Intensive Care Medicine
MCQ
- Clostridium tetani
a. is a Gram-positive coccus
b. is commonly found in soil
c. may be found in human faeces
d. secretes harmful endotoxins
e. spores are destroyed by boiling for 1 hour - Regarding the clinical features of tetanus,
a. incubation period describes time from injury to first spasm
b. incubation period may be as long as 30 days
c. onset time describes time from first symptom to first spasm
d. autonomic dysfunction is common
e. laryngospasm may occur - In tetanus,
a. involvement of the cranial nerves has a better prognosis
b. neonatal disease commonly arises from the umbilicus
c. neonatal tetanus is preventable by maternal vaccination
d. neonatal tetanus carries a lower mortality
e. catecholamine levels are often elevated - Differential diagnoses may include
a. drug reaction
b. hypocalcaemia
c. strychnine poisoning
d. sepsis
e. encephalitis - Regarding the management of tetanus,
a. muscle relaxants form the main treatment
b. tetanus immunoglogulin is recommended
c. oral metronidazole is the antibiotic of choice
d. infection leads to immunity
e. surgical debridement can be delayed for 12 hours to allow resuscitation
The answers can be found at end of article.
CASE REPORT
A 52-year-old woman was admitted to the surgical ward, having been assaulted three days previously. She had suffered a head injury and her conscious level had gradually reduced over the 24 hours prior to admission. Her Glasgow coma score on admission was 12/15 and she had an open wound on her scalp, which smelt offensive. She was admitted to the surgical ward but the consultant was called when she began to have seizures 6 hours after admission. On closer observation of the patient the consultant recognized these ‘seizures’ to be severe spasms of her back muscles. Her jaw was clenched closed, her neck was stiff, her GCS had fallen to 10/15 and she had a temperature of 38.7°C. Tetanus complicating severe head injury and scalp wound infection was diagnosed. The differential diagnosis of meningitis was excluded by microbiological CSF examination.
She was transferred to theatre for urgent debridement of the wound and managed on the Intensive Care Unit postoperatively. Tetanus immunoglobulin was not available from pharmacy and she was treatment with intravenous penicillin, flucloxacillin and metronidazole. She returned from theatre ventilated and was sedated with intermittent intravenous doses of 10mg diazepam and 50mg pethidine. The spasms were partially controlled on this regimen, but addition of nasogastric phenobarbitone achieved complete suppression of the spasms by the second postoperative day. She required ventilation for 11 days, having a tracheostomy inserted on the seventh day of her admission and required two further trips to theatre for debridement of the scalp wound. She was discharged to the ward on day 23, with the tracheostomy removed. She had a residual mild hemiparesis, but otherwise made a good recovery.
INTRODUCTION
Tetanus causes approximately 1 million deaths worldwide and remains endemic in the developing world. Approximately half of these deaths are in neonates and most occur in Africa and Asia. Immunization has dramatically reduced the number of cases in developed countries, with 12-15 cases per year reported in the UK (0.2 per million population).
Tetanus is caused by a gram-positive bacillus, Clostridium tetani, which is commonly found in soil, but may also be isolated from animal or human faeces. It is a motile, spore forming, obligate anaerobe. Spores are not destroyed by boiling but are eliminated by autoclaving at 120°C for 15 minutes 1 (at one atmosphere pressure). Tetanus is usually diagnosed clinically as the bacterium is rarely cultured.
PATHOPHYSIOLOGY
Under the anaerobic conditions found in infected or necrotic tissue, the bacillus secretes two toxins: tetanospasmin and tetanolysin.
- Tetanolysin damages the surrounding viable tissue and optimizes conditions for bacterial multiplication.
- Tetanospasmin causes the clinical syndrome of tetanus, by entering peripheral nerves and traveling via axonal retrograde transport to the central nervous system. Tetanospasmin disables release of neurotransmitter from presynaptic vesicles (particularly the inhibitory neurotransmitters GABA and glycine). The result is disinhibition of motor and autonomic neurons, causing rigidity, muscle spasms and autonomic dysfunction. A relative deficiency of synaptic acetylcholine (similar to that caused botulinum toxin) causes flaccid paralysis that is clinically mild in humans.
High toxin load results in diffusion of toxin via the blood to nerves throughout the body.
CLINICAL FEATURES
Tetanus usually follows a recognized injury, which may be trivial or occur indoors. Other routes of entry include burns, ulcers, gangrene, snakebites, septic abortion, childbirth, intramuscular/intravenous injections and surgery.
The incubation period (time from first injury to first symptom) averages 7-10 days (range 1-60 days), whilst the clinical onset time (time from first symptom to first spasm) varies between 1-7 days. Shorter incubation and onset times are associated with more severe disease. Muscle spasms and rigidity are predominant in the first week and reduce after 2- 3 weeks. Autonomic disturbance usually starts several days after spasms, and persists for 1-2 weeks. Recovery from the illness occurs due to re-growth of axon terminals.
The clinical triad consists of muscle rigidity, spasms and autonomic dysfunction. Early symptoms are neck stiffness, sore throat and poor mouth opening. Increased muscle tone may affect agonist and antagonist muscle groups together, resembling a convulsion. Spasms may be spontaneous or triggered by visual, auditory or emotional stimuli and can be severe enough to cause fractures or avulse tendons. Pharyngeal and laryngeal spasms may lead to aspiration or airway obstruction. Continual spasms may lead to respiratory failure.
The most common form of tetanus (80 %) is generalized tetanus, with muscles throughout the body affected. Muscles of the head and neck are usually affected first, giving rise to masseter spasm (trismus or ‘lockjaw’) and a typical facial expression (risus sardonicus). Neck stiffness and dysphagia are also common. Truncal rigidity with predominant extensor spasm may lead severe arching of the back during spasm, called opisthotonus.
Poor cough, inability to swallow, gastric stasis all increase the risk of aspiration. Respiratory failure continues to be a major cause of mortality in developing countries, whereas severe autonomic dysfunction causes most deaths in the developed world.
Autonomic dysfunction results from paroxysmal increases in sympathetic activity, with basal catecholamine levels rising ten-fold. This results in tachycardia, hypertension and pyrexia, with a hyperkinetic circulation, low/normal systemic vascular resistance and normal right and left sided cardiac filling pressures.
Other features include excessive salivation and sweating (may lead to dehydration), cardiomyopathy and myocardial infarction. Gastric stasis, ileus, diarrhea and high output renal failure may also be related to the autonomic disturbance. The effects on the parasympathetic system are less clear.
Localized tetanus is seen with lower toxin loads or peripheral injuries. Mortality is much lower in this group unless the cranial nerves are involved (cephalic tetanus).
Neonatal tetanus, with a particularly high mortality, is rare in developed countries but common in the developing world. Neonates present within a week of birth with fever, vomiting and ‘convulsions’. Differential diagnoses include sepsis and meningitis. The cause is usually poor umbilical hygiene and the disease is preventable by maternal vaccination, even when administered during pregnancy.
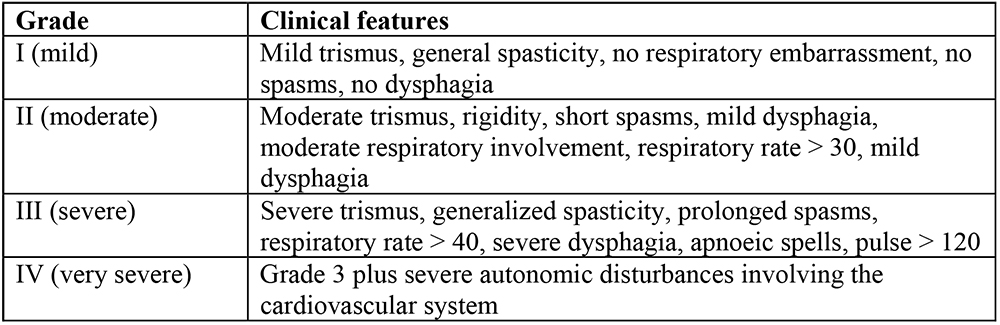
ABLETT CLASSIFICATION OF SEVERITY
MANAGEMENT OF TETANUS
Three principles apply:
1. Prevent further toxin release.
- Organise early surgical debridement of wounds, repeated as necessary.
- Give antibiotics: Metronidazole 500mg IV 8 hourly is the antibiotic of choice and benzylpenicillin 1MU IV 6 hourly is an alternative (but is a GABA antagonist). Erythromycin, tetracycline, chloramphenicol and clindamycin are acceptable choices. Remember that heavily contaminated wounds need additional antibiotic cover for other bacteria.
2. Neutralise toxin present in the body outside the CNS.
- Give human tetanus immunoglobulin (Ig) 150 units/kg IM into different sites within 24 hours of diagnosis. An intravenous preparation may be available in some centres (5000-10000iu). An alternative, where human Ig is unavailable, is to use 1500-10000 units anti-tetanus horse serum IM – anaphylaxis is a risk with this preparation and sensitivity tests are recommended.
3. Minimise the effects of the toxin already in the CNS.
- Control rigidity and spasms with sedation, give respiratory support where
necessary and control autonomic dysfunction.
SPECIFIC TREATMENT
Intensive care management is desirable, especially if respiratory and/or autonomic features are present.
Sedation.
Sedation and avoidance of unnecessary stimulation is the primary treatment for controlling spasms and autonomic dysfunction. This is usually achieved using benzodiazepines (GABA agonists), such as diazepam or midazolam (both 0.1mg/kg IV or IM 1 – 4 hourly). Midazolam can be given as an intravenous infusion (2 -10 mg/hr). Opioids, such as morphine (0.1 mg/kg IV/IM 2-6 hourly) or pethidine (1 mg/kg IV/IM 2- 6 hourly) sedate well in combination with benzodiazepines and morphine can be infused intravenously (1 – 10 mg/hr). Where available, propofol is replacing these drugs as it has less accumulation. Anticonvulsants, particularly phenobarbitone (up to 200 mg IV or PO/NG 12 hourly), and phenothiazines (usually chlorpromazine) may be added as an adjunctive sedative. Heavy sedation may be required, necessitating close monitoring of the need for formal airway control and mechanical ventilation.
Muscle relaxation is indicated where sedation alone is inadequate. Vecuronium (0.1 mg/kg IV as needed) or atracurium (0.5 mg/kg IV) are appropriate. Pancuronium may worsen autonomic instability by inhibiting catecholamine reuptake. Prolonged usage of aminosteroid muscle relaxants has been associated with critical illness neuropathy and myopathy.
The use of other drugs, such as dantrolene and intrathecal baclofen (a GABA–B agonist) is unproven.
Treatment of autonomic dysfunction.
Fluid loading is a useful in minimizing autonomic instability.
Magnesium sulphate is an effective adjunct in relaxation, sedation and controlling the autonomic disturbance in tetanus. It is a pre-synaptic neuromuscular blocker, reduces catecholamine release from nerves and the adrenal medulla, and reduces receptor responsiveness to released catecholamines. A loading dose of 5g should be given over 20 minutes, followed by an intravenous infusion of 2g/hr. The dose may be increased by up to 0.5 g/hr until spasms are relieved, or the patellar reflex disappears. If infusion devices are unavailable, give 2.5g IV every 2 hours, titrating the frequency of administration to symptoms. By antagonizing calcium metabolism, magnesium causes weakness and paralysis in overdose. Monitoring of serum magnesium levels is important to prevent this: the normal serum magnesium level is 0.7 – 1.0 mmol/l, whilst an acceptable therapeutic level is 2 – 3.5 mmol/l.
Beta-blockers (particularly long-acting agents) have been implicated in sudden cardiac death and are not recommended. The short-acting beta-blocker esmolol may be used to manage tachycardia and hypertension, where invasive monitoring is available.
The alpha-2 agonist, clonidine inhibits the release of norepinephrine from prejunctional nerve endings and may have a useful role.
GENERAL MANAGEMENT
Enteral feeding should be started early in order to prevent malnutrition caused byinability to swallow, increased metabolic rate, autonomic gastrointestinal dysfunction and muscular activity.
For patients needing artificial ventilation, steps should be taken to prevent ventilator- associated pneumonia, such as nursing in the semi-recumbent position. Prevention of respiratory complications by chest physiotherapy, mouth care and regular tracheal suctioning may be necessary due to increased secretions. Where ventilation is likely to be required for more than 8-10 days consider early tracheostomy. Adequate sedation for all procedures should minimize autonomic disturbance.
As with all patients with long-term critical illness, measures to minimize the risks of thromboembolism, gastrointestinal haemorrhage and pressure sores should be implemented. Psychological support for both the patient and relatives should be provided.
OUTCOME AND PREVENTION
Mortality varies greatly amongst units and is about 5-10 % in mild-moderate cases but rises significantly where ventilation is required, particularly in developing countries. Autonomic dysfunction and hospital-acquired infections are common causes of death.
All patients with tetanus require active immunization with tetanus toxoid, as infection does not confer immunity. In the UK, a course of five injections is recommended: a primary course at the age of 2, 3, 4 months and boosters at 5 and 15 years. In the USA, 10 yearly boosters are still recommended. Current UK guidelines for the management of wounds may be found at http://www.dh.gov.uk/assetRoot/04/11/78/31/04117831.pdf
FURTHER READING
1. Cook TM, Protheroe RT, Handel JM. Tetanus: a review of the literature. Br J Anaesthesia 2001;87: 477-87 [FULL TEXT]
2. Towey R. Tetanus: a review. Update in Anaesthesia. Issue 19, Article 17 [FULL TEXT]
3. Beeching NJ, Crowcroft NS. Tetanus in injecting drug users. BMJ, 2005; 330(7485): 208 – 209 [FULL TEXT]
ANSWERS TO MCQ
1. a, d and e are false. Tetanus is a bacillus. Exotoxins are secreted. Spores are destroyed by autoclaving, not boiling.
2. a is false. See section on Clinical Features.
3. a and d are false. Cephalic tetanus has a poor prognosis. Neonatal tetanus has a high mortality.
4. All are true. The differential diagnoses are important to know since the diagnosis of tetanus is based on clinical features.
5. a, c, d and e are false. Sedatives are the mainstay of treatment nowadays. IV not oral metronidazole is the drug of choice and infection does not confer immunity (vaccination is still required). Surgical debridement should proceed as soon as possible.



