Basic Sciences
QUESTIONS
- Who should be considered for CPET testing?
- What ventilatory variables are measured during a standard CPET test?
- What is the anaerobic threshold?
INTRODUCTION
Cardiopulmonary exercise testing (CPET) is a functional assessment of cardiopulmonary reserve. It has been used in the assessment of elite athletes and for the diagnosis of dyspnoea for which it is now recognised as the gold standard. CPET is becoming routine in the preoperative assessment of patients undergoing major surgical procedures. The results of CPET can help to assess an individual’s risk of perioperative morbidity and mortality and plan their postoperative care including critical care bed allocation.
This tutorial will look at the background to CPET, its physiology, practicalities of performing the test and evidence supporting its use in pre-operative risk stratification. It will not cover direct interpretation of raw CPET data.
OVERVIEW OF CPET
CPET can be used to evaluate both cardiac and respiratory function. CPET systems use the analysis of gas exchange at rest, during exercise and recovery in combination with physiological variables such as heart rate, blood pressure and ECG monitoring, to provide a comprehensive assessment of exercise tolerance1. CPET combines assessment of ventricular, respiratory and cellular function to evaluate cardiovascular and respiratory pathophysiology.
CPET is a valuable tool in the assessment of exertional dyspnoea, myocardial ischaemia and cardiac failure and the effectiveness of their treatment. It can also be used to assess respiratory function by means of exercise spirometry, to assess restrictive and obstructive lung disease and detect exercise-induced asthma.
A patient’s ability to respond to the increased physiological demands of surgery is heavily reliant on their cardiac and pulmonary function1. Cardiac failure is a common denominator in many postoperative deaths. Patients are more likely to die when oxygen delivery is insufficient to meet the body’s oxygen requirements2. Pre-operative CPET aims to quantify cardiorespiratory dysfunction.
PHYSIOLOGY
The ability to perform exercise is directly related to the cardiopulmonary system’s ability to supply oxygen and remove carbon dioxide. These processes require adequate pulmonary ventilation and gas exchange, gas and substrate transport in the blood, and uptake and utilisation at a cellular level. The advantage of CPET is that by taxing these mechanisms, abnormalities not apparent at rest are frequently revealed1.
CPET measures three ventilatory variables:
- Oxygen consumption
- Carbon dioxide excretion
- Minute ventilation.
When these values are combined with power output, heart rate and elapsed time, a number of other variables can be derived. Different patterns of test results are characteristic of specific disease states. Diagnosis and prognosis depend upon the comparison of measured values with tables of predicted values for age, sex, peak measures of oxygen consumption (VO2), power and heart rate, as well as patterns of the derived variables.
VO2 max and VO2 peak
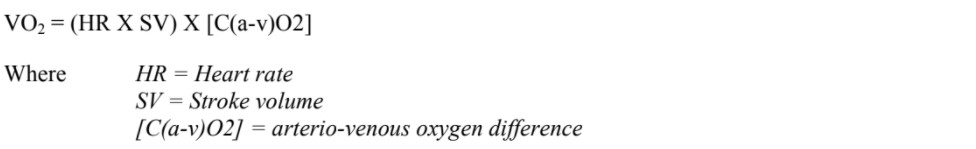
VO2 max is the maximum capacity of an individual’s body to transport and use oxygen during incremental exercise3. It is rarely achieved in the pre-operative assessment clinic. Peak VO2 is the highest oxygen consumption achieved during any particular CPET. Although volitional, the peak VO2 is an important measurement because it is associated with mortality as outlined above. The VO2 measured during CPET is the product of cardiac output and arterio-venous oxygen difference:
The ability to climb more than 5 flights of stairs correlates with a VO2 peak of > 20ml/kg/min, whilst those able to climb less than one flight of stairs correlates with a VO2 peak of < 10ml/kg/min3
Mortality risk is closely associated with peak VO2. A reduction of one metabolic equivalent of task (MET) from predicted peak MET correlates with a 15% increase in mortality, where one MET equals 3.5ml O2 kg-1 min-1. Predicted peak METs are as follows:
- 18.4-(0.16 x age) for men
- 14.7-(0.13 x age) for women.
Age and sex specific interim life tables are available for the UK population through the government actuary department website (http://www.gad.gov.uk) or the website for the UK national office for statistics (http://www.statistics.gov.uk). These are also available for local populations in many other countries worldwide via government websites.
On average, worldwide population mortality has fallen year-on-year, so the most current life tables should be used, either to generate cross-sectional risk, “risk of dying in the next month is 1 in 540”, or longitudinal, “median life expectancy is 15 years”. Comorbidities such as previous myocardial infarction or stroke independently affect mortality risk. These must be taken into account in addition to CPET results when calculating perioperative risks.
It has been suggested that patients with a peak VO2 of less than 14ml/kg/min have a worse overall prognosis than those with a VO2 peak above 14ml/kg/minute in the context of heart failure. However, the relationship between VO2 and survival is continuous, and an absolute cut off point has been challenged.
Anaerobic Threshold
There is an excellent description of the anaerobic threshold by Older et al2, on which the next paragraph is based. Exercise requires immediate breakdown of intracellular adenosine triphosphate (ATP) as a source of high energy phosphate. The source of the ATP is mainly aerobic oxidation of glycogen and fatty acids in mitochondria. When aerobic metabolism is unable to meet the cell’s ATP requirement, anaerobic cytoplasmic metabolism of glucose via pyruvate and lactic acid will provide small amounts of ATP. The point at which aerobic metabolism is no longer adequate and anaerobic supplementation begins is known as the anaerobic threshold (AT). After the AT has been reached, aerobic metabolism does not cease, but anaerobic metabolism supplements aerobic production of ATP as the work rate increases.
Cellular metabolism is reliant on, and limited by, oxygen and substrate availability, which is a direct function of the cardiopulmonary system. CPET is able to identify aerobic metabolism, anaerobic metabolism and the anaerobic threshold because different metabolic pathways have different signatures on gas exchange.
Cellular respiration is coupled to external respiration via the cardiovascular and pulmonary systems as described above. This chain of supply is therefore limited by cardiac function, ventilation adequacy, integrity of the systemic and pulmonary vascular systems and the function of intracellular metabolic pathways. CPET can look at each of these factors and identify heart failure, ventilation/perfusion mismatch, peripheral vascular disease, pulmonary hypertension, and problems with cellular oxygen utilization.
PRACTICALITIES
CPET is carried out as an outpatient procedure. The patient sits on a bicycle ergometer or walks on a treadmill and is connected to a 12 lead ECG, blood pressure cuff and pulse oximeter. Inspired and expired gases are sampled by a metabolic cart via a mouthpiece or facemask, allowing oxygen consumption and carbon dioxide excretion to be measured. The patient then begins pedaling on the bicycle whilst the resistance gradually increases, or walking on the treadmill whilst speed and gradientgradually increase. The test lasts around 13 minutes, although a total of approximately 25 minutes is needed to allow setup of the test including connecting the monitoring.
Discussion of test results
Perhaps the most important part of the consultation is the opportunity to discuss the operation, perioperative care and implications of personalised risk stratification with the patient. This may be the first time that the patient has had the benefits and risks of surgery presented in an easily understandable form. Occasionally this leads to reconsideration of the decision to undergo surgery.
Most appointments take about one hour. In addition to performing the test and the patient discussion, a thorough exploration of the case notes to establish accurate past medical history and context may be time consuming. This is also a good opportunity to complete communication with family members and other clinicians, including surgeons, anaesthetists other relevant specialists, GPs and critical care services.
Blood tests are not routinely performed. Arterial blood is occasionally sampled to better diagnose contributions of heart and lung pathologies to cardiopulmonary dysfunction.
Major complications of CPET include death, myocardial infarction, cardiac arrest and orthopaedic injury. Fortunately major complications are rare (perhaps 1 in 50 000 tests)1, but tests do need to be carried out under appropriate medical supervision, in adequately prepared clinical surroundings.
CPET AND PREOPERATIVE PREPARATION
A report by the Improving Surgical Outcomes Group recognised that tests currently used for the pre-operative evaluation of patients are expensive and poor at predicting actual risk6. Many clinicians are able to quote average mortality and morbidity figures for individual procedures, but it is important that these risks are individualised to patients to make assessment of risk more accurate.
The results of CPET are not only useful for assessing risk but can also guide peri-operative care. Patients can be more appropriately triaged to peri-operative interventions, avoiding unnecessary use of critical care resources whilst increasing critical care surveillance where appropriate. Pre-operative interventions include outpatient exercise, nutritional support and drug therapy. It is likely that risk assessments that include CPET results can guide the use of neoadjuvant chemotherapy and radiotherapy and optimize the timing of surgery. Demand for level 2 and 3 critical care facilities can be anticipated weeks in advance of admission, allowing hospitals to plan patient flow and the allocation of personnel Monday through Sunday6.
Who should be considered for CPET?
Major surgery is associated with high postoperative VO2 and cardiorespiratory demands. Patients with reduced cardiorespiratory reserve may be unable to meet this increased demand.
In order to accurately assess risk both cardiorespiratory reserve and the “oxygen demand” stress of the procedure need to be taken into account. As such patients presenting for major vascular, intra- abdominal, urological or orthopaedic procedures may benefit from CPET, as may patients known to have cardiovascular or respiratory co-morbidities6
SUMMARY
CPET is a non-invasive, functional assessment of cardio-respiratory performance. It has clinical applications in diagnosis, assessment of adequacy of treatment and pre-operative risk stratification of patients. CPET allows the calculation of a number of diagnostic and prognostic variables, and can identify pathophysiology not apparent at rest. CPET identifies patients who are less able to meet the increased oxygen delivery demands of major surgery. This can inform peri-operative planning including the use of pre-operative optimization, invasive monitoring and allocation of post-operative critical care resources.
ANSWERS TO QUESTIONS
- Who should be considered for CPET testing? Patients presenting for major vascular, intra-abdominal, urological or orthopaedic procedures may benefit from CPET, as may patients known to have cardiovascular or respiratory co-morbidities
- What variables are measured during a standard CPET test? Three ventilatory variables are measured: oxygen consumption, carbon dioxide excretion and minute ventilation
- What is the anaerobic threshold? Anaerobic threshold is the point at which aerobic metabolism is no longer adequate and anaerobic supplementation begins.
WEBLINKS
REFERENCES and FURTHER READING
- Balady G J, et al. Clinician’s guide to cardiopulmonary exercise testing in adults. Circulation. 2010; 122:191-225.
- Older P, Hall A. Wasserman, K (ed): Gas Exchange in Heart Disease. Armonk, NY: Futura publishing Company, Inc. 1996
- Myers et al. Cardiopulmonary exercise testing and prognosis in severe heart failure: 14mL/kg/min revisited. Am Heart Journal. 139(1):78-84, 2000
- Portch D, McCormick B. Pulmonary Function Tests and Assessment for LungResection. Update in Anaesthesia. http://update.anaesthesiologists.org
- Modernising care for patients undergoing major surgery. Improving patient outcomes and increasing clinical efficiency. A report by the Improving Surgical Outcomes Group
- http://www.v02max.co.uk/pre-op-assessment.html



