Cardiothoracic Anaesthesia
KEY POINTS
- Deep Hypothermic Circulatory Arrest (DHCS) is a technique used mainly to facilitate complex aortic arch surgery.
- Deep hypothermia reduces cellular metabolism and protects tissues from ischaemia during circulatory arrest, most importantly the central nervous system.
- In addition to the usual complications of cardiac surgery and cardiopulmonary bypass, deep hypothermia induces a significant coagulopathy.
- Even at very low core temperatures, cerebral metabolism is not abolished and therefore the duration of DHCA must be as short as possible to reduce complications.
- Pharmacological neuroprotection and adjuvant perfusion methods are often used to improve the safety of the technique.
INTRODUCTION
Deep Hypothermic Circulatory Arrest (DHCA) is a technique employed to facilitate complex cardiovascular surgery. Complete cardiopulmonary arrest is induced to allow surgery on major blood vessels which cannot be bypassed intraoperatively and therefore upon which surgery would normally cause disruption to distal blood flow and profound haemorrhage in the surgical field. Hypothermia causes a depression of the metabolic rate and cellular metabolism, protecting the central nervous system (CNS) from ischemia. Hypothermia is defined as mild between 32 to 35°C, moderate between 28 and 32°C and deep less than 28°C.
One fifth of total oxygen consumption is by the CNS, 60% to maintain cellular integrity and 40 % for neurotransmission. On average, the cerebral metabolic rate for oxygen (CMRO2) is reduced by 7% for every 1°c decrease in temperature from 37°c and this decrease accelerates under 20°c1. This is combined with the linear reduction in cerebral blood flow (CBF) with hypothermia and results in uncoupling of CBF and CMRO2 at 22°c 2. At 18°c, 60% of patients will have an isoelectric electroencephalogram (EEG), increasing to 99% of patients at 12.5°c. 1 This represents profound suppression of cerebral metabolic activity and confers the neuroprotection of deep hypothermia. The use of hypothermic circulatory arrest is limited by the duration of the circulatory arrest that can safely be tolerated before significant neurological and multisystem side effects occur.
INDICATIONS FOR DHCA
DHCA is most commonly used in elective complex aortic arch surgery where it is impossible to perfuse the brain through cerebral vessels using cardio pulmonary bypass (CPB). DHCA is also commonly employed in repair of Type A dissection in an emergency. Other indications are shown in table 1.
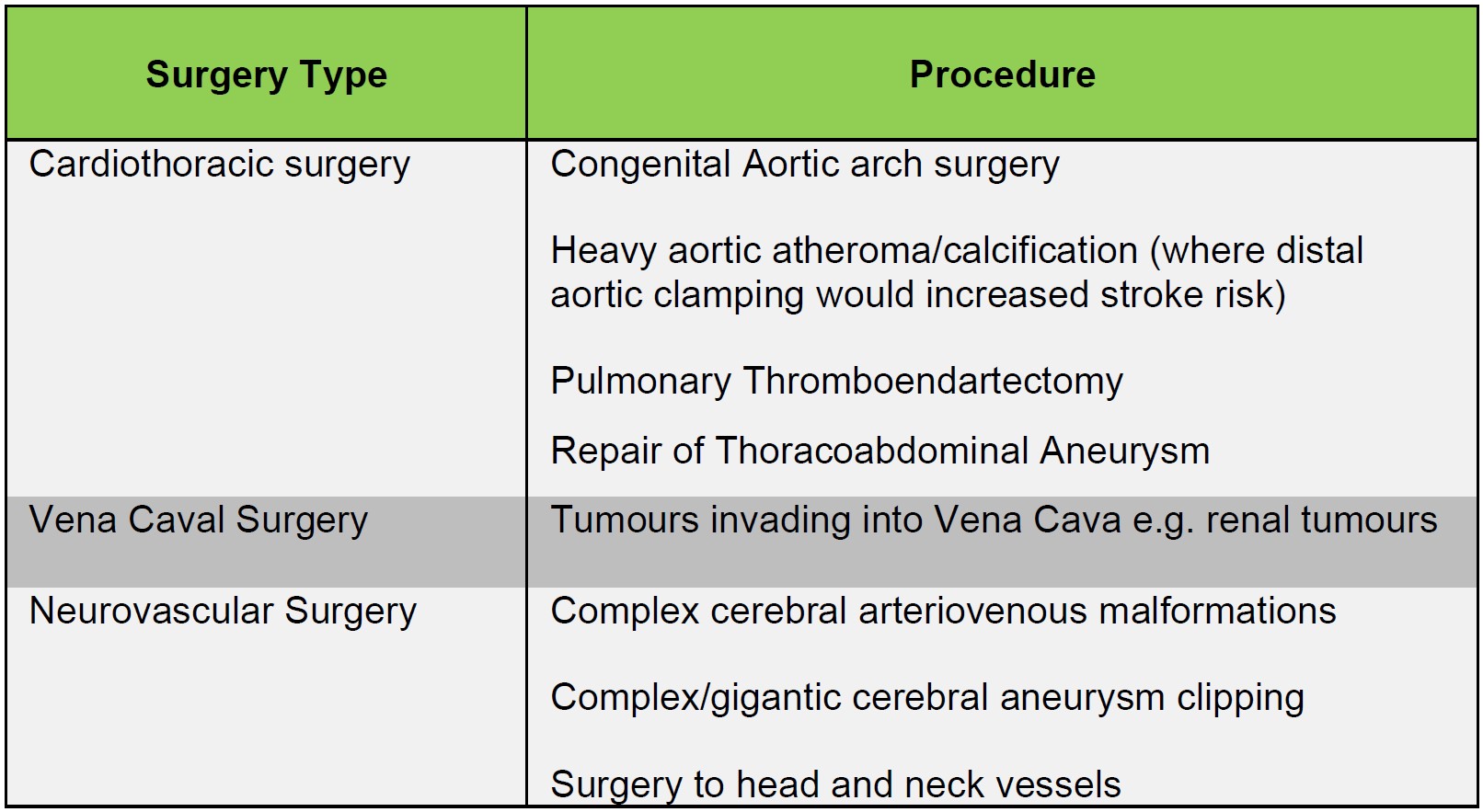
Table 1 showing other indications for Deep Hypothermic Circulatory Arrest
CONDUCT OF DHCA
Pre-operative assessment and pre-medication are conducted as per any open-heart procedure. A baseline neurological exam is useful prior to DHCA to establish a baseline in the event of emerging neurological deficits in the post-operative course. In addition, some centres employ neurocognitive tests to detect more subtle changes post-operatively. Invasive arterial monitoring placement and its interpretation will be decided by the nature of surgery, the location for bypass cannulation and whether any perfusion adjuncts are to be used, and may require bilateral upper limb or a combination of right upper limb and lower limb cannulation. Temperature measurement is of utmost importance in DHCA. Often, two sites are used such as nasopharynx and oesophagus or nasopharynx and urinary bladder temperature. A pulmonary artery flotation catheter and bypass return line temperature are additional sources of information for temperature. The patient is heparinized and CPB commenced as standard but timings and the degree of hypothermia are generally instructed by the surgical procedure.
Cooling and arrest
Once CPB is established at full pump flow rate, cooling will begin to the chosen temperature. The temperature gradient between the venous inflow to the CPB circuit and the arterial outflow is kept at less than 10°c.3 Many centres pack the head in ice or use a head cooling device to prevent passive rewarming. If clinicians choose pharmacological neuroprotective modalities they are administered before the circulatory arrest. Types of pharmacological neuro-protective agents will be further discusses later in the tutorial.
The intravenous anaesthetic agents, if used, can be titrated, once the patient is below 28 degrees and additional paralytics can be re-dosed before the circulatory arrest. Once the desired temperature is reached the patient is partially exsanguinated into the CPB circuit and bypass is terminated. The heparinized blood during DHCA lies in stasis and no further drug can be infused nor can blood be sampled.
Optimal temperature and duration of DHCA
An optimal temperature is still the subject of on going research. With differing study methodologies and wide variations in practice, a consensus on an optimal temperature is difficult to achieve. Most centres will conduct DHCA at a temperature of 18-20°c.
Studies performed on pigs have shown that even at core temperatures of 8°c, CMRO2 remains at 8 to 11% of baseline11.. The conclusion has been made that during DHCA, oxygen consumption still occurs despite an isoelectric EEG. Outcomes from studies suggest a DHCA duration of 40 minutes is probably safe after which the incidence of stroke and neurological deficit begins to markedly rise4,5, therefore, the DHCA duration should be as short as possible.
Glucose and haematocrit management
It is well established that hyperglycaemia is associated with adverse postoperative outcomes in cardiac surgery.2 Hyperglycaemia is common during DHCA. CPB induced inflammatory mediators mediate insulin resistance whilst hypothermia causes decreased insulin release. In addition, corticosteroids are commonly administered for neuroprotection prior to DHCA which exacerbates the problem. Hyperglycaemia leads to intracellular acidosis as lactate is produced from glucose and promotes excitotoxicity. Blood glucose levels should be monitored every 30mins aiming for <10mmol.l-1.
Deep hypothermia leads to increased blood viscosity, increased red cell rigidity, causes impaired microcirculation and potentially ischaemia. In addition, the oxyhaemoglobin dissociation curve is shifted to the left impairing oxygen delivery.
Haemodilution improves microcirculatory flow but at the expense of a decreased oxygen carrying capacity but this is less critical during deep hypothermia due to the profound decrease in oxygen consumption. Whilst there is limited evidence to suggest an optimal target, a haematocrit of 22% or Hb of 7.5g/dL is usually maintained, with a recent study showing no benefit when Hb was maintained at either >8g/dL or >10 g/dL during DHCA6.
Neurological Monitoring during DHCA
This may take two forms:
1. Electrical – Electroencephalogram (EEG) or Somatosensory evoked potentials (SSEPs)
2. Oximetry – Jugular Venous bulb oxygen saturations (SjO2) and near infrared spectroscopy (NIRS)
In some centres, depth of anaesthesia monitoring may be used (e.g. BIS monitoring) however it is unclear how to interpret these values in the context of DHCA. Table 2 shows the advantages and limitations of the different methods.
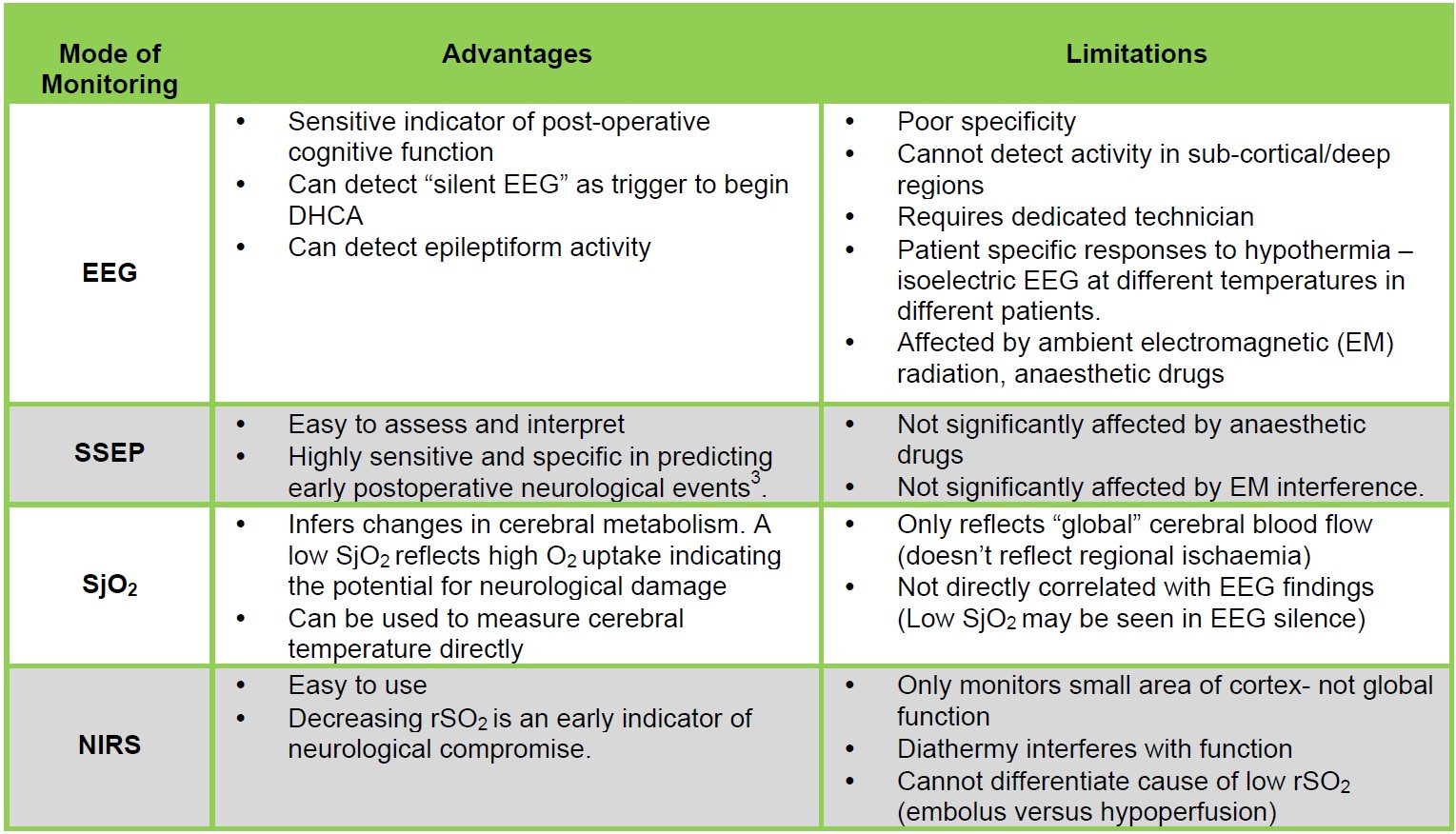
Table 2. Advantages and limitations of various forms of neurological monitoring during DHCA.
ADDITIONAL NEUROPROTECTIVE STRATGIES DURING DHCA
Pharmacological neuroprotection
Pharmacological agents are commonly administered to enhance the neuroprotective effect of deep hypothermia. During DHCA no new drugs can be added to the patient’s blood so drugs must be administered prior to cessation of circulation. A recent worldwide survey of 105 centres indicated differing practices.7 European centres most commonly administer thiopental compared to non-European centres (61.5% vs 17.7%) who prefer propofol (66.1% vs 28.4%). Corticosteroids were routinely used throughout all centres (approximately 70% of European Centres and 95% of non-European centres) and the most common agent was methylprednisolone.
Thiopental and propofol both decrease CMRO2 and decrease CBF. The greatest neuroprotective effects of thiopental are seen at high doses which tend to cause myocardial depression. In addition, this may lead to delayed wakening and extubation. This effect is not seen with propofol but there is little evidence to suggest an improved neurological outcome with either drug in DHCA1. Corticosteroids reduce the systemic inflammatory response (SIRS) generated by the CPB and reduce levels of inflammatory cytokines but do however make maintenance of normoglycaemia more difficult and may lead to an increased risk of sepsis. Again, conflicting evidence does not indicate a clear benefit.
In some units, general anaesthesia is maintained using volatile agents added through the circuit. Volatiles confer global cerebral protection, depress metabolic demand and reduce excitotoxicity by inhibiting glutamate release. Volatile agents increase tolerance to ischaemia in animal models through pre-conditioning but there is insufficient data yet to infer how this translates into neuroprotection during DHCA. Various other agents are used less frequently for example magnesium, mannitol and lidocaine. In addition, a multitude of other agents have been investigated, however much of this work is in animal models or CPB-only cardiac surgery meaning that currently no drug has any established efficacy in improving neurological outcome in DHCA.
Acid base management
Decreases in blood temperature results in decreased ionization of water and an increase in the solubility of gases in blood as described in Table 3. This leads to the physiological alkalosis of hypothermia. However, blood gas analysers warm blood to 37°c for analysis irrespective of the patient’s actual temperature, therefore the ABG results will show normal pH and pCO2 values. To correct for this, the temperature is manually input and the machine mathematically calculates the values for that temperature using the Rosethal correction (Change in pH = 0.015 pH units per degree C change in temperature). For example, arterial blood glass (ABG) analysis performed on a patient at 20°c would show a pH of 7.65 a pCO2 of 2.4kPa (18mmHg) but it must be remembered that the total CO2 content of blood remains the same.
There are two methods of interpreting blood gas analysis in the hypothermic patient:
- The pH-Stat method. The ABG is corrected for the patient’s temperature and the results are interpreted against the “normal values” for 37 °c which are pH of 7.4 and pCO2 of 5.3kPa (40mmHg). As in the above example a patient cooled to 20°c would appear alkalotic and hypocapnic. The perfusionist acts to correct these values to “normal”, i.e. the aim is to maintain a pH of 7.4 and pCO2 of 5.3kPa irrespective of the patient’s actual temperature. This is achieved by adding carbon dioxide to the CPB circuit. The patient’s blood now becomes acidotic and hypercapnic and there is an increase in the total CO2 content.
- The Alpha-Stat method. The ABG result is NOT temperature corrected. The results at 37°C are interpreted against the “normal values” for 37°c and the aim is to maintain those parameters. This allows the physiological hypothermic alkaline drift to occur allowing the intracellular pH to be maintained.
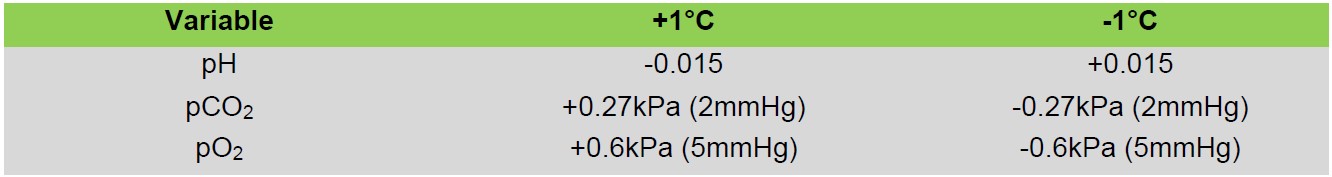
Table 3. Outlining the blood gas changes seen with each 1°C deviation from 37°C
Arterial pCO2 is the major regulatory factor on cerebral blood flow. The pH-Stat method increases arterial pCO2 which leads to an increased cerebral blood flow and a loss of autoregulation which allows faster and more homogenous cooling and improved oxygen delivery, however it does permit an increased embolic load and may contribute to cerebral oedema during warming. Porcine modelling shows improved neurological outcome when pH-Stat is used during cooling, even despite a controlled microembolic load8. In addition, in neonates and infants, pH-Stat appears to yield improved mortality2. Using Alpha-Stat, cerebral autoregulation is preserved reducing the risk of cerebral oedema and emboli, but may lead to uneven distribution of blood flow in those with underlying cerebral vasculopathy. Cerebral enzymatic activity is better preserved however. Many studies suggest that Alpha-stat provides more optimal neurological outcomes in adults, whilst others studies also found no difference.
Conflicting evidence make it difficult to favour one method over the other and in addition many studies comparing the two strategies have been focused on CPB only cases and as such can only be extrapolated to the unique physiology of DHCA. Svyatets et al9 recommend using a combined strategy in which pH-Stat is used during cooling and then switching to Alpha-Stat at arrest and rewarming.
REWARMING
After completion of the portion of surgery requiring DHCA, CPB is reinstituted. Initially deep hypothermia is maintained for around 10 minutes in order to reperfuse the CNS with cold blood to reduce ischaemic reperfusion injury. Again, a temperature arterio-venous gradient of <10°c is maintained. Warming must be slow and usually limited to <0.5°c per minute 2. The time to achieve rewarming therefore may be up to 90 minutes. In addition, the core temperature should not exceed 36.5°c as hyperthermia will exacerbate any neurological damage. During rewarming, hypothermia coagulopathy must be managed aggressively. The intravenous anaesthetic agents will need to be titrated up during rewarming.
ADJUVANT PERFUSION STRATEGIES
There are two adjuvant perfusion techniques which may modify DHCA. These combine therapeutic hypothermia with intra-operative cerebral perfusion to maintain blood flow to the brain during surgery. This is analogous to cold cardioplegia during CPB and has been termed “cerebroplegia”. The techniques differ between centres and among specialists. An in-depth explanation is beyond the scope of this tutorial but there are two broad approaches: Images 1 & 2 offer a simplistic illustration of the two techniques.
- Selective antegrade cerebral perfusion (SACP; Figure 1): The cerebral vessels are selectively perfused either in a hemispheric or bi-hemispheric fashion with intra-operative surgical cannulation, separate from CPB and relies on an intact circle of Willis to perfuse the whole brain. A flow of 10-20mls.kg-1 aiming for mean pressures of 50-70mmHg is used in many centres as this is deemed to be physiological10. The advantages of this technique is that it allows a lesser degree of hypothermia (23-25°c) which decreases hypothermic complications and the length of cooling/rewarming periods and therefore total CPB time. In addition, it maintains a constant supply of oxygenated blood to the brain during the surgery. Additionally, the SACP can be configured to deliver cold (10-12°c) blood to the brain while allowing a higher body core temperature (25-29°c). This technique does however still require DHCA to the lower body whilst surgery on the aorta is completed.
- Retrograde cerebral perfusion (RCP; Figure 2): The brain is perfused in a retrograde fashion with cold oxygenated blood through the superior vena cava which is snared below the azygous vein. Blood drains back through the arch vessels. It is based on the premise that the cerebral venous system is valveless, however the presence of valves has been shown in humans11. The perfusion pressure typically used is 25mmHg. The advantage of RCP is its ability to extend the safe duration of DHCA up to 60 minutes11, however many studies dispute the ability of RCP to achieve effective cerebral perfusion and it may be that RCP helps to maintain a low intracranial temperature in DHCA. It is also less likely to cause distal emboli than SACP.
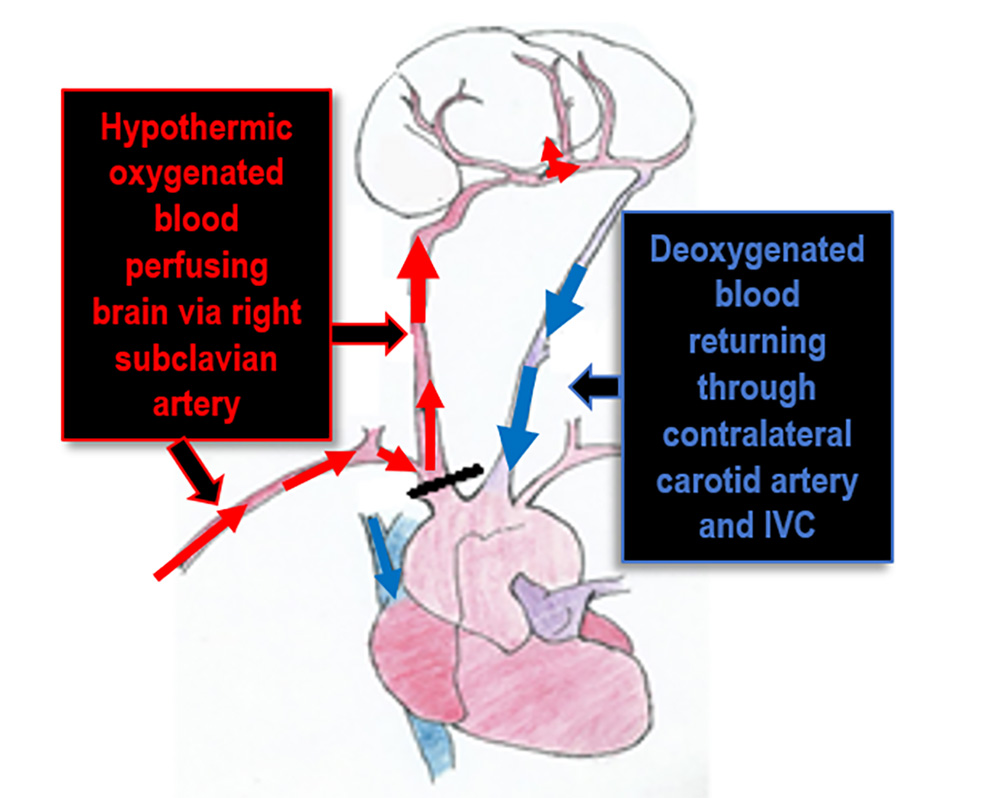
Figure 1: Selective antegrade cerebral perfusion. Original illustration by Ying Wang, Student at Brighton University
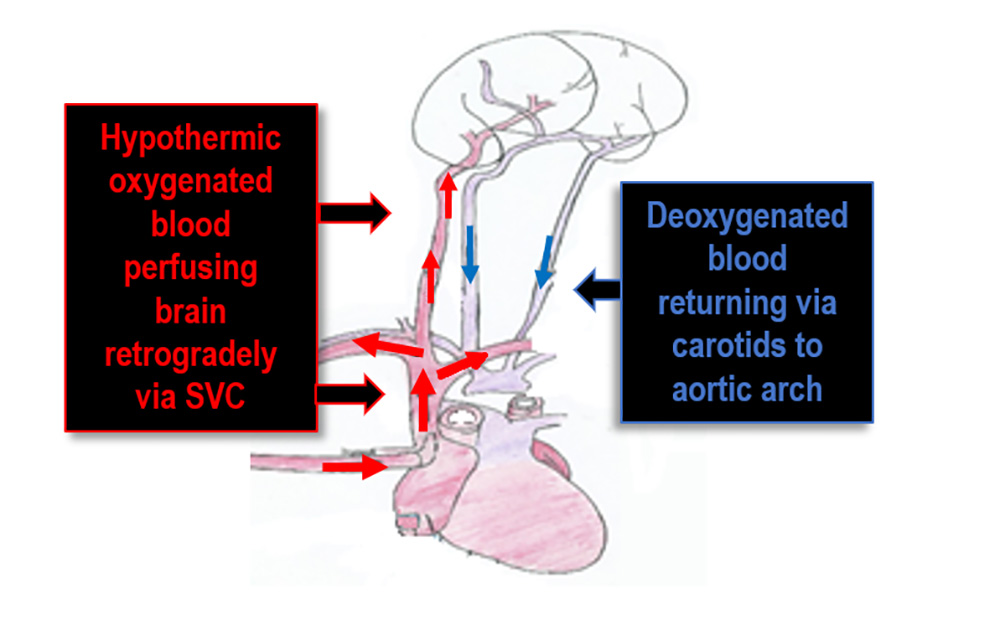
Figure 2: Retrograde cerebral perfusion Original illustration by Ying Wang, Student at Brighton University
SACP appears to have gained greater acceptance as the perfusion adjunct of choice in recent years however recent studies have shown comparable clinical outcomes to standard DHCA.12 SACP significantly increases the complexity of surgery but allows lesser degrees of hypothermia. RCP is a less complicated technique which is advantageous in emergency surgery and many authors now recommend using transcranial doppler to assess flow reversal rather than using an arbitrary perfusion pressure. Both techniques are not a replacement for DHCA, rather are used to extend and improve the technique to deliver the maximum neuroprotection.
SUMMARY
- DHCA remains an important technique in cardiac surgery and anaesthesia.
- Circulatory arrest is induced to facilitate surgery on the aortic arch whilst deep hypothermia is employed prevent ischaemic injury.
- Neurological monitoring and pharmacological neuroprotection are used in many centres to further reduce the risk of neurological injury.
- Anterograde and retrograde perfusion methods are increasingly being used to extend the duration of DHCA.
REFERENCES AND FURTHER READING
- Englum BR, Andersen ND, Husain AM, Mathew JP, Hughes GC. Degree of hypothermia in aortic arch surgery – optimal temperature for cerebral and spinal protection: deep hypothermia remains the gold standard in the absence of randomized data. Annals of Cardiothoracic Surgery. 2013;2(2):184-193.
- Ghariani S, Liard L, Spaey J, Noirhomme P H, El Khoury G A, de Tourtchaninoff M, Dion R A, et al. 1999. “Retrospective study of somatosensory evoked potential monitoring in deep hypothermic circulatory arrest.” The Annals of thoracic surgery 67 (6): 1915-8; discussion 1919-21.
- Chapter 14. Deep Hypothermic Circulatory Arrest. Cardiac Surgery in the Adult, 4e. Andrew W. El Bardissi; Robert A. Oakes; R. Morton Bolman III. Access Surgery.McGraw-Hill Medical
- Degree of hypothermia in aortic arch surgery – optimal temperature for cerebral and spinal protection: deep hypothermia remains the gold standard in the absence of randomized data Brian R. Englum1, Nicholas D. Andersen1, Aatif M. Husain2, Joseph P. Mathew3, G. Chad Hughes1
- Optimal temperature management in aortic arch operations Michael O. Kayatta1 • Edward P. Chen1 Gen Thorac Cardiovasc Surg (2016) 64:639–650
- Comparison of Two Different Red Blood Cell Transfusion Thresholds on Short-Term Clinical Outcomes of Patients Undergoing Aortic Surgery With Deep Hypothermic Circulatory Arrest Wang, Yongyuan et al. Journal of Cardiothoracic and Vascular Anesthesia (2016) Volume 30 , Issue 5 , 1163 – 1166
- Practice variations in the conduct of hypothermic circulatory arrest for adult aortic arch repair: focus on an emerging European paradigm. Gutsche JT1, Feinman J2, Silvay G3, Patel PP1, Ghadimi K1, Landoni G4, Yue Y5, Augoustides JG1. Heart Lung Vessel. 2014;6(1):43-51.
- Perioperative effects of alpha-stat versus ph-stat strategies for deep hypothermic cardiopulmonary bypass in infants du Plessis, Adre J. et al.
- Is pH-stat or alpha-stat the best technique to follow in patients undergoing deep hypothermic circulatory arrest? Khairul Anuar Abdul AzizAyo Meduoye CardioVasc Thorac Surg (2010) 10 (2): 271-282.
- Bachet, Jean What is the Best Method for Brain Protection in Surgery of the Aortic Arch? Selective Antegrade Cerebral Perfusion Cardiology Clinics , Volume 28 , Issue 2 , 389 – 401
- Ueda Y. A reappraisal of retrograde cerebral perfusion. Annals of Cardiothoracic Surgery. 2013;2(3):316-325. doi:10.3978/j.issn.2225-319X.2013.01.02. Anthony L. Estrera; Editorial Comment: Is retrograde cerebral perfusion dead?. Eur J Cardiothorac Surg 2013; 43 (5): 1071-1072. doi: 10.1093/ejcts/ezs564
- Anthony L. Estrera; Editorial Comment: Is retrograde cerebral perfusion dead?. Eur J Cardiothorac Surg 2013; 43 (5): 1071-1072. doi: 10.1093/ejcts/ezs56413. Perioperative effects of alpha-stat versus ph-stat strategies for deep hypothermic cardiopulmonary bypass in infants du Plessis, Adre J. et al. The Journal of Thoracic and Cardiovascular Surgery. Volume 114 Issue 6 , 991 – 1001



