Intensive Care Medicine
Key Learning Points:
- Severe traumatic brain injury in children is associated with a high incidence of morbidity and mortality.
- The clinician can reduce the impact of secondary brain injury, especially by avoiding hypoxia and hypotension.
- The most important initial interventions are control of the airway and cervical spine, breathing and circulation.
- Surgically correctable lesions are uncommon but must be actively sought and treated
QUESTIONS
Answer the following multiple-choice questions before you begin the tutorial. The correct answers will be found in the tutorial:
- In infants:
- Sudden rise in intra cranial pressure is not dangerous as the suture lines and fontanelles are still open
- Intracranial pressures are between 2 and 10 mmHg
- The mean arterial blood pressure is lower than in older children
- The brain has a ready store of oxygen for metabolism
- Hypovolaemia may be secondary to an intracerebral bleed in a neonate.
- Cerebral blood flow
- Increases in the presence of hypoxia
- Decreases in the presence of a raised pCO2
- Increases with fall in the body temperature
- Varies according to mean arterial blood pressure under normal conditions
- Decreases during seizure activity
- When a child with a head injury comes to the hospital
- The first step is to establish a patent airway
- Taking history that indicates mechanism of injury is not very important
- 0.45% saline with dextrose is the first choice of intravenous fluid to maintain blood pressure
- Blood glucose level should always be checked
- Patient’s core temperature should be maintained below 35 degrees centigrade.
- With regards to analgesia and anaesthesia for children with head injury
- All inhalational anaesthetics increase cerebral blood flow
- All intravenous anaesthetic agents reduce cerebral blood flow
- Suxamethonium can be used cautiously for rapid sequence induction
- Ketamine is the induction agent of choice
- Providing good analgesia may help management of intracranial pressure
- The following are the indications for tracheal intubation in paediatric head trauma
- GCS < 8
- Inadequate respiratory effort
- Patient who is very agitated with a potentially severe head injury
- Facial and neck injuries
- Seizures
- The following indicate a severe head injury
- GCS < 8
- Fracture of skull
- Penetrating injury to the skull
- Failure to localise a painful stimulus
- Nausea
- Clinical suspicion of a severe head injury in a child warrants the following
- Cervical spine immobilisation
- Maintenance of mean arterial blood pressure of over 60 mm of Hg.
- Hyperventilation to maintain end tidal carbon dioxide at 3.5 mm of Hg
- Head CT scan
- Referral to paediatric intensive care unit if possible
INTRODUCTION
Trauma is an increasingly common cause of serious morbidity and mortality around the world, and children are particularly vulnerable. Children who have severe traumatic injuries are usually pedestrians involved in road traffic accidents and head injuries occur in approximately 75% of these patients. Of those that survive severe traumatic brain injury, many are left with significant behavioural, cognitive, emotional and physical damage.
This tutorial will consider the pathophysiology of paediatric traumatic brain injury, and simple steps that can be taken to improve outcomes in a resource poor environment.
PATHOPHYSIOLOGY
The disproportionately larger and heavier head and weak neck muscles of children render them particularly prone to head injury after trauma. The primary cause of head injury varies with age. In infants, non-accidental injury should be considered; toddlers frequently suffer falls, whereas road traffic accidents and sports related injuries are more common in older children and adolescents.
Primary Brain Injury
Occurs at the time of in initial injury, and may result in brain contusion, laceration, and haematoma formation or diffuse axonal injury. Younger children are more likely to develop subdural haematomas and diffuse cerebral oedema without a skull fracture, whereas in adolescents, skull fractures, contusions and extradural haematomas are more common.
Secondary Brain Injury
Occurs in the minutes to days after the initial injury and may be due to hypotension, raised intracranial pressure or cerebral ischaemia. Secondary brain injury is worsened by hypoxia, hypercarbia, anaemia, pyrexia, hypoglycaemia or hyperglycaemia. Secondary brain injury may be modified by simple clinical interventions, the most important of which are avoidance of hypotension and hypoxia.
Intracranial pressure
The brain is enclosed within the rigid skull. The intracranial pressure (ICP) is determined by the volume of the brain tissue, the cerebrospinal fluid (CSF) volume, and the cerebral blood volume. Increase in the volume of the intracranial contents, for instance due to cerebral oedema or an extradural, subdural or intracerebral haematoma, will result in increased intracranial pressure. Compensation is possible for small rises in ICP by increased CSF absorption and a reduction in intracranial blood volume. Infants can compensate for slow increases in intracranial pressure because of their open fontanelles and suture lines; however sudden acute changes in intracranial pressure are not well tolerated at any age. If compensatory mechanisms are overwhelmed, intracranial pressure will increase rapidly and the brain will herniate through the structures within the skull or the foramen magnum ( ‘coning’) to cause coma and death.
Cerebral perfusion pressure
The cerebral perfusion pressure (CPP) is the effective blood pressure that perfuses the brain and is defined as:
CPP = MAP – ICP
where MAP is the mean arterial pressure. The MAP and therefore CPP vary with age, as does the ICP. Table 1 shows the normal systolic BP in children, also the optimal level systolic BP to be achieved in children with traumatic brain injury, that is, >95th centile for age. Cautious fluid resuscitation and infusion of vasoconstrictors such as noradrenaline may be required.
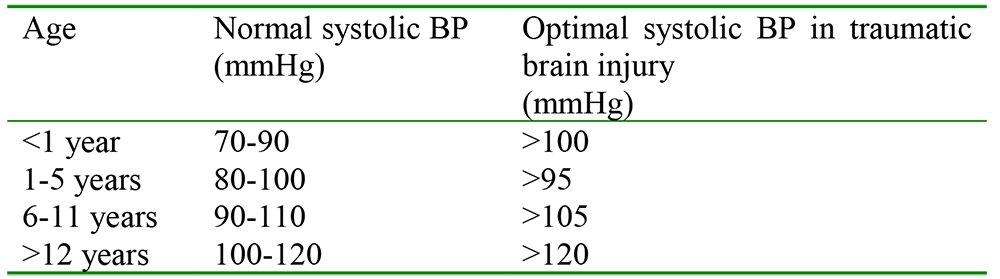
Table 1. Normal systolic blood pressure and optimal systolic blood pressurein children with traumatic brain injury.
Typical intracranial pressures are 8–18mmHg in adults and 2–10 mmHg in children. The venous pressure is low under normal circumstances and does not affect the CPP, but abnormally raised venous pressure will reduce CPP.
Cerebral blood flow
Under normal conditions, cerebral blood flow is maintained at a constant level to meet the metabolic demands of the brain over a wide range of MAP by the process of autoregulation. The autoregulation range for adults is 50-140 mmHg. The autoregulation range is not known in infants and children, but is likely to be around 40-90 mmHg.
Cerebral autoregulation is impaired by acute brain injury; in this situation, cerebral blood flow follows cerebral perfusion pressure passively. It is vital to keep the blood pressure within the ‘high normal’ range in head injured patients, as hypotension will result in cerebral ischaemia.
In the absence of invasive measurement of intracranial pressure, cerebral perfusion pressure should be maintained between 50-70 mmHg, that is, MAP 70-90 mmHg, assuming the intracranial pressure to be 20 mmHg. The MAP may be calculated from systolic/diastolic BP: MAP = DBP + (SBP-DBP/3). Cerebral perfusion pressure less than 50 mmHg has been demonstrated to be a predictor of poor outcome in severe traumatic brain injury in adults and children. Extreme hypertension will result in increased cerebral blood flow and cerebral oedema and should also be avoided.
OTHER FACTORS AFFECTING CEREBRAL BLOOD FLOW AND INTRA CRANIAL PRESSURE
Oxygen
An adequate supply of oxygen is essential to meet the metabolic requirements of the brain. In addition, hypoxia results in cerebral vasodilatation and increase in cerebral blood flow and hence intracranial pressure. Cerebral blood flow begins to rise when PaO2 falls to 6.7kPa (50mmHg), and doubles at PaO2 of 4kPa (30 mmHg). Hypoxia must be avoided at all times in patients with head injury.
Carbon dioxide retention
Is a potent cause for cerebral vasodilatation and increase in intracranial pressure. Conversely, hyperventilation resulting in hypocarbia results in cerebral vasoconstriction and at extreme levels will cause cerebral ischaemia. It is important to maintain the carbon dioxide levels within normal range as much as possible (4.5-5.5 kPa). Remember, end tidal CO2 measurements usually underestimate arterial CO2, especially if there is coexisting lung injury or disease. Modest hyperventilation may be used to reduce intracranial pressure in an emergency (but keep PaCO2 > 4KPa, and definitely not below 3.5).
Body temperature
Has an important effect on cerebral blood flow. For every 1°C increase in body temperature, there is a 5% increase in cerebral metabolic rate leading to an increase in cerebral blood flow and intracranial pressure. Pyrexia should be avoided in the head injured patient, and normothermia/moderate hypothermia is desirable. Excessive hypothermia therapy below 33°C may increase mortality.
Blood glucose
The brain is critically dependent on a normal blood supply of glucose for metabolism and only has a very small store of glucose in the form of glycogen. Children are more susceptible to hypoglycaemia as the cerebral metabolic rate is higher in children than adults (peak at 6 years). Conversely, hyperglycaemia should be avoided after head injury as it induces lactic acidosis and production of oxygen free radicals and worsens outcomes. It is important therefore to actively seek and treat hypoglycaemia and hyperglycaemia.
Seizures
Seizures increase the metabolic demands (and therefore oxygen requirements) of the brain and must be treated promptly.
Fluid and electrolyte abnormalities
Hypotonic fluids must be avoided in children with head injury as a fall in plasma sodium will exacerbate cerebral oedema. Plasma sodium and plasma osmolality must be maintained within the high normal range (aim for plasma sodium 150 mmol/l in severe head injury).
Children with traumatic brain injury are susceptible to a variety of abnormalities of plasma sodium: Inappropriate antidiuretic hormone (ADH) – hyponatraemia, low plasma osmolality, high urinary osmolality, normo/hypervolaemia, potential cerebral oedema. Treat with fluid restriction if asymptomatic or hypertonic saline if symptomatic (1-2 ml/Kg 3% saline bolus)
Cerebral salt wasting – hyponatraemia, high urinary osmolality, hypovolaemia and hypotension. Treat with normal saline bolus
Diabetes insipidus – hypernatraemia, high plasma osmolality, low urinary osmolality, hypovolaemia and hypotension
Diabetes insipidus occurs as a result of failure of blood supply to the posterior pituitary with loss of ADH production in the posterior pituitary – it should be treated by administration of DDAVP (Desmopressin), however, DI is a late sign in head injury and often heralds brain stem death.
Coagulopathy
Penetrating injury is associated with release of brain tissue into the circulation, which may result in disseminated intravascular coagulation.
Autonomic changes
Intense peripheral vasoconstriction and hypertension are often seen in severe head injury.
Neurogenic pulmonary oedema
Severe head injury may be associated with sudden onset of severe pulmonary oedema leading to hypoxia.
Analgesia and anaesthetic agents
Pain and anxiety increase metabolic demands and should be treated, avoiding excessive doses of agents that may cause respiratory depression, or alternatively, ventilating the patient electively to allow for this.
A small percentage of children with head injury may require surgery to evacuate intracranial haematoma. Volatile anaesthetic agents reduce the metabolic requirements but increase cerebral blood flow and ICP. Halothane increases ICP more than isoflurane and should be avoided if possible.
Intravenous anaesthetic agents reduce the cerebral metabolic rate, and also reduce cerebral blood flow and ICP, with the exception of ketamine, which increases ICP. Ketamine should be avoided in head injury patients if possible; thiopentone or propofol are the intravenous agents of choice, along with judicious doses of opioids to obtund the reflex cardiovascular responses to intubation.
Suxamethonium will increase ICP transiently only. Suxamethonium is indicated for rapid sequence induction in head injured patients.
ASSESSMENT OF NEUROLOGICAL DISABILITY
All children suspected of head injury should have regular neurological assessments and assessment of pupil responses.
Modified Glasgow Coma Scale for Children
Rapid neurological assessment of patients with head injury may be made using the AVPU score (Alert, responds to Verbal commands, responds to Pain, Unresponsive). The Glasgow coma scale is a more sophisticated method of assessing and describing level of consciousness and has been modified for use in children (table 2). The motor response is the most accurate predictor of poor outcome; any child with a reduction in motor score below “localizing pain” should be treated as having a severe head injury.
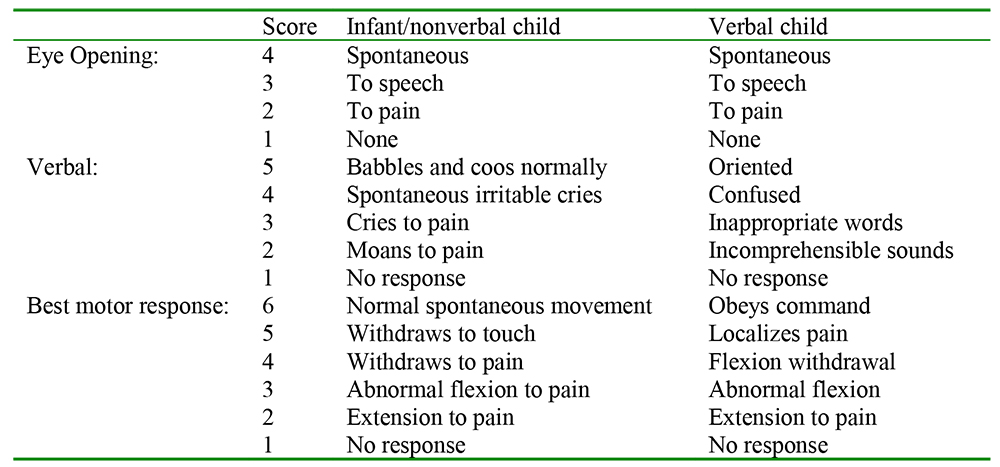
Table 2. Modified Glasgow coma score for children
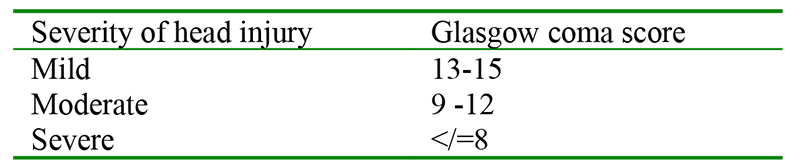
Table 3. Severity of head injury
Pupil responses
Pupil responses are an important clinical sign and should be assessed regularly in all children with head injuries.
- Normal response – pupils react symmetrically to light and accommodation
- Bilateral fixed and dilated pupils – inadequate cerebral perfusion, possibly irreversible brain injury
- Bilateral pupil constriction – early brain herniation through the foramen magnum, injury to the brainstem, side effect of opioids
- Unilateral fixed and dilated pupil – herniation of the brain through the tentorium cerebelli within the skull on the same side, optic nerve injury
- Unilateral pupil constriction – unilateral brainstem injury, Horner’s syndrome
MANAGEMENT OF CHILDREN WITH TRAUMATIC BRAIN INJURY
Children with head injury must be assessed and appropriate management started immediately. Delays, particularly in management of hypoxia and hypotension, worsen outcome.
In a child thought to have suffered a minor head injury only, the following signs are worrying and merit admission of the child to hospital for close monitoring, including regular neurological assessments:
- Patients who are not fully alert
- Persistent vomiting, severe headaches
Children with moderate to severe head injury should all be admitted for rapid assessment. The following features in the history and clinical condition indicate the possibility of a severe head injury:
- History of a fall from a height, a high-speed road traffic accident, or road traffic accident where the child is a pedestrian or a cyclist
- Loss or reduced level of consciousness
- External sign of skull fracture, including base of skull fracture (‘panda eyes’, blood or CSF in the ear, bruising of the mastoid process behind the ear)
- A Glasgow coma score of </= 8 or loss of ability to localise pain on the motor category
Immediate management of a child with moderate to severe traumatic brain injury
Assess the conscious level and pupil responses at the same time as attending to ‘ABC’ as follows:
- Airway with cervical spine immobilisation
- Breathing and ventilatory control
- Circulation and control of obvious external bleeding
- Disability and neurological status, including pupil responses
- Exposure – secondary survey with top to toe examination to detect associate injuries (consider non-accidental injury)
The first priority is stabilisation of the airway and the cervical spine. Airway patency should be established, taking care of the cervical spine (jaw thrust +/- airway adjuncts), and high flow oxygen should be administered. Cervical spine injuries are uncommon and only occur in about 1% of severe head trauma patients. However, children should have cervical spine immobilisation if there is a suspicion of cervical spine injury, for instance a significant mechanism of injury, a history of loss of consciousness, neck pain or tenderness, another severe (“distracting”) injury or a history of intoxication. A child who is restless and disoriented should not be forced to wear a rigid cervical collar or forcibly restrained as this may increase fighting, anxiety and intracranial pressure.
Breathing
Should be assessed by clinical examination of respiratory pattern and rate, chest auscultation and oxygen saturation. A Chest X-ray should be obtained as part of the initial essential imaging. Arterial blood gas analysis should be obtained if possible.
The child will require intubation and ventilation in the ICU in the following situations:
- Reduced level of consciousness with a Glasgow coma score ≤8
- Inadequate breathing (saturation persistently <95% in oxygen), hyperventilation or hypoventilation (PaO2 <9kPa in air/<13kPa in oxygen or PaCO2 <3.5/>6kPa)
- Loss of protective laryngeal reflexes
- Significant facial or neck injuries
- Seizures
An intubated child with a head injury in the ICU will require sedation and analgesia; midazolam and morphine are the usual drugs of choice. A muscle relaxant may be required if it is difficult to control the ventilation. The child should be ventilated to obtain a normal PaCO2. An appropriately trained nurse or anaesthetist should always be present with the child.
Circulation
Hypotension must be actively sought and treated. Venous access should be established early and blood samples taken for full blood count, electrolytes and group and save. Two cannulae should be inserted, and intraosseous access or venous cutdown should be considered if venous access is difficult.
A useful formula for expected blood pressure in children is:
- Expected systolic BP (mmHg) = 80 + (age in years x 2).
As discussed above, a higher than normal blood pressure should be maintained to ensure adequate cerebral perfusion.
Normal saline or Ringers are the fluid of choice for initial resuscitation. An initial fluid bolus of 10 ml/kg should be given, followed by another 10 ml/kg if the child remains hypotensive. Overhydration must be avoided, as this will promote cerebral oedema formation. If the haemoglobin is less than 7g/dl then extracranial causes of blood loss should be considered (or chronic anaemia). The child may require blood transfusion. Of note however, an intracranial bleed in a neonate may cause hypovolaemia and a fall in haemoglobin (before signs of raised ICP become apparent).
Disability and exposure:
Assess the GCS and pupil responses. Other injuries should be sought and treated. Scalp lacerations may result in significant blood loss. If the child remains cardiovascularly unstable and requiring volume resuscitation, consider other sites of blood loss: chest, abdomen, pelvis or major limb fracture.
Indications for CT scanning
A CT scan is the gold standard imaging in assessing patients with head injury, if available. The CT scan will pinpoint a surgically remedial lesion such as subdural or extradural haematoma, and give an indication of severity of brain injury (presence of cerebral oedema, contusions, intracerebral bleeds etc). However, this is an expensive facility and may not always be available at the receiving hospital. The indications for CT scanning are as follows:
- A clinical suspicion of severe head injury, such as reduced conscious level, amnesia, abnormal drowsiness
- Skull fracture, either basal or open or depressed skull fracture
- Seizures, other neurological deficits or persistent vomiting
- A dangerous mechanism of injury
- Suspicion of non-accidental injury
As cervical spine X-rays are rarely adequate in children wearing cervical collars, a CT of the head should be extended to include the neck too.
Indications for referral for surgery
10 – 20% of patients with severe traumatic brain injury have a surgically treatable condition such as extradural haematoma requiring burr hole; neurosurgical intervention may be life saving in this situation. A surgical opinion should be sought if the CT scan shows an intracranial haematoma or there is clinical suspicion of an intracranial haematoma, such as progressive focal neurological signs. A surgical opinion should also be sought in the case of depressed skull fracture, CSF leak or penetrating injury. Tertiary neurosurgical centres are able to offer interventions to manage severe raised intracranial pressure (see below).
Intensive care management:
The primary goal of intensive care management in severe traumatic brain injury is prevention of secondary brain injury by maintaining adequate cerebral perfusion and oxygenation and controlling raised intracranial pressure. Children with severe traumatic brain injury should be transferred to an intensive care unit if at all possible. Secondary and tertiary centres will be able to undertake advanced techniques such as invasive blood pressure monitoring, use of inotropes and intracranial pressure monitoring, as well as CSF drainage or decompressive craniotomy for patients who deteriorate due to diffuse cerebral oedema. Such treatments are expensive and will not be possible in most resource poor environments. General supportive measures should be possible in all intensive care units.
General intensive care management
All patients with head injury should have simple measures instituted as follows:
- Nurse the child in 30° head up position with neutral head positioning
- Maintain SpO2 >95%
- Maintain CO25-5.0 kPa
- Maintain blood pressure in the high/normal range
- Avoid excessive fluid loads
- Avoid hypotonic fluids containing dextrose. Aim for plasma sodium 145-150 mmol/l
- Use inotropes if necessary to maintain blood pressure (noradrenaline)
- Provide adequate sedation and analgesia
- Maintain blood sugar in normal range
- Maintain normal temperature, treat pyrexia aggressively
- Control seizures
- Provide adequate nutrition via a nasogastric tube (start early).
Special treatment for raised intracranial pressure, tertiary centres:
- Institute intracranial pressure monitoring using a bolt or extradural or intraventricular catheter if possible. Rising intracranial pressure should be managed aggressively, particularly ICP>20mmHg
- CSF drainage via intraventricular drain
- Mild hyperventilation to PaCO2 < 4.5 kPa
- Consider osmotic therapies to reduce intracranial pressure such as mannitol or 3% hypertonic saline
- Consider barbiturate-induced coma with refractory intracranial pressure elevation if the child is cardiovascularly stable.
- Profound hyperventilation to PaCO2 < 3.9 kPa may be used temporarily pre-craniotomy
- Decompressive craniectomy may be considered in children with diffuse cerebral oedema, within 48 hours of injury, with no sustained episodes of intracranial pressure >40mmHg and secondary clinical deterioration with evolving cerebral herniation
Conclusion
Immediate airway management (with cervical spine control) and cardiopulmonary resuscitation are the most important early steps in management of traumatic brain injury in children. The importance of avoiding hypotension and hypoxia and of detection and rapid treatment of surgically remediable lesions cannot be over emphasised. Children are best managed in experienced paediatric trauma centres if at all possible. This may require transfer to another centre over long distances. Excellent communication and multidisciplinary approach is essential to produce the best outcomes.
References and further reading:
- Hatch and Sumner. Trauma and transport Textbook of Paediatric Anaesthesia (3rd Edition): 635-645,
- Hatch and Sumner. The central nervous system Textbook of Paediatric Anaesthesia (3rd Edition): 95-108,
- CATS clinical guidelines on Traumatic Brain Injury http://www.cats.nhs.uk/PDF/CATS_TBI.pdf
- Triage, assessment, investigation and early management of head injury in infants, children and adults http://www.nice.org.uk/CG056
- Orliaguet, Meyer and Baugnon. Management of critically ill children with traumatic brain injury, Paediatric Anaesthesia 2008;(18):455-461
- Giza, Mink and Madikians. Pediatric traumatic brain injury: not just little adults. Current Opinions in Critical Care 2007;(13):143-152
- Lam and Mackersie. Paediatric head injury: incidence, aetiology and management. Paediatric Anaesthesia 1999; (9): 377-385
- F.J.M.Walters. Intra cranial pressure and cerebral blood flow: Update in Anaesthesia, www.worldanaesthesia.org
Answers to MCQs
-
- F
- T
- T
- F
- T
-
- T
- F
- F
- F
- F
-
- T
- F
- F
- T
- F
-
- T
- F
- T
- F
- T
-
- T
- T
- T
- T
- T
-
- T
- T
- T
- T
- F
-
- T
- T
- F
- T
- T



