General Topics
PART 1: TECHNICAL ASPECTS, A STANDARD INTERPRETATION. ROUTINE AND COMMON ABNORMALITIES OF THE CHEST RADIOGRAPH
This is part 1 of a 3-part series of tutorials. Parts 2 and 3 will focus more specifically on the chest radiograph changes commonly seen on the intensive care unit.
MULTIPLE CHOICE QUESTIONS
- Concerning the normal chest radiograph:
- The right mediastinal border is formed by the right brachiocephalic vein, SVC and right hilum
- The right hilum lies 1-2 cm above the left
- The horizontal fissure runs from the hilum to the 6th rib in the axillary line
- The right ventricular border is visible on the frontal film
- Concerning the frontal chest radiograph:
- The medial heads of the clavicles should be equidistant from the tracheal midpoint in an unrotated film
- An adequate breath should result in 5 rib ends visible anteriorly
- Sternal fractures are readily visible
- Obscuration of the right heart border indicates right lower lobe disease
- Concerning the frontal chest radiograph:
- The cardiothoracic ratio should be less than 1:2 on the PA film
- This ratio is decreased in expiration
- The lingula is considered to form part of the left lower lobe
- The oblique fissure is visible on the frontal film
INTRODUCTION
The chest radiograph, or X-ray (CXR) is one of the commonest investigations requested for intensive care patients. Its correct interpretation is therefore an integral skill for ICU clinicians. As with history and examination skills, a structured approach is necessary to avoid missing important signs. Interpretation of the CXR does not take the place of a good history and examination, but should be seen as an extension of the examination process. A firm grasp of the normal chest film is an essential start point.
This article does not aim to cover all aspects of CXR interpretation, rather to give an introduction to interpretation and highlight aspects which are particular to intensive care patients.
TECHNICAL ASPECTS
The chest is imaged by positioning the patient between an X-ray source and an X-ray sensitive plate. The distance from the source to the patient is relatively great compared to the distance from the patient to the plate in order to reduce magnification of the image and problems of rotation of the structures within the patient. Even so, the structures nearest the plate will have their size most faithfully
represented, whereas those furthest from the plate will be subject to a small but significant degree of magnification. The patient may be orientated in several ways:
- anterior-posterior (‘AP’ – with the patient facing the source, standard in ICU, lower radiation dose, quality affected by rotation)
- posterior-anterior (‘PA’ – with the patient facing the plate, higher xray dose, less affected by rotation) or
- lateral, expiratory, lordotic or decubitus
This discussion will be confined to AP and PA films since these are by far the most common on intensive care. The term frontal view will be used to represent PA or AP collectively in contrast to lateral views.
Different tissues absorb X-rays to different extents, resulting in a spectrum of exposures onto the plate and a corresponding spectrum of shades of grey on the final film. High density (radio-opaque) tissues such as bone and metal (e.g. prosthetic heart valves, coronary stents) appear white. Low-density (radiolucent) tissues such as air appear black. Fluid (e.g. blood, consolidation) and fat are moderately absorbent and therefore appear grey.
Standard Assessment Routine
Interpretation of the CXR can be considered in three stages: preliminaries, the film itself, and synthesis of these abnormalities into a differential diagnosis
1. Preliminaries
It is common for students to be asked to interpret a CXR in front of peers or seniors only seconds after it has been brandished in front of their eyes. A careful introduction to the film in question is not only important to avoid assigning abnormalities to the wrong patient, but also allows a few extra seconds to scan the film. Check the following:
Name
Is the radiograph from the patient you’re interested in discussing?
Date
Is the date of the CXR the date you were expecting? Intensive care patients typically accrue several CXRs on their journey to the ICU, and may even have films from when they were clinically well
Orientation
- Is this an AP or a PA film – look for this written on the film, or the comment “supine” suggesting an AP film.
- Is the film displayed the correct way around? Look for the “L” or “R” markers added to the film.
More cruel examiners have been known to present a CXR of a patient with dextrocardia the wrong way around to see if students check the orientation markers placed by the radiographer
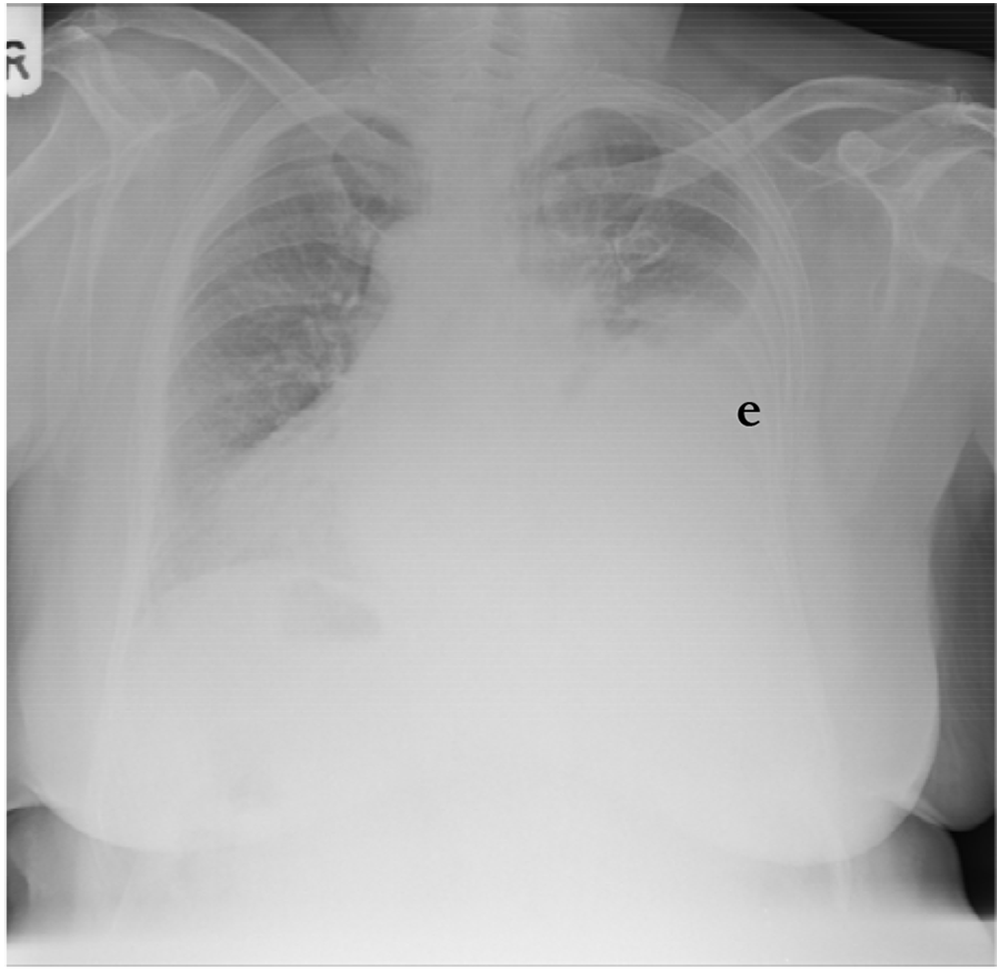
Figure 1. CXR of a patient with dextrocardia. Note the white orientation tab in the top left of the film (“R”) confirming that the film has been displayed the correct way around. This patient also has a left sided pleural effusion (e)
Adequacy
Can you see the area you need to see? Check the lung apices are visible. If the CXR was indicated for naso-gastric tube placement then check it is visible. Ideally an adequate breath allows five ribs to be visible anteriorly.
Rotation
The medial ends of the clavicles should be equidistant from the spinous processes that project between the clavicular heads. This is shown in figure 2 in the upper inset. The dimension A equals the dimension B.
Penetration
Three lower thoracic vertebrae and the pulmonary vessels to the left lower lobe should be visible through the cardiac silhouette. This is shown in figure 2 in the lower inset.
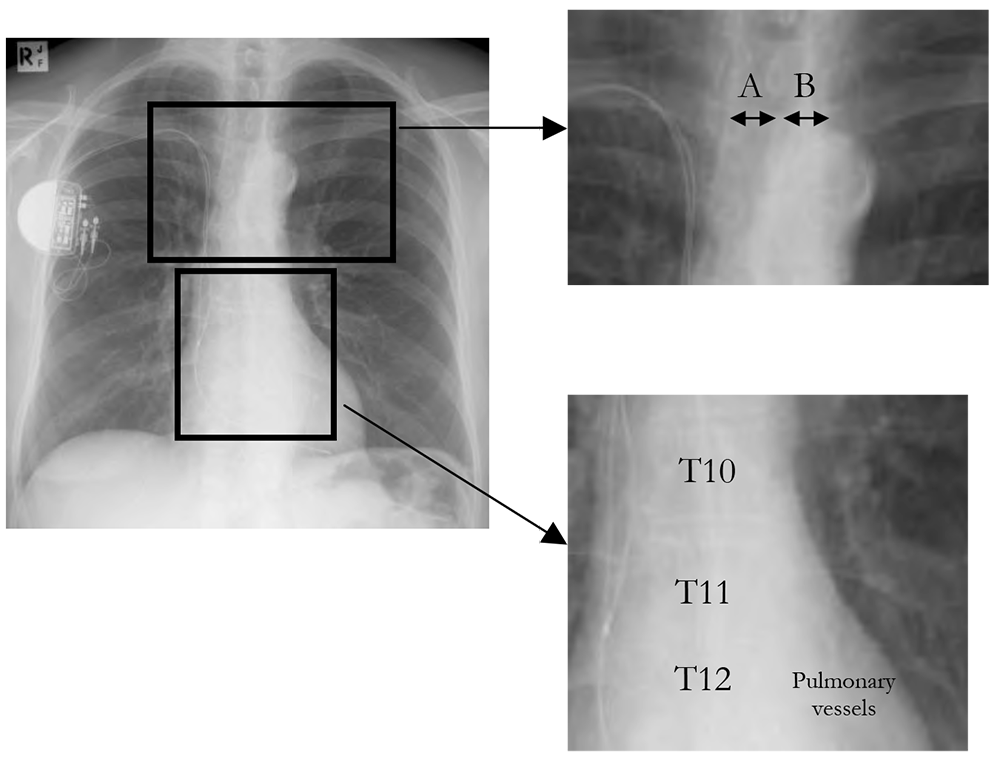
Figure 2. Illustration of how to check for non-rotation and for adequate penetration. The film is otherwise normal, with the addition of a pacemaker with atrial and ventricular wires.
Lines
Most patients in intensive care will have evidence of monitoring as well as tubes in the trachea, the stomach, the oesophagus or the pleural cavities. It is important both to acknowledge their presence, to comment on whether they are correctly placed and to consider what this might suggest about the disease processes within the patient – a history of dyspnoea and an endotracheal tube visible on CXR should trigger a mental note to look thoroughly for signs of lung disease.
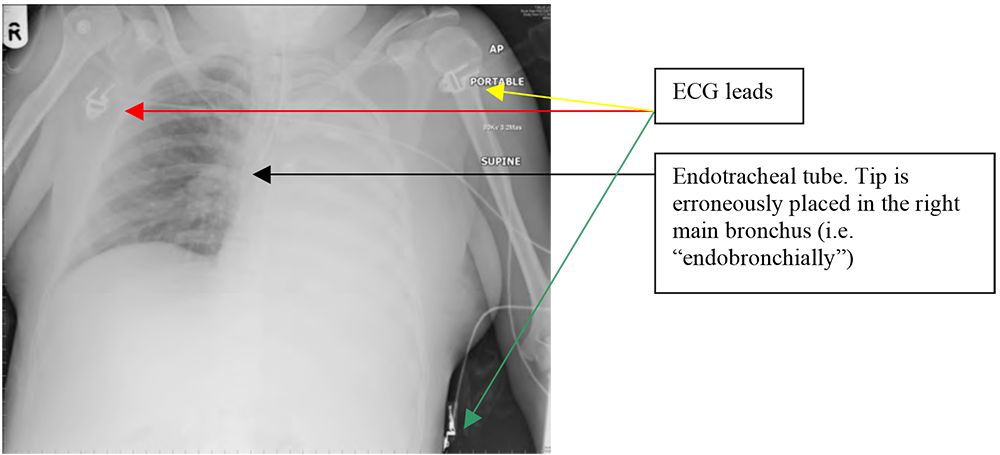
Figure 3. CXR showing a left sided white-out. Examination of the “lines” aspect of the film (ECG leads and a misplaced endotracheal tube) will quickly lead to the diagnosis – the endotracheal tube is endobronchial, leading to a left lung collapse.
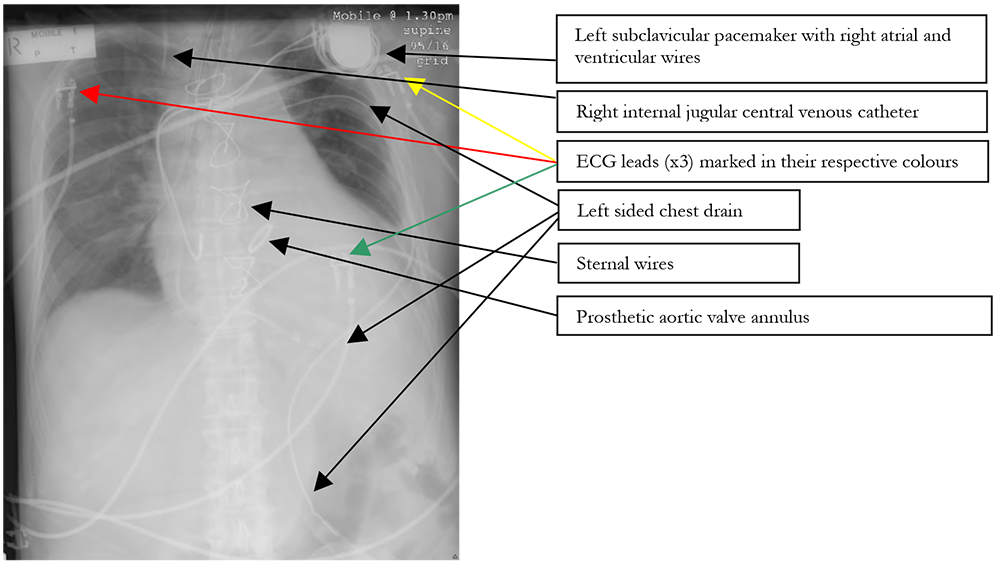
Figure 4. In some patients the discussion of lines may take some time! This patient has ECG leads, a left sided chest drain, sternal wires, an aortic valve replacement, a left subclavicular pacemaker, a naso- gastric tube and a right internal jugular central venous catheter.
2. The Film
The majority of the film is taken up by lung and cardiac tissue, and indications for requesting a chest radiograph often relate to perceived lung disease. It seems logical therefore to start with these areas. A good understanding of normal anatomy is important. The image is traditionally displayed in reverse with the patient’s left side shown on the right side of the film, and vice versa. Initial examination of the chest film should always confirm that the viewer is looking at the film the intended way around!
The Lungs and Lung Fissures
Since most of the lung consists of air, which is essentially transparent to X-rays (“radiolucent”) the only structures which are visible in normal lungs are the blood vessels, the interlobar fissures and the walls of some larger bronchi seen end on.
The right lung is divided into three lobes by means of two fissures: oblique and horizontal. The oblique fissure runs from a position anterior on the diaphragm in a posterior direction superiorly towards the apex of the lung around T4 posteriorly, splitting the lung into an anterior, superior section (the upper and middle lobes) and a posterior, inferior section (the lower lobe). The horizontal fissure runs from the anterior wall of the lung to the hilum, horizontally, dividing the upper section of the right lung into an upper lobe and a middle lobe. On the PA film, only the horizontal fissure is visible running from the right hilum to the region of the sixth rib in the axillary line.
The left lung is divided into two lobes, an upper and a lower, by an obique fissure similar to the right lung. The lingula, or remnant of the middle lobe on the left, is considered to form part of the upper lobe.
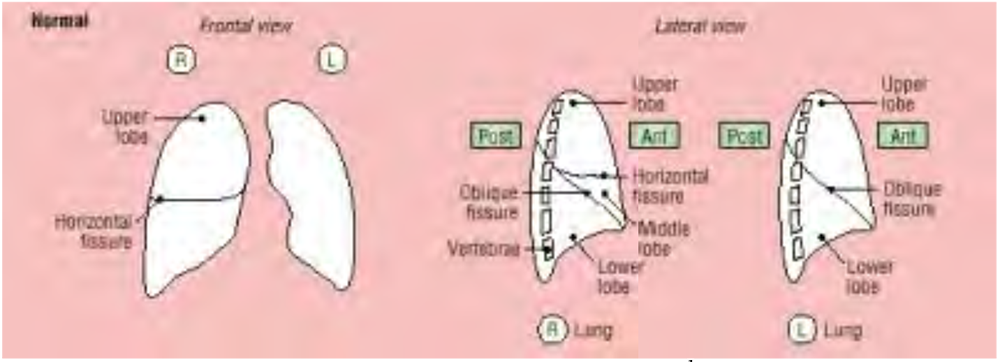
Figure 5. Anterior and lateral views of the lungs on CXR.1
Consideration of the anatomy makes it clear that examining the chest anteriorly can only detect signs in the upper and middle lobes on the right side, and mainly only in the upper lobe on the left side. Posterior examination findings – apart from the very apex of the lung – relate entirely to disease processes in the lower lobes on either side. Many intensive care patients are more easily examined anteriorly than posteriorly, which should be borne in mind when correlating clinical and radiological findings.
Traditionally the chest radiograph is loosely divided into upper, middle and lower zones, and thus comments about particular lobes can be avoided where interpretation is difficult. The lung fields should be scanned methodically from upper to lower zones, with particular attention paid to the apices and the area behind the heart. In case of doubt, it may be useful to compare radiolucency between sides, while being aware that a rotated patient will, of itself, lead to a difference in lucency between the two sides. Areas of abnormality can be described by zone (e.g. “right upper zone”) and by density. Low-density (“see through” or “radiolucent”) areas are black, higher density areas (“radio-opaque”) areas are white.
Clinicians should be aware that at least one third of the lung volume is not visible on a frontal film since the anterior attachment of the diaphragm obscures its appearance.
The silhouette sign is a useful tip in distinguishing which section of the lung is affected by a disease process. If two areas of similar density are placed next to each other, they will blend into one shadow on CXR – the border will be “lost”. If however the border is still visible, then the appearance is due to superimposed areas of similar density. This logic is most commonly applied when a clinician notices the loss of a border which is normally visible. For example: right hemidiaphragm not visible?…right lower lobe disease present, left hemidiaphragm not visible?…left lower lobe disease present. “Loss” of the left and right cardiac borders represents lingular and right middle lobe fluid respectively. Further detail on differentiating different disease processes in the lungs is discussed in the “Common Abnormalities” section in part two.
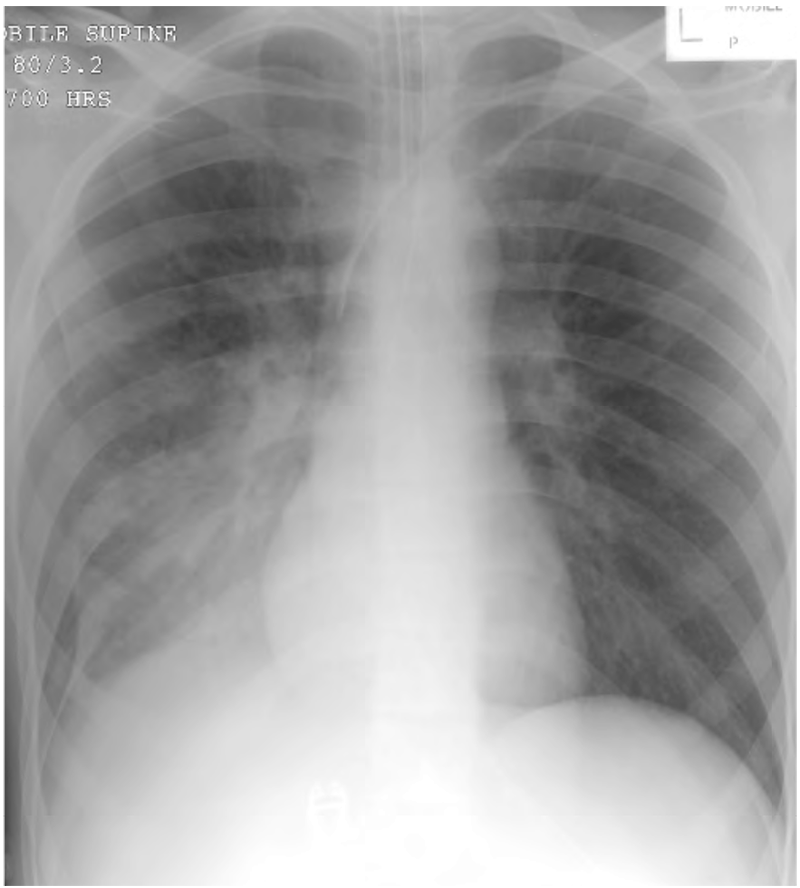
Figure 6. “Loss” of the right hemi-diaphragm (A) indicating right lower lobe disease.
The Heart
From superior to inferior the right side of the mediastinum and cardiac outline consists of the right brachiocephalic vein, the superior vena cava, the right hilum (consisting of the right main pulmonary artery), the right atrium and lastly the inferior vena cava which ultimately pierces the right hemi-diaphragm. The left side of the mediastinum and cardiac outline consists of the arch of the aorta, the pulmonary trunk, the left atrium and the left ventricle. All the borders of the heart should be apparent, apart from where the heart lies on the left hemidiaphragm.
The position of the heart is variable, though “traditionally” one third of the cardiac silhouette lies to the right of the midline, two thirds to the left. The ratio of the width of the heart to the internal width of the thorax should be less than 1:2. Remember that this ratio will increase in expiration, on AP films and when the diaphragms are elevated.
Hilar regions
The appearance of the hila consists of shadows created by pulmonary arteries, upper pulmonary veins, and any abnormal lymphadenopathy. In the normal film, they should be of equal density and size with the left hilum 1-2cm above the right.
Bony Anatomy
Chest X-rays display the ribs, the sternum and both clavicles and humeri.
Ribs
Both anterior (to the sternum) and posterior (to the spinal vertebrae) attachments of the ribs are visible on the chest radiograph. It is important to be clear on differentiating the two. The posterior ribs lie horizontally, whereas the anterior ribs slope inferiorly joining the costochondral cartilages, which are of lower density than bone, are therefore relatively radiolucent, and so appear darker than bone.
Sternum
The sternum is difficult to discern on a frontal view, and patients with clinical suspicion of sternal fractures require either lateral plain films or more detailed imaging such as computed tomography (CT) or magnetic resonance imaging (MRI) if available.
Clavicles and Humeri
Clinicians should be aware that some comment on these bones is possible via a chest X-ray, though clinical suspicion may require further imaging.
Diaphragm
The diaphragm is considered in two halves (left and right “hemidiaphragms”) though anatomically there is only one diaphragm. The right hemidiaphragm is higher than the left, on full inspiration dropping to the level of the sixth rib anteriorly. If the diaphragm is not clearly seen it indicates fluid in the adjacent lung tissue (lower lobes both sides).
Alternatively, if the patient is sitting upright or standing, the hemidiaphragm may prevent gas in the abdominal cavity rising out of the abdomen. This leads to a hemidiaphragm clearly outlined on both sides indicating free gas in the abdomen. This may be due to recent surgery or an abnormal communication between the bowel and peritoneum such as a perforation or post-operative wound dehiscence.
Soft Tissues
Remember to check axillae for massive lymphadenopathy, the thoracic wall for surgical emphysema and in female patients that both breast shadows are present. Mastectomy and a pleural effusion…? Consider recurrent malignancy.
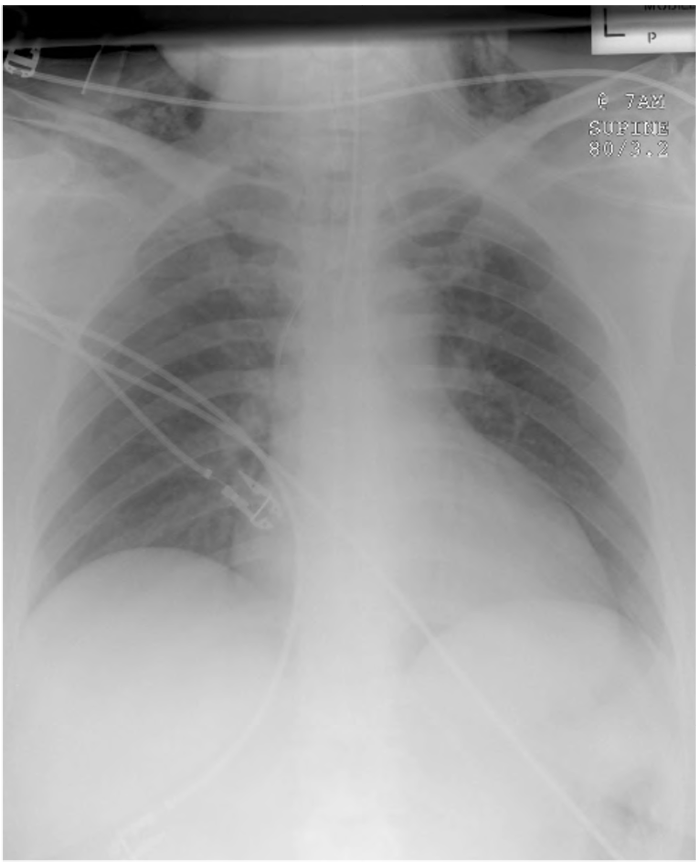
Figure 7. Surgical emphysema visible particularly in the neck
The Abdomen
An abdominal film is often more appropriate for suspected abdominal disease. Certain exceptions exist: a CXR may be taken to look for intraperitoneal “free” gas as it rises up and collects under the diaphragm. Subdiaphragmatic abscesses, gallstones, dilated loops of bowel and the whereabouts of a naso-gastric tube may all be evident. Don’t miss them.

Figure 8. Free gas is clearly evident under the right hemidiaphragm
Problematic Areas
Certain areas on the CXR are notoriously difficult to view. Special effort should be made to look at these areas to avoid missing subtle findings. Areas include:
- Lung apices
- Soft tissues
- Behind the heart
The following three figures illustrate the difficulties involved:

Figure 9. Hiatus hernia behind the heart, clearly visible. Note the fluid level within the stomach.
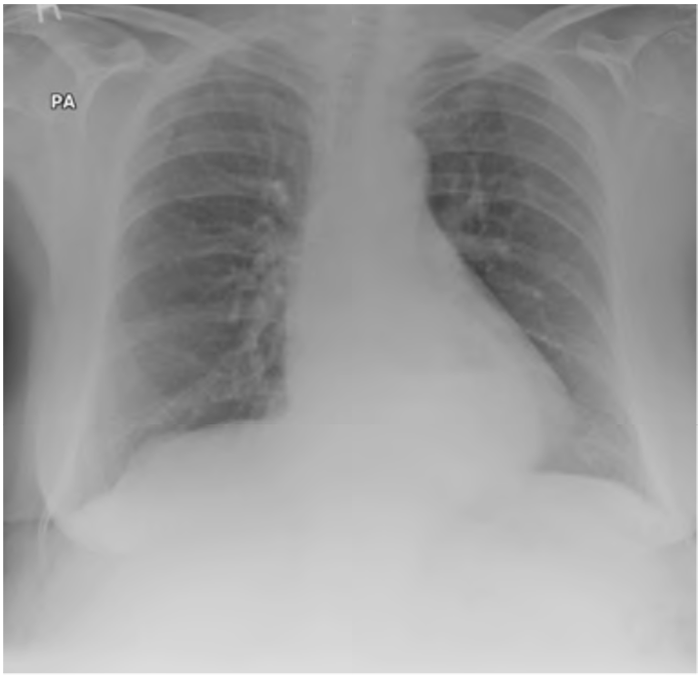
Figure 10. A more subtle hiatus hernia, though the fluid level is also visible on careful inspection.
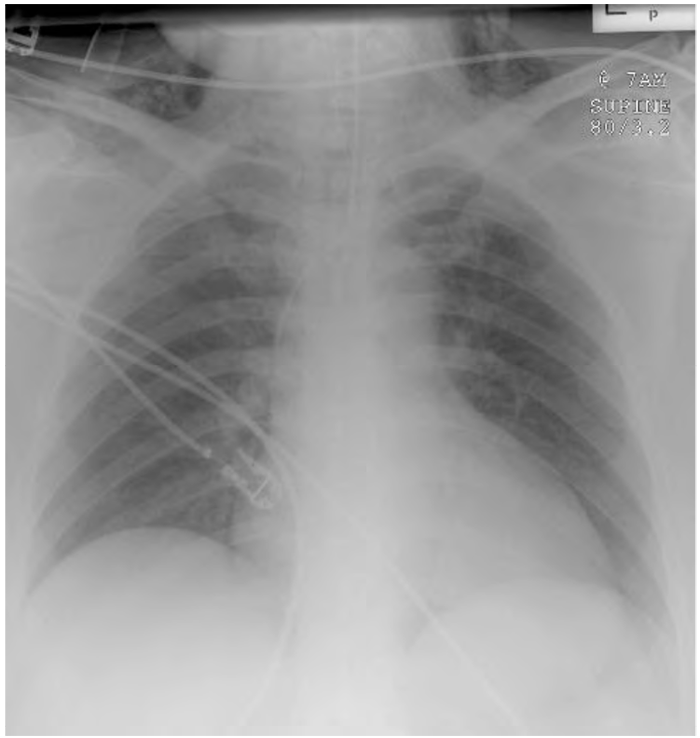
Figure 11. Surgical emphysema. Visible in the soft tissues of the neck. ECG leads, an endotracheal tube and a left subclavian central venous catheter are also visible.
3. The Synthesis
Two possible methods are suggested for summarising.
1. If the clinician feels confident of the diagnosis then open with this, and follow it with supportive evidence and pertinent negatives. For example:
“This 56 year old gentleman, who presented with shortness of breath, has a left sided pneumothorax. I note the retracted lung edge in the left hemithorax and an absence of lung markings distal to the lung edge. The trachea is central. The CXR is otherwise normal.”
Brief discussion of management should follow.
2. If the candidate does not feel confident of the diagnosis then it is reasonable to summarise the positive findings and suggest a differential. This may happen because the positive findings have been missed, or because the findings are difficult to put together. There is no shame in this – findings may be subtle (only found in an examiner’s head) and findings may not reflect the textbook descriptions. Say what you see! Either way, in an exam situation the structure is helpful as it lends itself naturally to discussion and gentle prodding by the examiner. For example, in the above case:
“This is a CXR of a 56 year old gentleman, who presented with shortness of breath. I note increased radiolucency in the left hemithorax in comparison to the right. Otherwise the CXR appears normal. My differential would include an exacerbation of chronic obstructive airways disease, an evolving pneumonia… and a pneumothorax”
MULTIPLE CHOICE ANSWERS
- Concerning the normal chest X-ray:
- True
- False – the left hilum lies higher than the right
- True
- False – the right ventricle is anterior and has no border on the frontal film
- Concerning the frontal chest film:
- False- they should be equidistant from the spinous processes of the vertebrae
- True
- False
- False-this indicates right middle lobe disease
- Concerning the frontal chest film:
- True
- False
- False
- False
REFERENCES
- The Chest X-ray made easy. Dick, Elizabeth Student BMJ 2000;8: 316-317.
ACKNOWLEDGEMENT
Many thanks to Bruce McCormick for his advice on the manuscript, and to Bruce McCormick and Andrew Lockwood for the use of their collections of CXRs.
BIBLIOGRAPHY
- Howling S, Jenkins P. Radiology for MRCP. Cheshire, UK: PasTest; 1998.
- Raby N, Berman L, de Lacey G. Accident & Emergency Radiology. 2nd ed. London: Elsevier; 2005.
- Chan O. ABC of Emergency Radiology. 2nd ed. Oxford, UK: Blackwell; 1995.
- Patel PR. Lecture Notes on Radiology. Oxford, UK: Blackwell; 1998.



