Regional Anaesthesia
Tutorial 55
Questions
- Why does a LA solution containing Epinephrine cause pain on injection and what can be done to render it less painful?
- What is the maximum time of upper and lower limb ischaemia?
- How can you avoid a systemic LA bolus using IVRA?
- What is your choice of drug for IVRA and why?
- What are the landmarks for the radial, median and ulnar nerves at the wrist and what sensory areas do they supply?
CARPAL TUNNEL RELEASE BLOCK
INTRODUCTION
- Carpal tunnel syndrome is a common problem and the operation to decompress the tunnel is usually performed under local anaesthesia.
- These operations can be done endoscopically but the majority are still performed with an open surgical technique.
- This block is usually carried out by the surgeon and many patients find the local anaesthetic infiltration particularly painful.
- I believe the following technique considerably reduces the pain of this procedure.
ANATOMY
- The carpal tunnel is formed by the arc of carpal bones posteriorly and the flexor retinaculum anteriorly. Through this tunnel travel the flexor tendons and the median nerve.
- The median nerve is surprisingly large (about the size of a pencil) and lies between the tendons of palmaris longus and flexor carpi radialis. It is 1 – 1.5 cm deep to the skin.
- Imagine the carpal tunnel as an archers bow. The carpal bones are the bow and the flexor retinaculum is the bowstring. The retinaculum is cut to allow the carpal bones to ‘spring” open, thereby releasing the pressure on the tunnel contents. the pressure on the tunnel contents.
EQUIPMENT
- Dental syringe and 27 G dental needle + 4 dental cartridges of prilocaine and felypressin.
- OR a 10 ml plastic syringe + 25 G (38mm) needle.
- 22 G (50 mm) short bevel needle.
- Prep solution.
TECHNIQUE
- If the patient is unduly anxious you may wish to administer intravenous midazolam and fentanyl. A bilateral infiltration can be quite unpleasant for the patient.
- Apply a pulse oximeter probe.
- Lay the forearm in a supine position and identify the landmarks. In particular note the median nerve location.
- The surgical incision will extend from 1 cm proximal to the wrist crease, along the “lifeline” for 2 – 3 cm distal to the wrist crease. Note the position of the subcutaneous veins and try to avoid perforating them.
- Apply the prep solution.
- I prefer to use a dental syringe and a 27 G long needle. The prilocaine / felypressin solution is less painful on injection.
- Insert the needle at the level of the distal wrist crease at the midline of the wrist. Slide it subcutaneously towards the elbow for 3 cm injecting as you go.
- It is sufficient to infiltrate the midline only but I usually fan the needle on either side of the midline. Inject a total of 2 – 3 ml.
- Without removing the needle from the skin, redirect it 180° and gradually advance along the line of the proposed incision for 3 – 4 cm. The subcutaneous palmar tissues are densely adherent. It is tough and very painful when injected. Take your time and advance the needle millimetre by millimetre injecting slowly as you go. Again it is prudent to redirect the needle twice on either side of the initial injection line. Use a total of 3 – 4 ml of LA.
- This is usually sufficient. The surgeon can inject more if necessary.
- I also inject LA deep to the flexor retinaculum. Use a 22 G short bevel needle and enter the skin just distal to the distal wrist crease and medial to the median nerve. The needle is vertical and at 0.5 – 1 cm depth you will feel the resistance of the flexor retinaculum. Use a loss of resistance technique to penetrate the ligament and just emerge on the far side.
- If the patient experiences a sharp pain, don’t inject. Make a second attempt more medially. Inject 3 ml of local anaesthesia into the tunnel.
- Place your thumb over the tunnel and press forcibly whilst flexing and extending the wrist half a dozen times. This forces the anaesthetic proximally and distally.
- An arm tourniquet is not required.
- Surgery can be commenced in 10 minutes.
DRUGS
- The commonly used local anaesthetic is lidocaine 1% with epinephrine. This works well but the epinephrine makes the LA quite acid and therefore painful.
- The solution can be rendered less painful by adding sodium bicarbonate ( 1 ml of 8.4% solution per 10 ml of lidocaine) and by warming the injectate to body temperature.
- Surgeons will tell you they prefer a concentrated epinephrine solution (eg 1:80,000) as it results in better vasoconstriction. I don’t agree with this as a better way to stem the blood flow is to apply the self retaining retractor.
- Prilocaine 1% + felypressin ( available in 2.2 ml cartridges) may be a preferred choice as it is less painful on injection.
- Bupivacaine 0.25% or Ropivacaine 0.3% are acceptable but the prolonged post operative analgesia is often accompanied by a patient complaint of prolonged median nerve block. Some patients find this paraesthesia unpleasant.
CONCLUSION
- Try to avoid injecting into the median nerve. Keep well to the medial side of it and don’t inject if the patient complains of pain.
- Bilateral carpal tunnel releases in particularly anxious patients should be done under general anaesthesia.
INTRAVENOUS REGIONAL ANAESTHESIA (IVRA)
(ALSO KNOWN AS BIERS BLOCK)
INTRODUCTION
- In the hands of the novice anaesthetist, this may well be the easiest block in the book.
- All that is required is the competence to insert an intravenous cannula and an ability to follow instructions to the letter.
- As with all regional blocks, it is mandatory to possess the necessary knowledge, skills and equipment to undertake emergency resuscitation.
- Intravenous Regional Anaesthesia (IVRA) provides good anaesthesia for surgical procedures below the elbow or knee.
- The block has its limitations. It is only suitable for surgery of less than 60 – 90 minutes duration. After this time the risks of prolonged tissue ischaemia and tourniquet discomfort become major considerations.
- Tourniquet pain can be “managed” by a subcutaneous ring block above the tourniquet and the judicious administration of intravenous midazolam / fentanyl.
- Tourniquet time however is non negotiable. The maximum time of upper limb ischaemia is 90 minutes (120 minutes for leg).
- Because of these limitations I seldom use IVRA in my everyday anaesthetic practice.
- I prefer a brachial plexus block which allows prolonged surgical anaesthesia and analgesia in the post operative period. A plexus block also covers the tourniquet discomfort.
- There is no getting away from the fact that IVRA is a simple, reliable and safe technique if performed properly. This makes it an excellent choice for the occasional anaesthetist.
INDICATIONS
- Minor surgery below the elbow in the upper limb and below the knee in the lower limb.
- Manipulation of fractures (eg Colles).
- Best reserved for superficial procedures (eg excision of skin lesions).
EQUIPMENT
- Double cuff tourniquet ideally (a single cuff tourniquet is satisfactory if a double cuff is unavailable). This must be checked for leaks and have an accurate manometer.
- Esmarch bandage. This is an elastic bandage which is wrapped around the limb to exsanguinate below the tourniquet.
- A 50 ml plastic syringe.
- 20 G intravenous cannula.
- Pulse oximeter.
- Resuscitation equipment.
TECHNIQUE
- I will outline the technique for an upper limb IVRA procedure. The lower limb is a virtually identical technique apart from some differences which I will discuss at the end of this section.
- The principle of the double cuff tourniquet system is to inflate the upper cuff and then inject the LA. After a few minutes the skin under the lower cuff will be insensitive. The lower cuff is inflated and the upper deflated (MAKE SURE YOU DON’T DEFLATE THE TWO CUFFS SIMULTANEOUSLY).
- Check the tourniquet and sphygmometer for leaks.
- Attach SpO2 (and ECG + BP if indicated).
- Insert a 20 G plastic cannula into the dorsi of each hand (the second cannula is for safety and iv sedation / analgesia).
- Check the systolic blood pressure.
- Apply the double cuff tourniquet to the padded upper arm.
- Use the Esmarch bandage to exsanguinate the arm below the tourniquet. In the case of an open wound or fracture it is acceptable to elevate the arm for 1 minute whilst compressing the brachial artery. [Fig 14 a, b, c]
- Inflate the upper cuff to 100 mm Hg above systolic.
- Check to ensure the radial pulse has vanished.
- Infuse prilocaine 0.5% (or lidocaine 0.5%) over 60 seconds. A typical volume for an 80 kg man would be 50 ml.
- This LA should not contain epinephrine. The maximum safe dose of both lidocaine and prilocaine is 3 mg / kg.
- Wait 5 – 10 minutes for the block to take effect and then inflate the distal cuff and deflate the proximal cuff. This must be done carefully. You cannot allow both cuffs to deflate accidentally as a large bolus of LA would enter the circulation.
- The arm will be blotchy and cyanosed. Surgery can begin.
- Tourniquet discomfort should be minimal if correct double cuff technique is followed. If you are using a single cuff, tourniquet pain can be alleviated by judicious doses of intravenous midazolam / fentanyl. A subcutaneous ring block of the arm above the tourniquet also helps.
- Do not let the tourniquet down for at least 20 minutes. Between 20 and 40 minutes the tourniquet should be deflated for 10 seconds and then reinflated for 10 seconds before finally deflating. This lessens the likelihood of a bolus of LA hitting the circulation.
- Occasionally the patient complains of tinnitus, flushes and dizziness when the tourniquet is released.
- Should a major complication occur (eg convulsions, cardiac arrest) institute immediate acute life support. Intubation, IPPV and anticonvulsants may be needed.
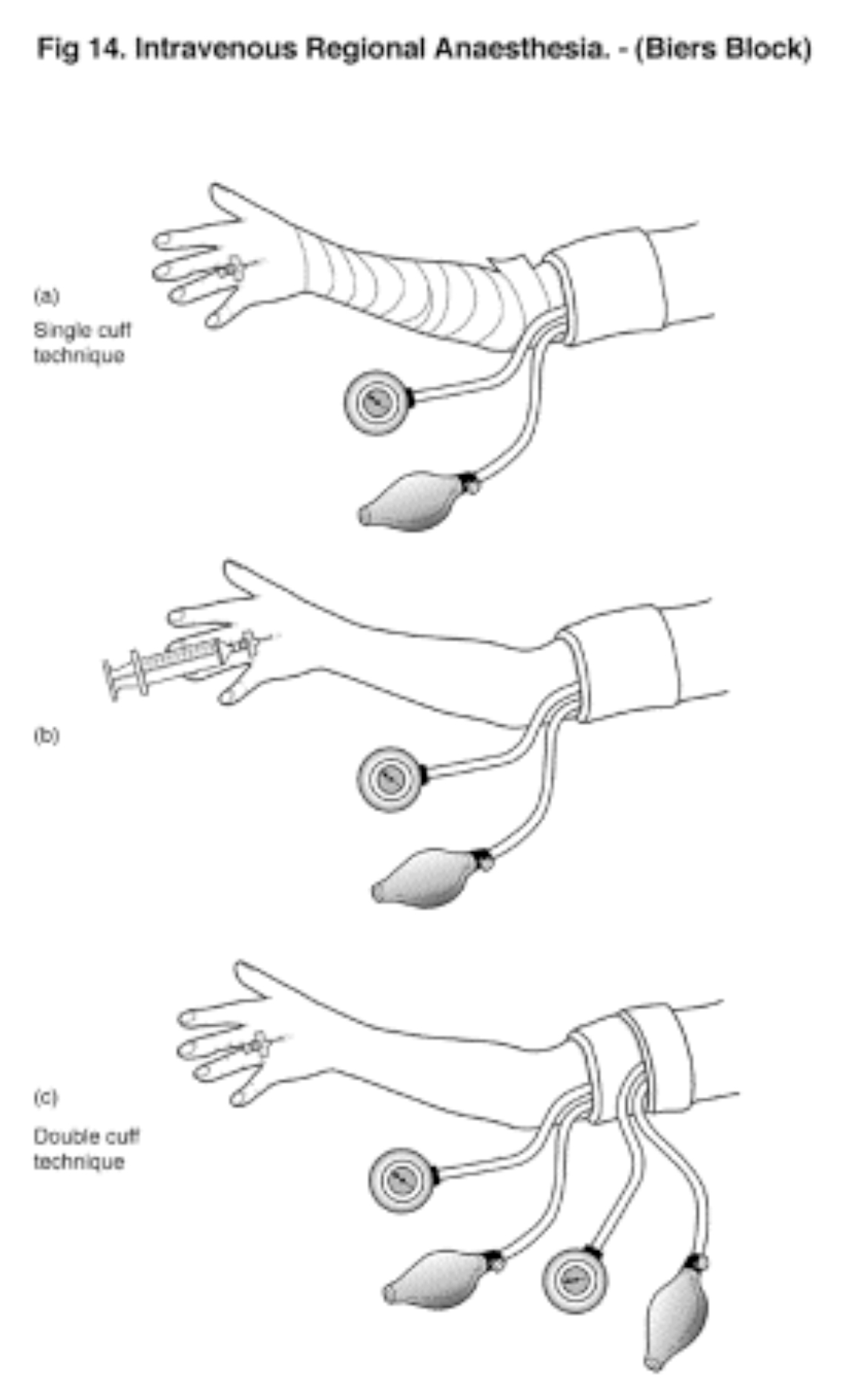
Figure 14 a,b,c (Click to enlarge)
DRUGS
- DO NOT USE BUPIVACAINE. It was a popular choice for IVRA at one time but there is an unacceptable risk of cardiac toxicity should a bolus of bupivacaine enter the circulation.
- At this stage neither levobupivacaine or ropivacaine are recommended for IVRA.
- The drug of choice is Prilocaine 0.5% but Lidocaine 0.5% is a satisfactory alternative.
- In adults, use 40 ml in a small arm, 50 ml in a medium sized arm and 60 ml in a large arm.
- Use Prilocaine 0.5% 3 mg / kg without epinephrine.
- In the lower limb larger volumes are necessary. It may be permissible to use up to 400 mg of prilocaine in an 80 kg man (ie 80 ml of a 0.5% solution). The maximum dose of lidocaine would be 250 mg (ie 50 ml 0f 0.5%).
- Clonidine 75 mcg can be added to the solution.
- Some anaesthetists add fentanyl and muscle relaxant to the LA solution. I don’t believe there is a significant advantage in this practice.
IMPORTANT POINTS
- IVRA is extremely safe providing the recommended procedure is adhered to.
- The main complication is inadvertent deflation of the tourniquet in the first 10 – 20 minutes. Even this occurrence is unlikely to be too serious in a young fit individual.
- IVRA is an easy learnt, simple regional block. It is a good reliable, safe technique in the hands of the occasional anaesthetist.
- IVRA is really only suitable for surgical procedures of 30 – 40 minutes duration.
- IVRA can be satisfactorily performed with a single cuff attached to a sphygmomanometer. It is not as elegant but is quite safe.
WRIST BLOCKS
INTRODUCTION
- Three nerves supply sensation to the hand – the median, the ulnar and the radial
- It is a simple matter to block these nerves at the wrist as the landmarks are obvious and the nerves are superficial.
- Blockade provides good conditions for hand surgery and excellent post operative analgesia.
- Patchy brachial plexus blocks can be supplemented by blocking the appropriate nerves at the wrist.
- Unfortunately hand surgeons demand a bloodless field which necessitates an upper arm tourniquet. It is often easier to block the whole arm to cover both the surgery and the tourniquet discomfort.
- It is important to have a good appreciation of the anatomy in order to achieve consistent success with wrist blocks.
ANATOMY
The median, ulnar and radial nerves supply the hand. [Fig 11]
Median nerve:
- The key landmark is the palmaris longus tendon which is located at the centre of the palmar aspect of the wrist. Make a clenched fist and it is immediately obvious (10% of people do not have this tendon).
- Place your index finger tip on the palmaris longus tendon. One centimetre on the radial side of palmaris longus lies the flexor carpi radialis tendon.
- The median nerve lies between these two tendons at a depth of approximately 1 cm.
- It supplies the skin of the thumb, index, middle and half the ring finger on the palm and the distal parts of the same three digits on the dorsum.
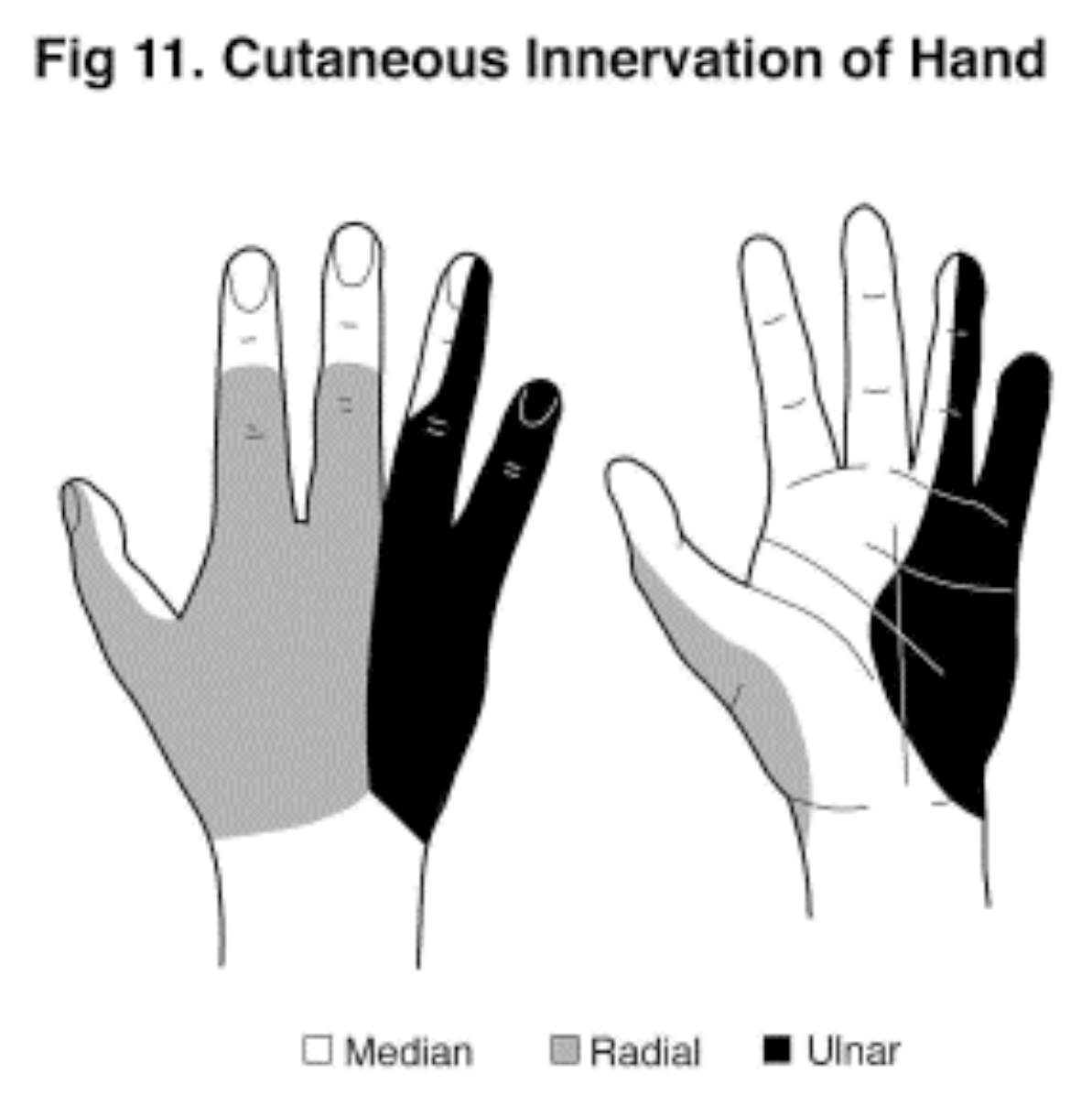
Figure 11 (Click to enlarge)
Ulnar nerve:
- Again make a clenched fist and locate the flexor carpi ulnaris tendon.
- The ulnar arterial pulse can be palpated just radial to this tendon.
- The ulnar nerve divides into dorsal sensory branches at a variable distance above the wrist. This is a “spray” of subcutaneous nerves.
- It supplies an area of skin covering the 4th and 5th digit on both the palm and dorsum as well as sending motor fibres to the intrinsic muscles.
Radial nerve:
- This nerve is entirely sensory and cutaneous at wrist level.
- It supplies an area of skin on the dorsum of the hand.
- I suggest you take an anatomical atlas and familiarise yourself with the landmarks.
- Remember:
- Median – radial side of palmaris longus
- Ulnar– ulnar side of ulnar artery.
- Radial– radial side of radial artery (subcutaneous)
INDICATIONS
- Hand surgery – may block one, two or three.
- Supplementation of patchy brachial plexus block.
EQUIPMENT
- Insulin syringe with fine needle for subcutaneous LA infiltration.
- 10 ml plastic syringe
- 25 G needles – 25 mm (short) and 38 mm (long).
- Sterile gloves and prep solution.
- Monitoring and iv cannula – I don’t bother but you may feel more comfortable with a pulse oximeter and an iv cannula in the other hand.
TECHNIQUE
MEDIAN NERVE:
- This nerve lies between palmaris longus and flexor carpi radialis, approximately 1 cm beneath the skin.
- The entry point is 2 cm proximal to the distal wrist crease and between the tendons.
- Inject a subcutaneous bleb of LA with the insulin syringe and then insert a 25 G (25mm) needle vertically.
- At a depth of 1 cm you should elicit a paraesthesia (you may have to redirect beneath palmaris longus to achieve this).
- You may be aware of the slight loss of resistance as the needle penetrates the flexor retinaculum. If paraesthesia hasn’t been obtained, simply inject the LA below this structure.
- Withdraw the needle 1 – 2 mm to avoid intraneural injection and deposit 4 ml of LA.
- Withdraw the needle to the skin and redirect the tip subcutaneously towards the palm of the hand. Inject 1 ml of LA to block the palmar cutaneous branch.
ULNAR NERVE:
- This nerve lies between the ulnar artery and flexor carpi ulnaris, approximately 1 –1.5 cm beneath the skin.
- The entry point is 2.5 cm proximal to the distal wrist crease between the artery and tendon.
- Using the insulin syringe, inject a bleb of subcutaneous LA and insert the long 25 G needle vertically.
- At a depth of 1 – 1.5 cm a paraesthesia is elicited. Withdraw the needle 1 – 2 mm and deposit 4 ml of LA.
- The ulnar nerve breaks into a spray of subcutaneous dorsal sensory nerves 5 – 10 cm above the wrist. To block these withdraw the needle to the skin and redirect it towards the ulnar side of the wrist. 5 – 10 ml of LA are infiltrated subcutaneously in a ring block fashion right around the wrist to the styloid process.
RADIAL NERVE:
- This nerve is entirely subcutaneous and sensory at wrist level. All that is required to block these is a subcutaneous infiltration of LA in ring block fashion from the radial artery (at a point 2.5 cm proximal to the distal wrist crease) around the radial border of the wrist to just beyond the anatomical snuff box.
- Use a long 25 G needle and inject 7 – 10 ml of LA.
DRUGS
- I generally use bupivacaine 0.25% or ropivacaine 0.4%. Lidocaine 1% is satisfactory for short procedures but invariably a prolonged period of post operative analgesia is preferable.
- Combine the LA with a vasoconstrictor (epinephrine 1:200,000) as this intensifies and adds to the duration of the block. Some authorities frown on this practice because of a perceived potential for end artery ischaemia.
IMPORTANT POINTS
- Wrist blocks are quick and easy to perform but they do involve multiple injections and hence a degree of patient discomfort.
- If a tourniquet is required it may be better to use a brachial plexus block. Stoical patients will tolerate a tourniquet for up to one hour, especially if intravenous midazolam and fentanyl are used.
- NEVER inject LA if the patient complains of severe pain on injection. Withdraw slightly and continue injecting. Intraneural injections can cause prolonged neuritis.
- I rarely block nerves at elbow level. The wrist is easier and I find I can provide suitable upper limb anaesthesia with either a brachial plexus block and / or a wrist block.
- If you block all three nerves you will find the ulnar and radial subcutaneous infiltrations almost meet on the dorsum of the wrist. I personally have no problem with producing a “total wrist ring block” but some anaesthetists counsel against this practice because of the potential for ischaemia.
- Some recommend not deliberately seeking paraesthesia due to the risk of post block neuritis. This is a reasonable concern. Simply inject beneath the flexor retinaculum to block the median and for the ulnar, advance to bone and inject the LA as you withdraw. The subcutaneous infiltrations are unchanged.



