Pain
KEY POINTS
- Postamputation pain syndromes, including phantom limb pain (PLP), are common in the postamputation patient and
are a significant public health burden. - The pathophysiology of PLP is thought to occur via peripheral, spinal cord, and cerebral mechanisms.
- Predisposing factors for PLP include severe preoperative pain, anxiety and depression, and hereditable factors.
- Clear evidence for definitive treatment and prevention remains lacking, with small sample sizes and heterogeneity limiting the validity of available data.
- It is recommended that management of these patients is commenced prior to the amputation, with multidisciplinary
care including patient education and optimisation of preoperative analgesia and psychological state. - We suggest a multimodal analgesic strategy encompassing the pre-, intra- and postoperative phases, incorporating
preemptive regional anaesthesia and the use of N-methyl D-aspartate–antagonist infusions.
INTRODUCTION
The phenomenon of phantom limb pain (PLP) was first described by Ambroise Paré, a French military surgeon in the 16th century.1 PLP has since remained somewhat enigmatic, lacking a clearly understood pathophysiological mechanism. With ongoing military conflicts and the increasing incidence of peripheral vascular disease, pain syndromes following limb amputations continue to challenge the medical community.
Classifications
Pain syndromes associated with limb amputations can be classified phenomenologically.
Acute stump pain refers to the immediate nociceptive pain response localised to the site of the amputation and is a direct manifestation of the extensive tissue trauma involved in the formation of the stump.
Persistent stump pain refers to nociceptive and/or neuropathic pain persisting in the operative stump for longer than 2 to 3 months postoperatively.2 While most patients experience resolution of their stump pain in the initial months following their operation, a small minority continue to be plagued by prolonged pain perceived as arising from the stump. The causative factor for a prolonged experience of pain is variable within this patient cohort, with aetiologies such as bone spurs, heterotrophic ossification, arterial insufficiency and neuromas all being potential suspects. More sinister pathologies such as osteomyelitis, superficial tissue infection and haematomas should be considered and treated on their merits. Importantly, a well-seated prosthesis plays a vital role in stump care and comfort.
Phantom sensation refers to any nonpainful sensory experience perceived to be originating from the absent limb. This is a common and almost universal experience in the early postoperative phase.
Phantom limb pain describes the perception of a noxious stimulus from the missing body part and is commonly distressing for the patient. Up to 78.8% of postamputation patients will experience PLP, with up to 92% of these patients experiencing the onset of this pain within the first week postoperatively.3 Patients may describe PLP as an intermittent, burning, electric-type pain that typically lasts minutes to hours. A small minority of patients, predominantly those with ischaemic vascular disease, experience constant, unremitting PLP.
PATHOPHYSIOLOGY
Figure 1 summarizes the pathogenesis of phantom limb pain.
Peripheral Mechanism
Amputation of a peripheral limb involves significant trauma to the surrounding soft tissue. This trauma results in inflammation and disrupts the normal neurological pathways, with resultant deafferentation. Both inflammation and deafferentation encourage the proximal portion of damaged A-delta and C-fibre nerve segments to sprout neuromas. Such neuromas possess reduced activation thresholds and a relative increased density of sodium channels, increasing the incidence of ectopic neural potentials and resulting in spontaneous discharges. Depending on the positioning of the neuroma, this may manifest in chronic stump pain or, if more proximal, may be experienced as phantom limb sensation or PLP.
Spinal Cord Mechanism
The most studied theory for spinal cord–derived PLP is that of central sensitisation. This process occurs when postamputation inflammation triggers neurons not responsible for the transmission of nociceptive signals to grow into lamina II of the dorsal horn. This generates an increased neuronal receptive field, which results in a relative increase in N-methyl D-aspartate (NMDA) receptor activity at the dorsal horn, with consequent increased susceptibilities to activation by noxious stimuli such as substance P, tachykinins and neurokinins in a process known as the ‘wind-up’ phenomenon.4 The culmination of this process is regional hypersensitisation of the neuronal field representing the region of the amputated limb. Concurrent restructuring of the descending inhibitory pathways via reductions in intersegmental inhibition at the spinal cord level results in spinal disinhibition, allowing additional nociceptive inputs to reach supraspinal centres.
Brain Mechanism
There are two described mechanisms for the role of the brain in the generation of PLP: cortical reorganisation and disturbance of the neuromatrix and neurosignature (Figure 1).
Cortical reorganisation refers to the neuroplasticity response to amputation, whereby areas of the cortex that represent the amputated region are taken over by neighbouring regions in both the primary somatosensory cortex and the primary motor cortex.4 This mechanism partly explains why stimulation of nerves in the surrounding area to the amputation site may result in
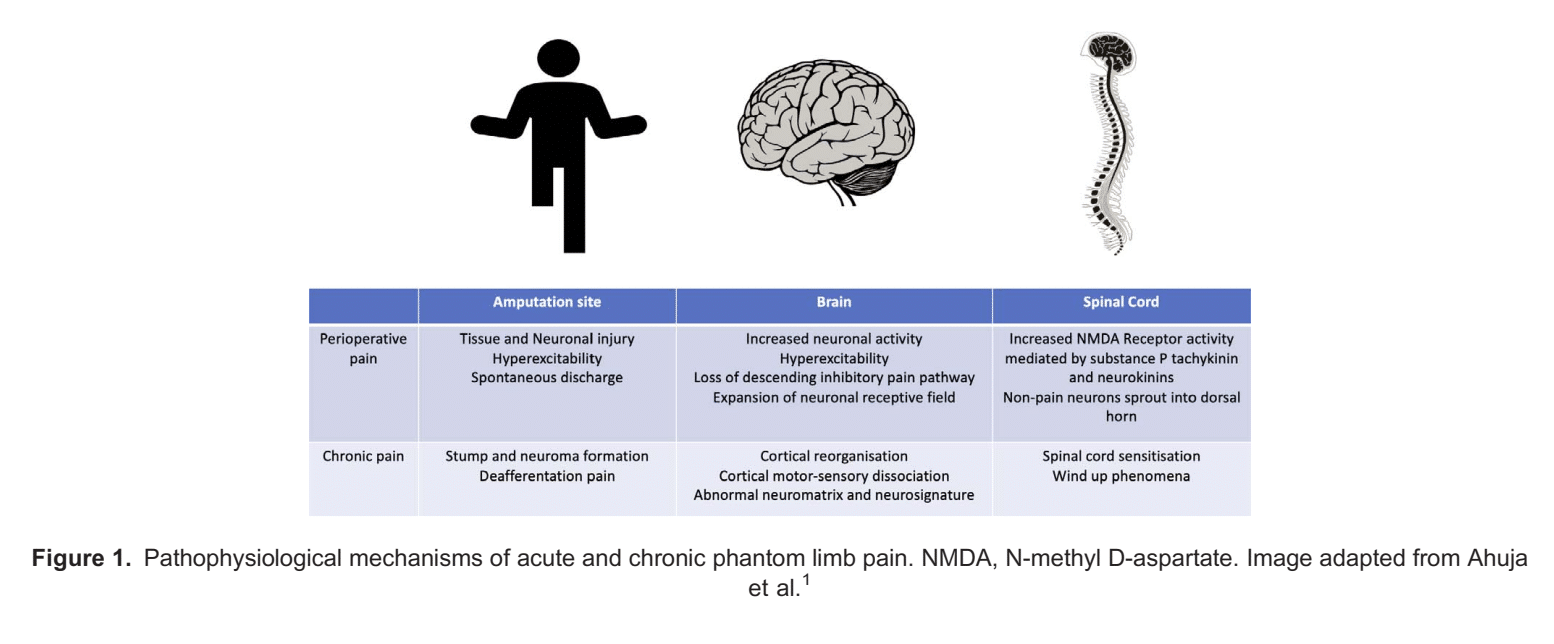
phantom sensation. More recent neuroimaging studies have demonstrated that the degree of this cortical reorganisation correlates with the severity of phantom limb sensation experienced by patients.4
The neuromatrix and its corresponding neurosignature constitute a hypothesis first driven by Ronald Melzack in 1989.4 The neuromatrix hypothesis purports that a network of neurons within the brain exists that integrate inputs from somatosensory, limbic, visual and thalamocortical components to generate a central cortical representation of the self.4 The neurosignature is thought to be the patterns of activity generated by the brain based on one’s conscious awareness and perception of the body itself. It is thought that amputation represents a deprivation of inputs into the neuromatrix, which distorts the neurosignature, resulting in a cortical error that generates phantom sensation.4
Predisposing Risk Factors
Recent reviews of the literature surrounding both PLP and chronic non-PLP support the assertion that the presence of preoperative pain, regardless of its anatomical relationship to the surgical site, significantly increases the risk of developing postoperative chronic pain.1 Furthermore, PLP is more likely to be experienced in those receiving upper-limb amputations or bilateral amputations, with female patients more frequently affected than male patients.1 Recent genetic analysis has also suggested that there is a genetic predisposition to chronic pain, with a heritability range between 30% and 70%.2 Genetic mapping has demonstrated that this heritability relates to the presence of GCH1 and KCNS1 genes, which increase the vulnerability of a patient to acute and chronic pain syndromes. Finally, it has long been understood that anxiety and depression in the perioperative period affect the development of PLP and chronic stump pain.2
MANAGEMENT
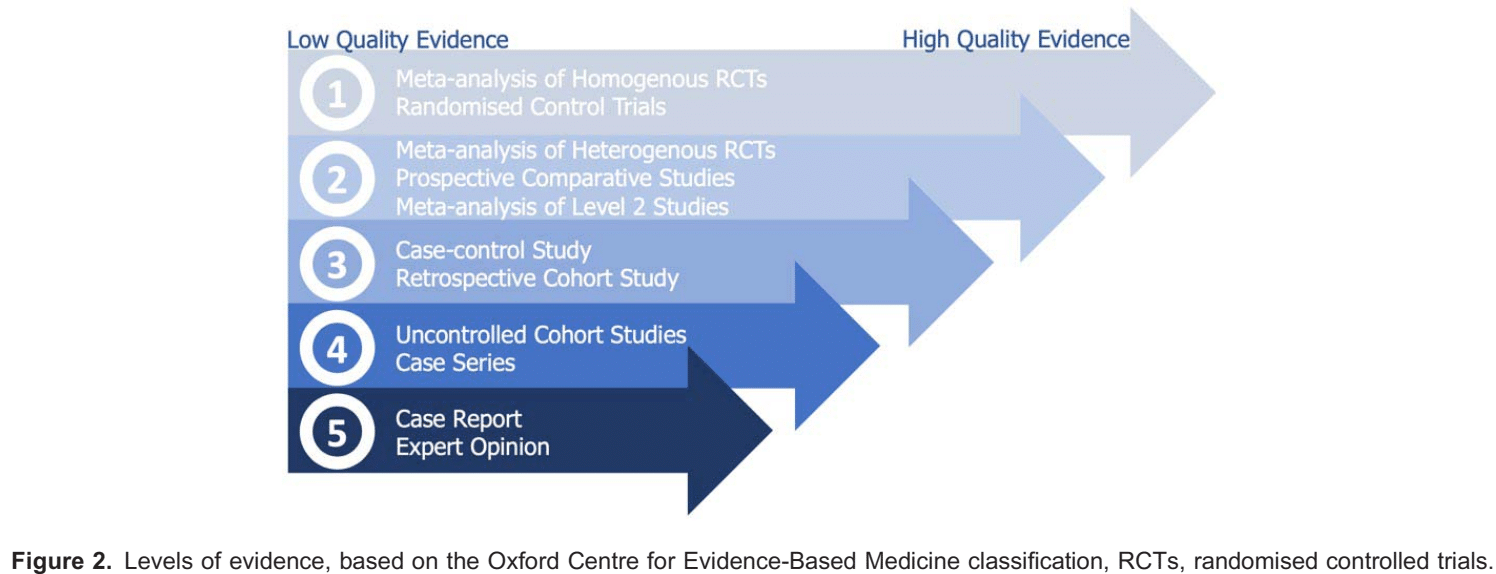
For the most part, evidence regarding treatment and prevention strategies for PLP and chronic stump pain remains frustratingly mixed, with heterogeneity and small sample sizes limiting the quality of data. As a result, a balanced multimodal approach appears sensible. See Figure 2 for definitions of levels of evidence used in this document.
Simple Analgesia
Where tolerated and clinically appropriate, regular simple analgesics including paracetamol (acetaminophen) and nonsteroidal anti-inflammatories (NSAIDs) should be incorporated into the analgesic regimen for postamputation pain, as per the World Health Organisation analgesic ladder. They benefit patients in the acute pain response; however, there is no evidence of impact on the incidence or severity of chronic stump pain or PLP.
Opioid Analgesia
With acute stump pain being readily identifiable and primarily nociceptive in nature, opioid analgesia has long been a mainstay of pharmacologic therapy. In keeping with this, there is level 1 evidence supporting the use of systemic patient-controlled opioid analgesia (PCA) for the management of acute stump pain in the immediate postoperative period.1 There is no robust evidence demonstrating the superiority of one opioid over another. In the setting of preventing PLP, opioid analgesia plays an adjuvant role, with level 2 evidence for opioid PCA use decreasing the severity and incidence of PLP at 6 and 12 months postoperatively when started 48 hours preoperatively and continued up to 48 hours postoperatively.1
Chronic stump pain is similarly largely nociceptive in nature; hence, treatment regimens have traditionally centred on simple analgesia with long-acting oral opioid analgesia. Opioids are potentially effective in this setting through their action both at the spinal cord level for local analgesia and likely more importantly at the supraspinal level, where oral opioids are thought to diminish the degree of cortical reorganisation associated with pain intensity.5 Tramadol has been found to be particularly effective in the setting of chronic nociceptive pain compared with its utility in the acute phase.6 Tapentadol, another atypical opioid, still requires further research into its utility in postamputation pain syndromes.
It must be noted that the potential for addiction and adverse effects (including hyperalgesia) with opioids are well documented, and hence, their need should be reviewed regularly and dose reductions initiated as soon as clinically appropriate.
NMDA Receptor Antagonists
The NMDA receptor antagonists ketamine and dextromethorphan have demonstrated clinical utility in the management of acute postamputation pain. Level 2 evidence supports the addition of adjuvant systemic basal infusions of NMDA receptor antagonists (eg, ketamine intravenously 0.1-0.2 mg/kg/h) in the setting in which analgesia is not appropriately achieved with opioid monotherapy and to limit the burden of opioid-induced side effects.1
Ketamine and dextromethorphan have been demonstrated to be beneficial in the short-term perioperative treatment of PLP7; however, there is conflicting and insufficient literature to support its use specifically for long-term prevention of PLP.
Recently published consensus guidelines following a meta-analysis of available data in 2018 demonstrated that there was weak or no evidence for the role of intravenous ketamine in the treatment of chronic PLP and chronic stump pain.8
Regional Anaesthesia
Recent research has demonstrated level 1 evidence supporting the use of either epidural or perineural catheters for reducing acute postoperative pain, particularly when continued >72 hours postoperatively.1 Level 1 evidence demonstrates an opioid sparing benefit with the use of epidural analgesic techniques.1 There is level 2 evidence supporting the role of epidural analgesia as part of a multimodal analgesic regimen in reducing both the incidence and severity of PLP at 12 months postoperatively when initiated at least 24 hours preoperatively and continued for at least 48 hours postoperatively.2
With regard to peripheral nerve block catheters, there is level 1 evidence supporting their use for acute postoperative pain and opioid sparing.9 There does exist some data to support the use of peripheral nerve blocks for the prevention of PLP, with some studies producing encouraging results. As an example, in an observational study, Borghi et al10 demonstrated an incidence of severe PLP of only 3% at 12 months in postamputation patients following the use of 0.5% ropivacaine continuous infusion vi perineural nerve catheters, which remained in situ for a median duration of 30 days (minimum to maximum range of 4-83 days), a significant improvement from the baseline reported incidence of 25-78.8% in an untreated population. In that study, lumbar plexus blockade was used for hip amputations, with more distal leg amputations receiving sciatic nerve catheters with or without femoral nerve catheters. Further large scale, well-powered randomised controlled trials are required to further clarify the utility of perineural nerve catheters in the prevention of PLP.
Calcitonin
Calcitonin is frequently cited in the literature surrounding postamputation analgesia; however, its mechanism of action remains unclear. Azria11 postulated that calcitonin acts primarily via the direct inhibition of neurons in the central serotonergic pathways firing in response to peripheral stimulation (and hence, serotonin receptor antagonists such as ondansetron may in theory reduce its effectiveness). The central mechanism is supported by calcitonin’s theoretical actions on B-endorphin production and peripheral inhibition of cytokine and prostaglandin production. Although its analgesic efficacy has been noted in spinal cord injury, there has been mixed level 2 evidence for its efficacy in treating PLP, with some studies suggesting a positive effect on pain levels acutely.8 In the literature, calcitonin has been given via many different administration routes, and the recommended dosing regimen is typically 200 international units once daily via the subcutaneous route. The intravenous route tends to be associated with the adverse effects of nausea and vomiting. Rarely, severe hypersensitivity reactions to calcitonin can occur. Other than level 2 evidence regarding the use of calcitonin in epidural catheters,1 there does not appear to be any significant evidence supporting its use for the prevention of PLP.
Gabapentinoids
Although studies specifically evaluating the role of gabapentinoids in acute stump pain are limited, there is evidence for their use in reducing opioid burden and acute pain generally,1 permitting cautious extrapolation for their use in a multimodal regimen in acute postamputation pain. Care must of course be exercised regarding adverse effects such as sedation. There exists level 2 evidence demonstrating that early postoperative use of gabapentinoids does not reduce the incidence of chronic stump pain or PLP.1 In contrast, there is level 2 evidence supporting their use for treating established PLP in terms of severity of pain but not functionality.1
Depending on age and comorbidities, typical dosing regimens include gabapentin 100 mg twice to 3 times daily, uptitrated to a maximum of 1200 mg 3 times daily dose as required or pregabalin 25-75 mg once daily uptitrated to 300 mg twice a day.
Lidocaine (Lignocaine)
Although there is some limited evidence supporting the use of intravenous lidocaine infusions for decreasing the severity of stump pain,7 overall there is not a truly convincing body of evidence supporting its use in the setting of postamputation pain. There is also some clinical experience to support the use of topical lidocaine for localised neuropathic pain in some patients, but good-quality supporting evidence in the postamputation literature is currently lacking.
Antidepressants
Tricyclic antidepressants are widely used in the treatment of neuropathic pain yet have no convincing evidence of efficacy in acute postamputation pain nor PLP.4 Their unrefined mechanism of action often results in drug interactions and undesired side effects, resulting in their use being contraindicated. Therefore, they are currently not advised for use in the management of postamputation pain in itself. Duloxetine has been demonstrated to be effective in neuropathic pain associated with diabetes mellitus, but there is no body of evidence to support its use specifically in postamputation pain.2
Nonpharmacological Therapies
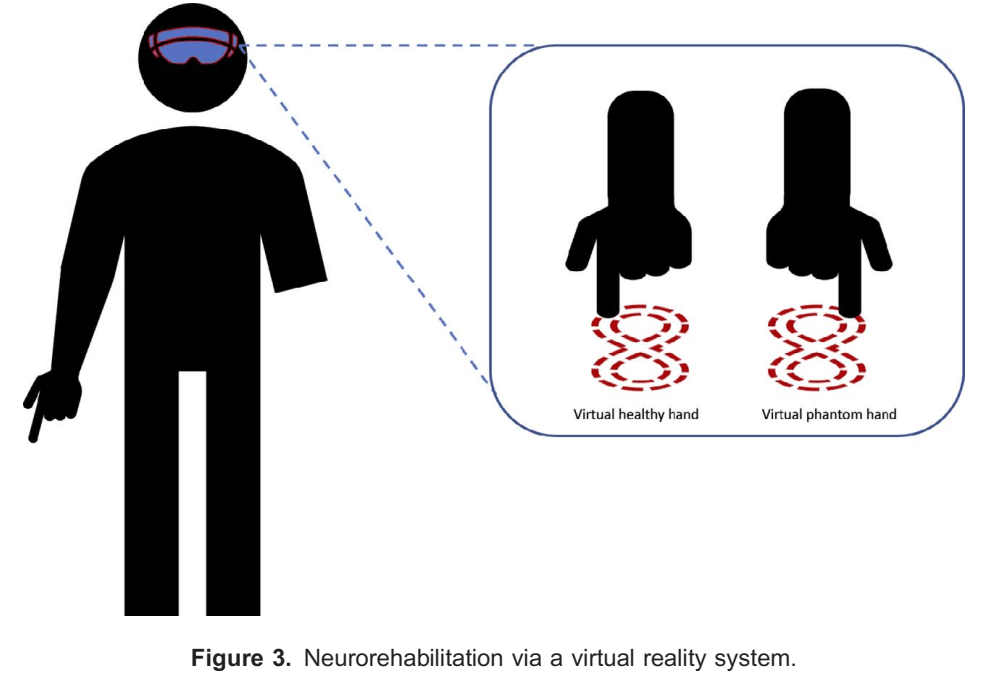
Graded motor imagery is a treatment regimen that incorporates the sequential training activities of laterality training, explicit motor imagery, followed by mirror therapy. There is now evidence that this is effective in reducing PLP severity, and given its low setup costs and lack of potential for adverse effects, this is likely to be a useful adjunctive therapy in patients with PLP.12 Virtual reality technology (Figure 3) is also a newer treatment modality that has a growing evidence base for reducing PLP severity, and further research is eagerly anticipated.13
Novel Interventions
The use of botulinum toxin A for chemodenervation of distal nerve segments has shown encouraging results in limited small trials, with statistically significant reductions in chronic stump pain at 1 month and up until 6 months.14 Similarly, small trials investigating pulsed radiofrequency ablation of neuromas have demonstrated a marked reduction in chronic neuropathic pain at up to 6 months post treatment in patients with symptomatic neuromas.7 The viability and clinical efficacy of these treatments need to be formally investigated with larger scale robust studies.
Where to Next?
Chessell et al15 suggested that monoclonal antibody–based therapeutics hold promise for the next frontier of analgesic drugs. Tumor necrosis factor alfa inhibitors and anti–nerve growth factor antibodies are currently in development, with phase 1 trials demonstrating efficacy in the treatment of chronic pain in patients with osteoarthritis and chronic lower back pain. It is hoped
that such antibody-based therapies will provide more effective alternatives to current analgesic modalities with a smaller side effect burden.7
SUGGESTED MANAGEMENT APPROACH
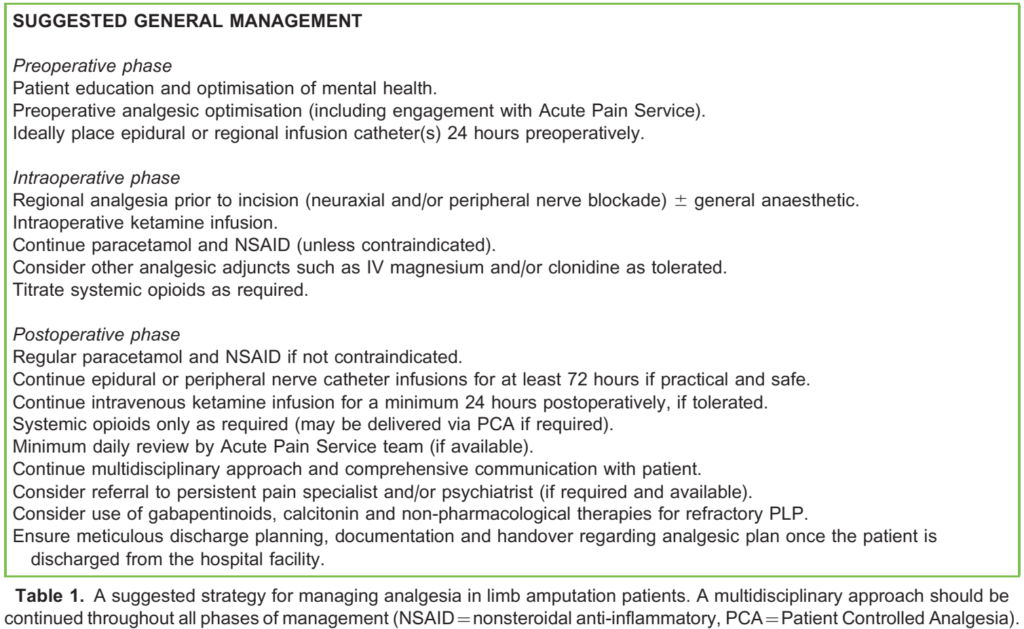
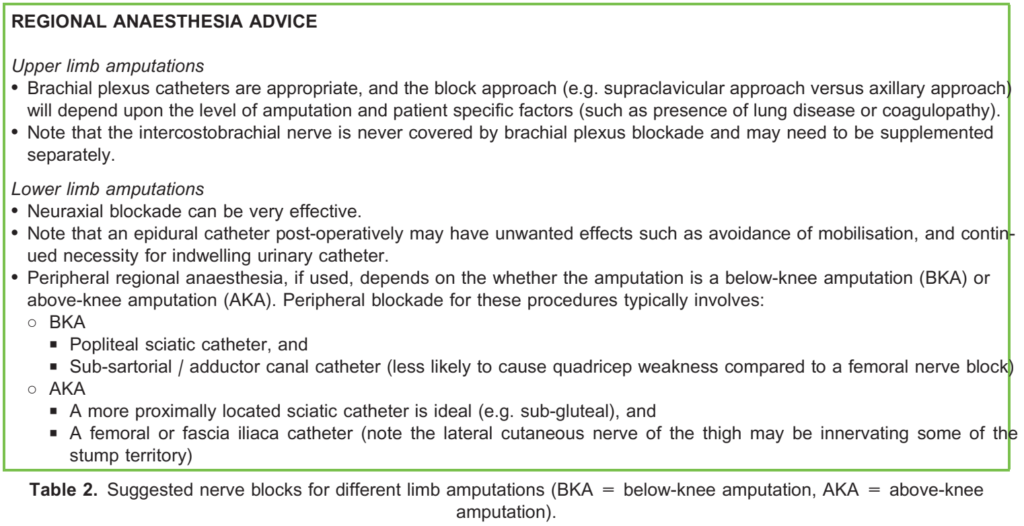
The authors’ suggested management approaches are outlined in Table 1 and Table 2.
SUMMARY
Managing post–limb amputation pain syndromes can be challenging and frustrating for both patients and physicians. Despite causing a significant public health burden, clear evidence for optimal management of these complex pain syndromes remains scarce. On the weight of the available evidence, we recommend a multimodal analgesic approach incorporating preemptive regional anaesthesia techniques, as well as attendance to nonpharmacologic interventions and risk factor management. There remains a need for large-scale randomized controlled trials with long-term follow-up, using prevention of PLP as the primary outcome.
REFERENCES
1. Ahuja V, Thapa D, Ghai B. Strategies for prevention of lower limb post-amputation pain: a clinical narrative review. J Anaesthesiol Clin Pharmacol. 2018;34(4):439-449.
2. Srivastava D. Chronic post-amputation pain: peri-operative management—review. Br J Pain. 2017;11(4):192-202
3. Richardson C, Glenn S, Nurmikko T, Horgan M. Incidence of phantom phenomena including phantom limb pain 6 months after major lower limb amputation in patients with peripheral vascular disease. Clin J Pain. 2006;22(4):353-358.
4. Subedi B, Grossberg GT. Phantom limb pain: mechanisms and treatment approaches. Pain Res Treat. 2011;2011:864605. doi:10.1155/2011/864605
5. Huse E, Larbig W, Flor H, Birbaumer N. The effect of opioids on phantom limb pain and cortical reorganization. Pain. 2001;90(1-2):47-55.
6. Wilder-Smith CH, Hill LT, Laurent S. Postamputation pain and sensory changes in treatment-naive patients: characteristics and responses to treatment with tramadol, amitriptyline, and placebo. Anesthesiology. 2005;103(3):619-628.
7. Hsu E, Cohen SP. Postamputation pain: epidemiology, mechanisms, and treatment. J Pain Res. 2013;6:121-136.
8. Cohen SP, Bhatia A, Buvanendran A, et al. Consensus guidelines on the use of intravenous ketamine infusions for chronic pain from the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists. Reg Anesth Pain Med. 2018;43(5):521-546.
9. Bosanquet DC, Glasbey JC, Stimpson A, Williams IM, Twine CP. Systematic review and meta-analysis of the efficacy of perineural local anaesthetic catheters after major lower limb amputation. Eur J Vasc Endovasc Surg. 2015;50(2):241-249.
10. Borghi B, D’Addabbo M, White P, et al. The use of prolonged peripheral neural blockade after lower extremity amputation. Anesth Analg. 2010;111(5):1308-1315
11. Azria M. Possible mechanisms of the analgesic action of calcitonin. Bone. 2002;30(5 suppl):80S-83S.
12. Limakatso K, Madden V, Manie S, et al. The effectiveness of graded motor imagery for reducing phantom limb pain in amputees: a randomised controlled trial. Physiother J. 2020;109:65-74.
13. Rutledge T, Velex D, Depp C, et al. A virtual reality intervention for the treatment of phantom limb pain: development and feasibility results. Pain Med. 2019;20(10):2051-2059.
14. Wu H, Sultana R, Taylor KB, Szabo A. A prospective randomized double-blinded pilot study to examine the effect of botulinum toxin type A injection versus lidocaine/depomedrol injection on residual and phantom limb pain: initial report. Clin J Pain. 2012;28(2):108-112.
15. Chessell IP, Dudley A, Billinton A. Biologics: the next generation of analgesic drugs? Drug Discov Today. 2012;17(15- 16):875-879.



