocks.20 It may be near the axillary artery or more frequently joined with the median nerve. If joined to the median nerve, it can run distally for a variable distance before separating from it. Notably, in cadaveric dissections, the musculocutaneous nerve can be absent in 8%, with the innervation of the biceps and brachialis provided instead by branches of the median nerve. A single axillary vein was observed in 42% of patients, two veins in 38%, three veins in 18% and four veins in 2%.
In these two described ultrasound studies, the incidence of anatomical variation was different to that previously reported from the results of anatomical dissection.19,20 Differences may be due to fat removal, muscle rigidity, vessel flattening or the position of the arm in anatomical dissections though in ultrasound studies the nerves can be found to move over each other when light to moderate pressure is applied to the probe.
In view of these possible anatomical variations, the axillary block procedure must be modified to accommodate them. Nerves around the axillary artery can be individually traced with ultrasound as they course distally from the axilla to confirm their nature, identity and relationship. In the case where the musculocutaneous nerve does not lie in its classical location, ultrasound guidance can be used to locate the aberrant nerve so that it may be blocked separately at its new location. Moreover, in the case where the musculocutaneous nerve fuses with the median nerve, there is potentially no need for an additional anaesthetic injection since the target nerve, the musculocutaneous nerve, is ensheathed along with the other nerves of interest for the axillary block.
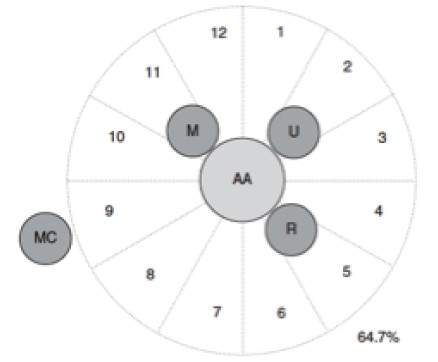
Figure 9. Schematic drawing of the most common arrangement of four nerves of the brachial plexus (M, median nerve; U, ulnar nerve; R, radial nerve; MC, musculocutaneous nerve) around the axillary artery (AA). Frequency of this topographic pattern given in percentage. J.-L. Christophe, et al. Assessment of topographic brachial plexus nerves variations at the axilla using ultrasonography. Br J Anaesth 2009; 103 (4): 606-612. doi: 10.1093/bja/aep207. Reproduced with permission of Oxford University Press on behalf of The British Journal of Anaesthesia Ltd. All rights reserved. This image is not covered by the terms of the Creative Commons licence of this publication. For permissions, please contact journals.permissions@oup.com.
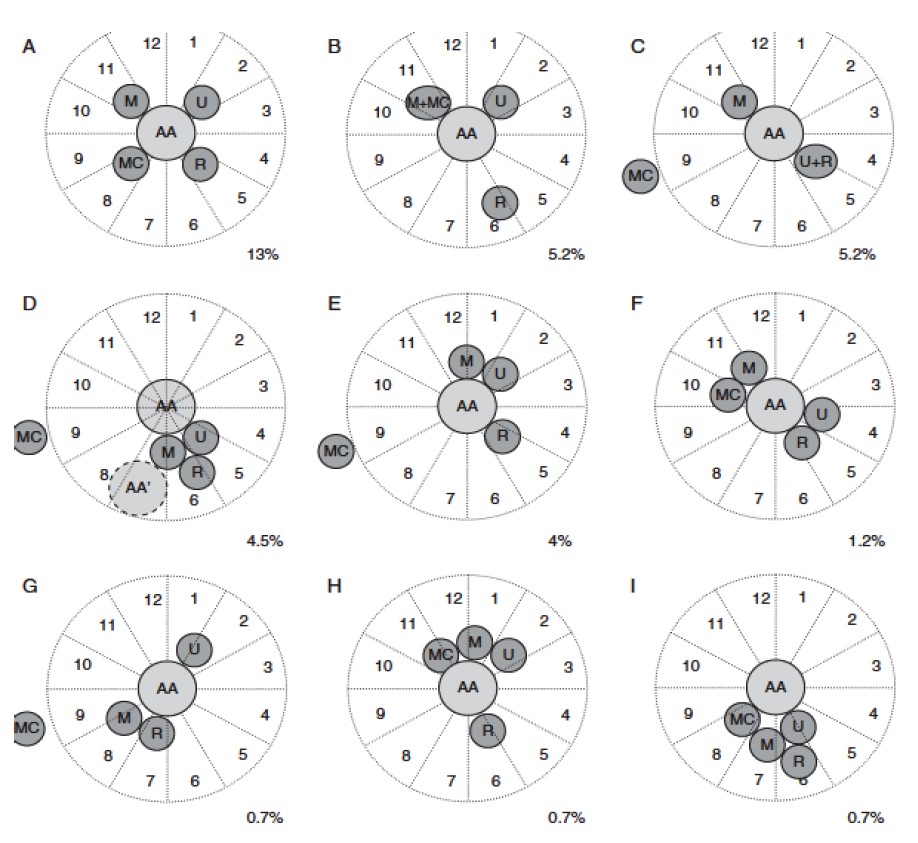
Figure 10. Schematic drawings of the less common arrangements of four nerves of the brachial plexus (M, median nerve; U, ulnar nerve; R, radial nerve; MC, musculocutaneous nerve) around the axillary artery (AA). Frequency of this topographic pattern given in percentage. J.-L. Christophe, et al. Assessment of topographic brachial plexus nerves variations at the axilla using ultrasonography. Br J Anaesth 2009; 103 (4): 606-612. doi: 10.1093/bja/aep207. Reproduced with permission of Oxford University Press on behalf of The British Journal of Anaesthesia Ltd. All rights reserved. This image is not covered by the terms of the Creative Commons licence of this publication. For permissions, please contact journals.permissions@oup.com
SUMMARY
- Anatomical variation of the BP is common and can influence the conduct and outcome of regional anaesthesia.
- Nerve stimulation is considered a blind technique and hence the clinician will not be aware of any underlying anatomical variation.
- Ultrasound, in contrast, enables the visualization of nerves and surrounding structures but its use is greatly dependent on the operator’s knowledge of the relevant anatomy.
- Ultrasound has been shown to improve the success rate of blocks in patients with anatomical variations.21
REFERENCES AND FURTHER READING
- Wozniak J, Kedzia A, Dudek K. Variability of the trunks and divisions of the brachial plexus in human fetuses. Adv Clin Exp Med 2013; 22: 309-18.
- Mian A, Chaudhry I, Huang R, Rizk E, Tubbs RS, Loukas M. Brachial plexus anesthesia: a review of the relevant anatomy, complications, and anatomical variations. Clin Anat 2014; 27: 210-21.
- Neal JM, Gerancher JC, Hebl JR et al. Upper extremity regional anesthesia: essentials of our current understanding. Reg Anesth Pain Med 2009; 34: 134-70.
- Williams PL, Bannister LH, Berry MM, Collins P, Dyson M, Dussek JE, Fergusson MW. Gray’s Anatomy. 38th edn. Toronto: Lippincott Williams and Wilkins, 2006.
- Cornish PB, Leaper C. The sheath of the brachial plexus: fact or fiction? Anesthesiology 2006; 105: 563-65.
- Winnie A, Radonjic R, Akkineni SR, Durrani Z. Factors influencing distribution of local anaesthetic injected into the brachial plexus sheath. Anesthesia and Analgesia 1979; 58: 225-34.
- Thompson GE, Rorie DK. Functional anatomy of the brachial plexus sheaths. Anesthesiology 1983; 59: 117-22.
- Franco CD, Rahman A, Voronov G, Kerns JM, Beck RJ, Buckenmaier CC. Gross anatomy of the brachial plexus sheath in human cadavers. Reg Anesth Pain Med 2008; 33: 64-9.
- Spence BC, Beach ML, Gallagher JD, Sites BD. Ultrasound-guided intrascalene blocks: understanding where to inject the local anaesthetic. Anaesthesia 2011; 66: 509-14.
- Sivashanmugam T, Ray S, Ravishankar M, Jaya V, Selvam E, Karmakar MK. Randomized comparison of extrafascial versus subfascial injection of local anaesthetic during ultrasound-guided supraclavicular brachial plexus block. Reg Anesth Pain Med 2015; 40: 337-43.
- Padur AA, Kumar N, Shanthakumar SR, Shetty SD, Prabhu GS, Patil J. Unusual and unique variant branches of lateral cord of brachial plexus and its clinical implications – a cadaveric study. J Clin Diag Res 2016; 10: AC01-04.
- Kerr AT. The brachial plexus of nerves in man, the variations in its formation and branches. Am J Anat 1918; 23: 285-395.
- Guday E, Bekele A, Muche A. Anatomical study of prefixed versus postfixed brachial plexuses in adult human cadaver. ANZ J Surg 2016 Apr 12; doi: 10.1111/ans.13534 [ePub ahead of print].
- Pellerin M, Kimball Z, Tubbs RS et al. The prefixed and postfixed brachial plexus: a review with surgical implications. Surg Radiol Anat 2010; 32: 251-60.
- Orebaugh SL, Williams BA. Brachial plexus anatomy: normal and variant. ScientificWorldJournal 2009; 9: 300-12.
- Chin KJ, Niazi A, Chan V. Anomalous brachial plexus anatomy in the supraclavicular region detected by ultrasound. Anesth Analg 2008; 107: 729-31.
- Fazan VPS, Amadeu ADS, Caleffi AL, Filho OAR. Brachial plexus variations in its formation and main branches. Acta Cir Bras 2003; 18: 14-8.
- Aggarwal A, Puri N, Aggarwal AK, Harjeet K, Sahni D. Anatomical variation in formation of brachial plexus and its branching. Surg Radiol Anat 2010; 32: 891-4.
- Christophe JL, Berthier F, Boillot A et al. Assessment of topographic brachial plexus nerves variations at the axilla using ultrasonography. Br J Anaesth 2009; 103: 606-12.
- Remerand F, Laulan J, Couvret C et al. Is the musculocutaneous nerve really in the coracobrachialis muscle when performing an axillary block? An ultrasound study. Anesth Analg 2010; 110: 1729-34.
- Klaastad O, Sauter A, Dodgson M. Brachial plexus block with or without ultrasound guidance. Curr Opin Anaesthesiol 2009; 22: 655-60.



