Basic Sciences
QUESTIONS
Before continuing try to answer the following questions, the answers can be found at the end of the article.
- When is high frequency jet ventilation (HFJV) indicated?
- What advantages does HFJV have when used for ENT (ear, nose and throat) cases?
- The following statements are true or false:
a. Use of HFJV increases PAWP (peak airway pressure) and decreases MAWP (mean airway pressure)
b. In one-lung ventilation, selective HFJV of the non-dependent lung increases PaO2 compared with collapse of the non-dependant lung
c. HFJV reduces breathing-related liver motion from 12mm to 2mm
d. HFJV offers no benefit in a lung protective strategy of ventilation
e. HFJV reduces mortality when used for preterm infants with respiratory distress syndrome - List the mechanisms of gas exchange in HFJV
- The following statements are true or false:
a. The supraglottic approach causes the least rapid increase in airway pressures
b. PAWP monitoring is an advantage of the subglottic approach
c. It is impossible to determine the FiO2 delivered with the subglottic approach
d. Jet ventilation should never be commenced until the airway is open
e. There is an inverse relationship between trapped gas volumes and cardiac index - The following statements are true or false:
a. PAWP AND MAWP increase linearly as the expiratory time is shortened.
b. Minimal changes in cardiac index are observed with subglottic ventilation at frequencies of 300 bpm
c. The most effective way to increase CO2 elimination is to increase the driving pressure (DP) while leaving the frequency unchanged
d. The output of the ventilator is not influenced by external factors such as airway resistance or lung compliance
e. As essential safety feature is an automated cut-off when the pause pressure (PP) is exceeded - What complications are associated with HFJV?
INTRODUCTION
HFJV is a versatile, safe and effective technique with growing indications for elective and emergency use. This article aims to give the reader an understanding of the basic science necessary to practice HFJV safely, and increase familiarity with the equipment and techniques used.
DEFINITION
HFJV is characterised by delivery of small tidal volumes (1-3mls/kg) from a high pressure jet at supraphysiological frequencies (1-10Hz) followed by passive expiration.
INDICATIONS
HFJV is indicated when it offers advantages over conventional ventilation. These indications fall into two main categories; to facilitate surgical access and to optimise pulmonary function.
1. ENT
Diagnostic laryngoscopy requires a technique to provide an unimpeded view of the larynx, immobility of the vocal cords and complete control of the airway and ventilation. The delivery of small tidal volumes produces less vocal cord movement whilst high-pressure ventilation permits the use of narrow bore jet ventilation catheters. These impede surgical access less than conventional endotracheal tubes. Jet ventilation catheters are constructed from non-flammable, fluoroplastic material providing advantages for use in laser surgery by reducing the chance of airway fire.
2. Thoracic Surgery
As in ENT surgery, the passage of a narrow catheter through the surgical field causes much less interference with surgery than the passage of a standard or double-lumen endotracheal tube. If a major conducting airway has been divided, the narrow catheter provides a relatively unobstructed, accessible circumference of trachea and bronchus so that the ends of a divided airway can be aligned for construction of an airtight anastomosis.
Use of HFJV during one-lung ventilation can be advantageous. The non-dependent lung is held slightly distended, so minimising shunt by increasing MAWP, aiding perfusion and allowing carbon dioxide removal without necessity for large volume excursions. Selective HFJV of the non-dependent lung, while the dependent lung is ventilated with conventional intermittent positive-pressure, increases PaO2 compared with simple collapse of the non-dependent lung and conventional ventilation of the dependent lung (1).
HFJV has also been successfully used in the treatment of major bronchopleural fistulae and tracheobronchial disruptions. Decreased PAWP and tidal volumes result in smaller gas leaks through pathological low-resistance pathways. Consequently, mediastinal and interstitial emphysema may be minimized.
3. Radiology
HFJV can provide a motionless field, and is therefore advantageous in radiologically-guided procedures.
Radiofrequency Ablation (RFA)
Use of HFJV for CT-guided RFA of liver tumours minimises breathing-related liver motion, reducing it from 12mm to 2mm (2). RFA of the left atrium using HFJV yields a more stable left atrial environment with less variation in left atrium volume and fewer ablations required.
Lithotripsy
The elimination of diaphragmatic excursion is ideal for use in extra-corporeal shock wave lithotripsy as it reduces urinary calculus movement. This increases lithotripsy efficiency with better utilisation of shockwave energy and less patient exposure to tissue trauma (3).
4. Critical Care
HFJV is particularly well suited for lung protective ventilation strategies. Low tidal volumes reduce the risk of over-distension and volutrauma. Reduced pressure swings during the ventilatory cycle and increased MAWP optimise end-expiratory lung volume, preventing collapse and cyclic atelectatrauma. A Cochrane systematic review of elective HFJV versus conventional ventilation for respiratory distress syndrome in preterm infants showed no difference in mortality but showed benefit in pulmonary outcomes. Further prospective, randomised trials are needed in adults.
MECHANISMS OF GAS EXCHANGE
With conventional ventilation where tidal volumes exceed dead space, gas exchange is largely related to bulk flow of gas to the alveoli. With high frequency ventilation, the tidal volumes used are smaller than anatomical and equipment dead space and therefore alternative mechanisms of gas exchange occur.
- Pendelluft describes the movement of gas between lung units with different time constants – a property related to the product of compliance and resistance. Following inspiration, there is redistribution of inspired gas from full, fast-filling units to slower-filling units, augmenting gas exchange.
- Convective streaming or Taylor dispersion occurs as a result of the asymmetrical velocity profile of the inspired gas front as it moves through the bronchial tree. Molecules in the central zones where axial velocities are higher diffuse to lateral zones with lower axial velocities.
- Cardiogenic mixing describes how the beating heart enhances gas exchange through agitation of surrounding lung tissue and molecular diffusion.
- Bulk flow may contribute partially to gas exchange as the leading edge of the gas front may actually reach a number of proximal alveoli.
Detailed discussion of the mechanisms of gas exchange can be found elsewhere and is beyond the scope of this article.
THREE DIFFERENT APPROACHES
Jet ventilation can be applied via supraglottic, transtracheal or subglottic approaches. The advantages and disadvantages of each technique are discussed below.
Supraglottic Approach
The supraglottic approach is advantageous as it allows a completely tubeless surgical field. However supraglottic techniques require the airway to be maintained during the procedure by the surgeon, and the quality of ventilation can be impaired by malalignment of the jet with the airway during attempts to access the operative site. There is also greater vocal cord movement when compared to the other techniques and a risk of blowing debris into the airway. It is not possible to monitor PAWP or end-tidal CO2 (ETCO2) with the supraglottic approach.

Figure 1. Rigid bronchoscope with jet ventilator attached for supraglottic jetting
With all approaches, peak and mean airway pressures increase linearly with increasing frequencies as the expiratory time is shortened. The rate at which these pressures increase is influenced by the approach used. The greatest rate of increase in airway pressure is seen with supraglottic techniques and the slowest rate of increase is seen with subglottic techniques.
Theoretically, it may seem that subglottic techniques increase airway pressures most rapidly because the jet is applied distally and expiratory flow is limited by the glottis/stenosis, whilst with supraglottic techniques the jet is applied proximally, and the glottis/stenosis impedes inspiratory flow as well as expiratory flow, thus reducing the rate of increase in airway pressure. However, the converse is true. There are 4 reasons for this;
1. Venturi Effect – gas flow at a constriction speeds up causing a pressure drop and entrainment. Supraglottic jet ventilation is a true Venturi type of ventilation and the tidal volume is the sum of injected and entrained air.
2. Flow characteristics in conducting airways – turbulent flow exists in the conducting airways, with primarily laminar flow in distal airways and alveoli. Turbulent flow generated in the upper airway is conducted for a variable distance downstream and therefore a supraglottic point of injection creates a greater column of turbulent flow causing a greater resistance to expiratory flow and gas trapping.
3. Double jetting – when a supraglottic jet is applied some gas is reflected from the glottis/stenosis thereby increasing supraglottic pressure. This acts as a second high pressure jet source directing gas beyond the stenosis as well as creating an unfavourable pressure gradient for exhaust gases, thus impeding expiratory flow and increasing gas trapping.
4. Expiratory impedance – exhaust gas must be expired through the glottis/stenosis, which is only open during the expiratory phase of the cycle with supraglottic techniques. Expiratory impedance therefore depends on the inspiratory : expiratory (I:E) ratio and the area of the stenosis aperture.
Supraglottic techniques should be avoided in small diameter stenoses due to rapid increases in airway pressures. With larger diameter stenoses, supraglottic techniques provide more efficient gas delivery with greater distending pressures (Venturi and double jet phenomenon), which may be required in patients with low respiratory compliance. Caution must be excised to avoid excessive gas trapping.
Transtracheal Approach
Transtracheal techniques provide the surgeon with operating conditions unhindered by anaesthetic equipment, and the anaesthetist controls the airway and ventilation. Entrainment is minimal allowing a consistent FiO2.
Transtracheal HFJV may be hazardous with small diameter stenoses (D<2d where D = stenosis diameter, d = jet catheter diameter), because the stenosis aperture is partially obstructed by the jet catheter, increasing exhaust impedance. With stenosis diameter <4.5 mm, airway pressure during transtracheal jetting increases above that during subglottic jetting at equivalent stenosis size (4).
Subglottic Approach
The rate of increase in airway pressure is reduced with subglottic techniques. Supraglottic/stenotic pressures remain atmospheric and the pathway for exhaust gases is open throughout the ventilatory cycle, reducing expiratory impedance and gas trapping. Subglottic techniques also produce consistent delivered oxygen concentrations since entrainment is minimal. PAWP and ETCO2 monitoring is also possible with the subglottic technique. This is not a completely tubeless technique and may impede surgical access to posterior glottis particularly.

Figure 2.1 Subglottic jet ventilation in practice

Figure 2.2 Transtracheal jet ventilation in practice
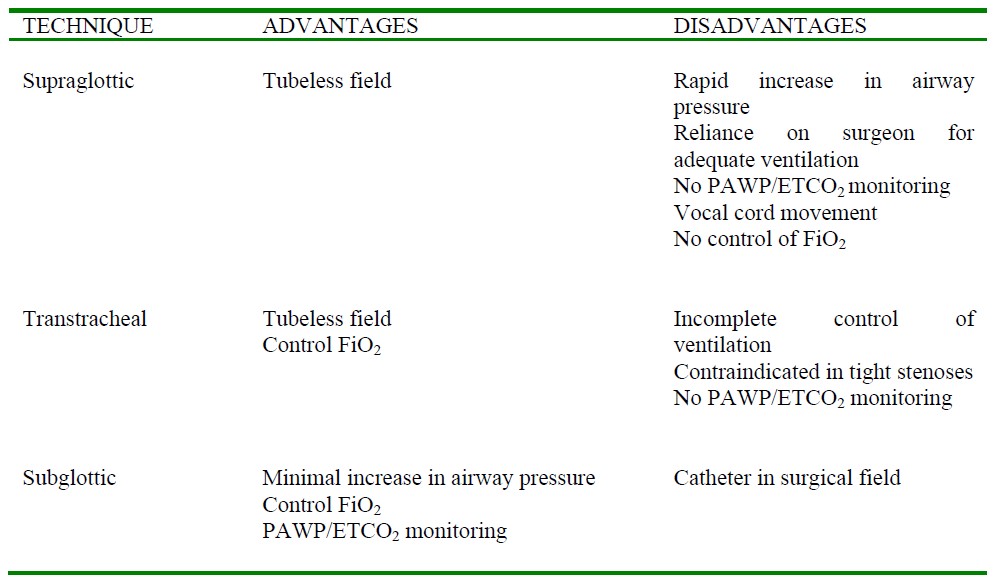
Table 1. Advantages and disadvantages of each approach
COMPLICATIONS OF HFJV
Barotrauma
Many complications associated with HFJV are due to use of a high pressure gas source. The high pressure jet may cause a rapid increase in airway pressure due to gas trapping if there is an inadequate expiratory pathway.
Increasing ventilation frequency and I:E ratio makes gas trapping more likely, and small diameter stenosis of the airway also predispose to this. Gas trapping impairs cardiac output; There is an inverse relationship between trapped gas volumes and cardiac index. Right ventricular end-systolic volume (RVESV) shows a direct relationship with ventilatory frequency. As the intrathoracic pressure rises, venous return is reduced and right ventricular (RV) afterload increased (due to compression of pulmonary vasculature). The relatively weak RV fails to cope with this increased afterload and may cause a complete loss of cardiac output.
Excessive gas trapping is not an inevitable consequence of jet ventilation. Small amounts of gas trapping and minimal changes in cardiac index can be observed with subglottic ventilation at frequencies of 150 bpm.
Exposure to dry gas
HFJV without humidification limits the duration of use. Prolonged exposure to dry gases under pressure causes traumatic airway injury leading to necrotising tracheobronchitis, atelectasis, loss of ciliated epithelium, mucosal inflammation, and excessive mucous and airway plugging. High frequency jet ventilators (Monsoon, Acutronic Medical Systems) which deliver humidified gas can be used for longer periods.
Hypercapnia
CO2 elimination is dependent on the frequency, and tidal volume raised to the second power. Tidal volume is modulated by canging the Driving Pressure (DP), and the most effective way to increase CO2 elimination is to increase the driving pressure while leaving the frequency unchanged. Large increases in DP and frequency reduce CO2 elimination as expiratory time for exhaust of gases is reduced.
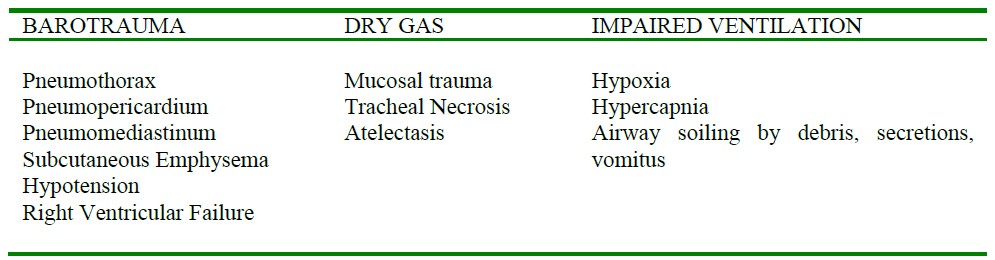
Table 3. Complications of HFJV
EQUIPMENT
High frequency jet ventilators
In the UK, the Mistral or Monsoon jet ventilator (Acutronic Medical Systems) is most commonly used. Their description cover the main principles of high-frequency jet ventilators.
The Mistral jet ventilator is an electrically powered, solenoid cycled, automatic, high frequency jet ventilator. The ventilator is supplied with compressed air and oxygen at 4 atmospheres from the hospital supply system. After passing through a pressure regulator, the gas reaches a manifold of four electromagnetic solenoid valves in parallel, which are closed in the resting position. When the solenoids are excited, one or more valves open, thus generating a discrete pulse of gas.
The volume of each pulse is determined by setting the respiratory frequency, I:E ratio, and DP. For example, increasing the frequency or decreasing the DP reduces the tidal volume, whilst increasing the inspiratory time or increasing the DP has the opposite effect. The output of the ventilator is not influenced by external factors such as airway resistance or lung compliance.
An essential feature of the ventilator is an airway pressure alarm and automated cut-off when the airway pressure exceeds a set limit. This limit is set as the pause pressure (PP), which is the pressure inside the airway and is measured from the tip of the jet ventilation catheter between each jet. The PP approximates the mean airway pressure. A PP exceeding the preset value results in activation of an alarm and suspension of further ventilation.

Figure 3. Mistral Jet Ventilator
Jet ventilation catheters
Supraglottic techniques employ ‘tubeless’ HFJV, with jet ventilation catheters used for transtracheal and subglottic approaches.
Subglottic catheters
Both the Hunsaker Mon-Jet and LaserJet catheters are double lumen catheters specifically designed for subglottic HFJV. Both have a metal stylet to aid intubation and are made of nonflammable, laserresistant material.
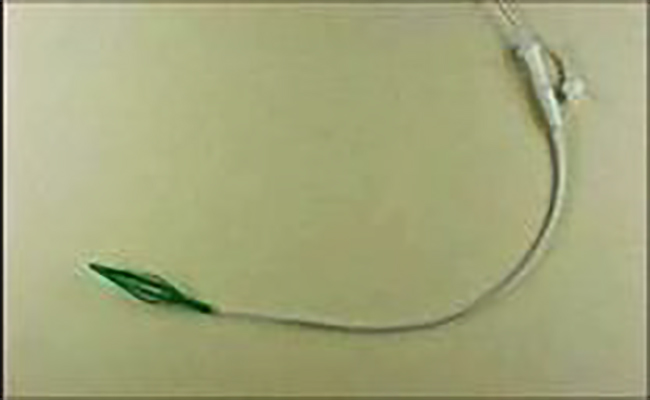
Figure 4. Hunsaker Mon-Jet Catheter (Medtronic Xomed)
The Hunsaker Mon-Jet catheter was designed specifically for microlaryngeal procedures. It is 35.5 cm long with an internal diameter of 2.7mm and an external diameter of 4.3mm. The ventilator is attached to the central lumen, with gas exiting through an aperture at the tip of the catheter. A monitoring port at 3.2 cm above the tip allows pressure and ETCO2 to be measured. The green basket at the distal end self-centres the tube within the trachea, aligning the jet away from tracheal mucosa to prevent trauma and submucosal injection of jetted gas.

Figure 5. LaserJet Catheter (Acutronic Medical Systems)
The LaserJet Catheter comes in two lengths, 40 or 70 cm. Both have an external diameter of 3.4 mm. As with the Hunsaker, there are two lumens, one for delivering gas and one for monitoring airway pressure and ETCO2.
Tube length can be gauged by approximating the length from the lips to the glottis by placing the tube alongside the patient’s airway prior to insertion. The red cuff surrounding the tube can then be positioned at the correct point to coincide with an appropriate position at the lips.
Transtracheal catheters
Many transtracheal catheters are available. One of these is the Ravussin jet ventilation catheter, which is available in three sizes; 13G, 14G and 16G for adults, children and infants respectively. They are kink resistant and are also used in manual jet ventilation.

Figure 6. Jet ventilation catheter acc. to Ravussin (VBM Medizintechnik GmbH-Germany)
TECHNIQUE
Many techniques exist based on patient characteristics, surgical requirements and anaesthetic experience. It is impractical to produce an exhaustive list of these so I will describe a technique used in my establishment.
If a LaserJet catheter is used, the length of insertion should be determined by approximation, laying the catheter next to the airway. The red cuff is then positioned as a guide to depth of insertion. Most often, the stylet is removed as the catheter is rigid enough alone.
Anaesthesia is induced using an intravenous agent, following which low-dose neuromuscular blockade is administered and direct laryngoscopy performed. Unless using an additional ventilator to deliver anaesthetic vapours via superimposed conventional ventilation, it is necessary to adopt a Total Intravenous Anaesthesia (TIVA) technique.
Although our practice is to use neuromuscular blockade, it is possible to pass the narrow, less stimulating jet ventilation catheter without neuromuscular blockade using alternative techniques, for example topical local anaesthetic. The catheter is introduced and secured with tape on the left side of the patient’s mouth. This is to facilitate surgical access from the right. Jet ventilation is not commenced at this point, and the patient is ventilated with a bag and mask until positioned on the operating table with the airway open. Alternatively, ventilation can be achieved via a laryngeal mask until the airway is open and HFJV can commence.
Once the airway is open, HFJV is started. The jet ventilator is attached to the central lumen of the catheter and the capnography and pressure tubing is connected to the monitoring lumen, both via luerloc to prevent disconnection under pressure. Initial ventilator parameters are set; It is usual to commence at a frequency of 100-150 per minute, with a DP of 1.0-1.5 bar, PP of 20 mbar and FiO2 of 1.0. These parameters are adjusted to achieve greatest efficacy and the fewest negative effects. Adequacy of ventilation is assessed by direct observation and palpation of chest wall movement along with monitoring of SpO2.
ETCO2 is monitored throughout, although this will not provide accurate estimation of arterial carbon dioxide tension due to the small tidal volumes and the slow response of carbon dioxide analysers. Interrupting jet ventilation with a conventional positive pressure breath overcomes this problem. An accurate reading can be obtained by turning the jet off and compressing the patient’s chest to cause a tidal expiration.
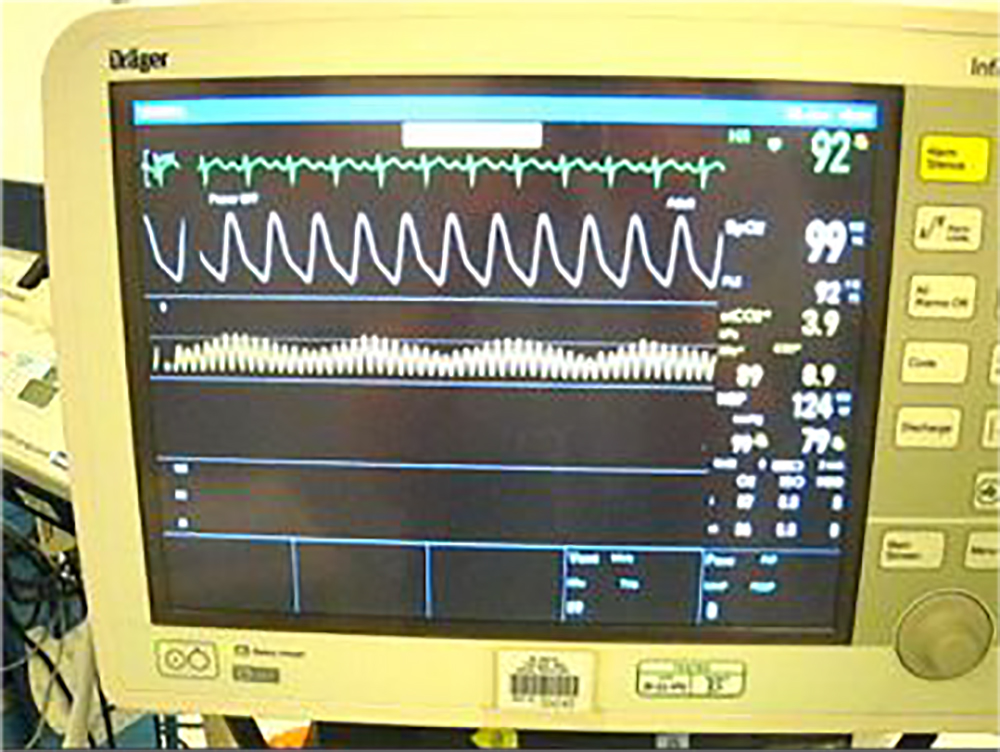
Figure 7. Capnograph during HFJV technique
When surgery is completed and the patient shows signs of respiratory effort, the jet ventilator is switched off. Supplemental oxygen is delivered via a bag and mask and the catheter removed in the same way as a standard endotracheal tube.
REFERENCES AND FURTHER READING
- Abe K et al. Effect of high-frequency jet ventilation on oxygenation during lone-lung ventilation in patients undergoing thoracic aneurysm surgery. J Anaeth 2006;20(1):1-5
- Biro P et al. High-frequency jet ventilation for minimizing breathing-related liver motion during percutaneous radiofrequency ablation of multiple hepatic tumours. Br. J. Anaesth 2009;102(5):650-653
- Canty D J, Dhara S S. High frequency jet ventilation through a supraglottic airway device. Anaesthesia 2009;64:1295–1298
- Buczkowski P W et al. Air entrainment during high-frequency jet ventilation in a modelo f upper tracheal stenosis. Br. J. Anaesth 2007; 99(6):891-897
ACKNOWLEDGEMENTS
Many thanks to Dr Radhika Bhishma (North Manchester General Hospital) for guidance on writing the article and Dr Patrick Wong (St George’s Hospital) for guidance and figures.
ANSWERS TO QUESTIONS
- When it provides advantages over conventional ventilation
- Immobility of vocal cords, unimpeded view, laser-safe catheters
- FTTFF
- Bulk flow, pendelluft, convective streaming, cardiogenic mixing
- FTFTT
- TFTTT
- See table in text



