Intensive Care Medicine
QUESTIONS
Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation.
- Following severe head injury (true or false):
a. Cerebral blood flow can fall to 50% of normal
b. Target PaCO2 should be 3.5 – 4.0kPa (26-30mmHg)
c. Cerebral perfusion pressure should be maintained above 70mmHg
d. Hypo- and hyperglycaemia worsen outcome
e. A temperature above 37°C worsens outcome - Following severe head injury indications for intubation include (true or false):
a. GCS ≤ 8
b. The presence of significant bleeding into the airway
c. Hypercarbia – PaCO2 > 6kPa (45mmHg)
d. A GCS ≤ 13 prior to inter-hospital transfer
e. A deterioration in GCS ≥ 2 prior to inter-hospital transfer - Symptoms and signs of elevated intracranial pressure may include (true or false):
a. Nausea and vomiting
b. Papilloedema
c. Pupillary constriction
d. Hypotension and bradycardia
e. Decerebrate posturing
INTRODUCTION
Head injury can be defined as any trauma to the head, other than superficial facial injuries. This term is often used interchangeably with both brain injury and traumatic brain injury.1
Every year over 1 million people present to hospital in the United Kingdom following head injury. Whilst between 80% and 90% of presentations involve mild head injury (GCS 13 – 15), the remainder include either moderate (GCS 13 – 15) or severe injuries (GCS ≤ 8).2, 3, 4
A bimodal age distribution exists, with young adults (15 to 29 years) and the elderly most commonly suffering head injuries. Men are more than twice as likely to suffer head injuries compared to women. Common causes of head injury include road traffic accidents, falls and assault.2, 5
Traumatic brain injury carries significant mortality and morbidity. Severe traumatic brain injury is associated with a mortality of approximately 40%. Furthermore, of the survivors, a significant proportion will have moderate to severe disability, with only approximately 20% making a good recovery, as described by the Glasgow Outcome Scale.4
Head injury can be subdivided into primary and secondary head injury. Primary injury refers to the initial injury, whilst secondary injury refers to factors which exacerbate the primary injury after the injury has occurred. The principles of management of severe head injury are aimed at preventing, or at least minimising, secondary injury.
NEUROPHYSIOLOGY RELEVANT TO SEVERE HEAD INJURY
A key factor in minimising secondary injury is avoiding cerebral ischaemia, by both maintaining adequate cerebral blood flow (CBF) and avoidance of conditions that increase oxygen consumption by cerebral tissues.
Hypoxia, hypotension, raised intracranial pressure (ICP) and anaemia all lead to a reduction in the delivery of oxygenated blood to cerebral tissues. Hyperthermia and epilepsy both increase cerebral metabolic rate, and therefore cerebral oxygen consumption. In addition, both hypoglycaemia and hyperglycaemia are associated with a worse outcome.2
Normal cerebral blood flow is approximately 50 mls/100g brain tissue per minute (mls/100g/min). Under normal circumstances autoregulation ensures that cerebral blood flow remains constant over arange of cerebral perfusion pressures (CPP). Autoregulation is thought to result from changes in vascular smooth muscle tone in response to vascular wall tension. Figure 1, below, illustrates that cerebral blood flow remains constant over cerebral perfusion pressures ranging from 60 to 160mmHg. Following severe head injury these autoregulatory mechanisms are often disrupted meaning cerebral blood flow becomes proportional to cerebral perfusion pressure.3, 5, 6
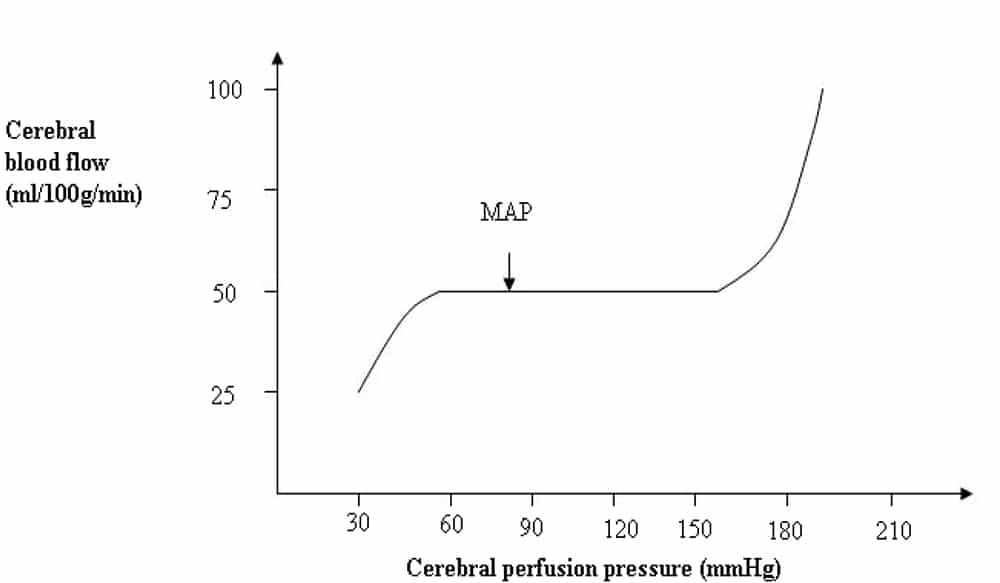
Figure 1. Graph illustrating changes in Cerebral Blood Flow with Cerebral Perfusion Pressure [Reproduced with permission from Hill and Gwinnutt (2007)]
As cerebral blood flow is difficult to measure, cerebral perfusion pressure is used as a surrogate marker for cerebral perfusion. Cerebral perfusion pressure is determined by mean arterial pressure (MAP), venous pressure (VP) and intracranial pressure:
CPP = MAP – (ICP + VP)
Under normal circumstances the venous pressure at the jugular bulb is zero or less, therefore, cerebral perfusion pressure is determined by the difference between MAP and ICP.7
CPP = MAP – ICP
It is this simplified version of the equation which is commonly used in clinical practice3, 8 and also by the Advanced Trauma Life Support and Brain Trauma Foundation guidelines.
Under normal circumstances cerebral blood flow is autoregulated across a range of cerebral perfusion pressures, following head injury autoregulatory mechanisms are often disrupted and cerebral blood flow becomes proportional to cerebral perfusion pressure. Previously, following severe head injury, a cerebral perfusion pressure of 60 to 70mm Hg was targeted. The most recent edition of the Brain Trauma Foundation guidelines (2007) suggest a target cerebral perfusion pressure of between 50 and 70mmHg.3, 8
As illustrated by the equation above, any increase in intracranial pressure will result in a decrease in cerebral perfusion pressure. Normal intracranial pressure is between 5 and 15mmHg; treatment should be initiated to lower ICP once it exceeds 20mmHg.8, 9
The relationship between intracranial pressure and changes in intracranial volume post-injury can be better understood by reviewing the Monro-Kellie hypothesis. This states that the cranium is rigid and fluid cannot be compressed. Therefore any increase in intracranial content will result in an increase in pressure. The intracranial contents consist of brain tissue, blood, CSF and extracellular fluid. Initially, any increase in volume of one of the contents is met by an equal decrease in the volume of another of the contents, preventing a rise in intracranial pressure. However, this compensation is limited to 100 to 150mls, after which intracranial pressure rises significantly. Figure 2 illustrates this and it can be seen that initial volume increase is compensated and does not result in significant pressure rise (flat section). Once the compensatory mechanisms are exhausted, a critical volume decompensation occurs and intracranial pressure rises rapidly with only small increases in volume.3
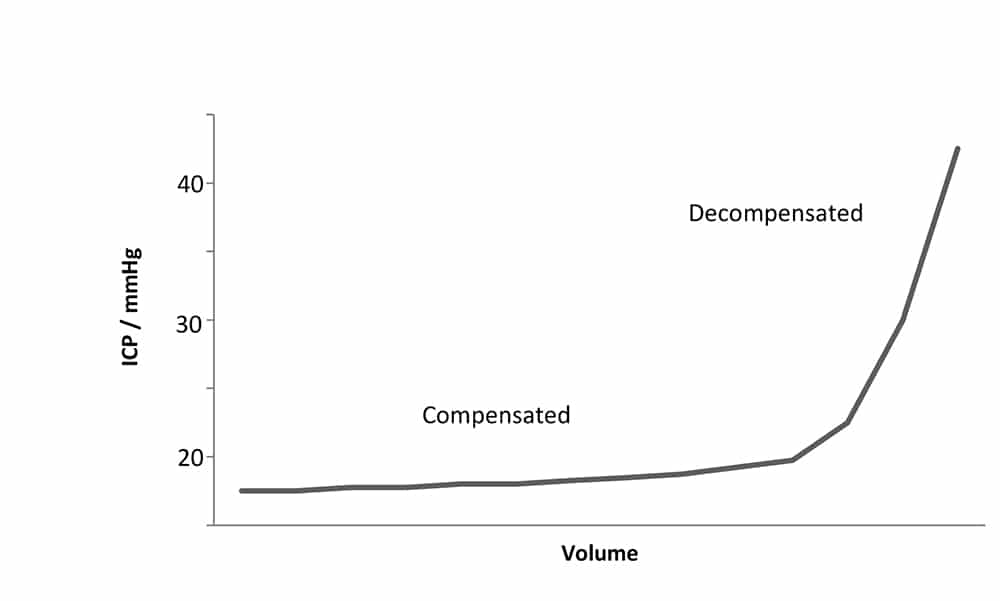
Figure 2. Diagram illustrating change in intracranial pressure with increased intracranial volume
Following head injury, a rise in intracranial pressure may result from an increase in intracranial blood volume (e.g. extradural haematoma), from an increase in cerebrospinal fluid volume (e.g. obstructivehydrocephalus) or from an increase in extracellular fluid volume (e.g. cerebral oedema).
Both CO2 and O2 can also influence ICP, through changes in cerebral blood flow and blood volume. CO2 exerts the greater influence – with a 15 – 30% increase in cerebral blood flow per kPa increase in PaCO2 (2-4% per mmHg). Figure 3, illustrates this relationship between PaCO2 and cerebral blood flow.6, 9
O2 affects cerebral blood flow to a lesser degree – only causing an increase when PaO2 falls below 8kPa (60mmHg). As significant changes in intracranial pressure may result, both CO2 and O2 must be carefully controlled.9
In summary, the brain following severe head injury is extremely susceptible to further physiological insults. Management is aimed at maintaining an adequate cerebral blood flow and avoiding conditions which increase cerebral oxygen consumption.

Figure 3. Graph illustrating changes in Cerebral Blood Flow with PaCO2[Reproduced with permission from Hill and Gwinnutt (2007)]
INITIAL ASSESSMENT AND MANAGEMENT OF THE HEAD INJURED PATIENT
Assessment
Patients may present with head injuries in isolation or in conjunction with other injuries. Up to 50% of patients with severe traumatic brain injury have major extra-cranial injuries. As a result the presence of co-existing injuries should be actively sought and excluded. A systematic approach to evaluation and initial management, such as that proposed by Advanced Trauma Life Support, should be adopted for these patients.4
Airway patency should be assessed and the cervical spine immobilised. The airway should be secured, by tracheal intubation, in patients who do not have a patent airway or who are significantly obtunded (GCS ≤ 8). The chest should be examined and any life-threatening injuries (e.g. tension pneumothorax, open pneumothorax, massive haemothorax, flail chest, cardiac tamponade) promptly treated.3
The circulatory state should be assessed using clinical parameters such as blood pressure and heart rate. Any sites of external haemorrhage should be directly compressed. Patients with suspected or confirmed on-going haemorrhage will require operative intervention. 3
An assessment of the patient’s Glasgow Coma Score (GCS) and pupillary reflexes should be made. In addition, the presence of any lateralising neurological signs, and, in the case of spinal cord injury, a documentation of the level of altered sensation, should also be noted.
The patient should be completely exposed to assess for other injuries, whilst taking care to prevent hypothermia. All aspects of the primary survey should be completed and identified life-threatening conditions treated, before commencing the secondary survey.
In the situation where life-threatening airway, thoracic or circulatory problems present together with life-threatening neurological injuries, priority is given to the definitive treatment of the former. Practically speaking this may mean, for example, the haemodynamically unstable polytrauma patient with a ruptured spleen and extradural haematoma undergoes splenectomy at the district general hospital before transfer to the neurosurgical centre for surgical evacuation of the extradural haematoma.
Specific Neurological Assessment and Investigation
The Glasgow Coma Score is used to formally assess the conscious level of the patient. This score, illustrated in Table 1 below, is composed of 3 components: eye-opening, verbal and motor response. The best response in each component is used to calculate the final score, which ranges from 3, at worst, to 15, at best.
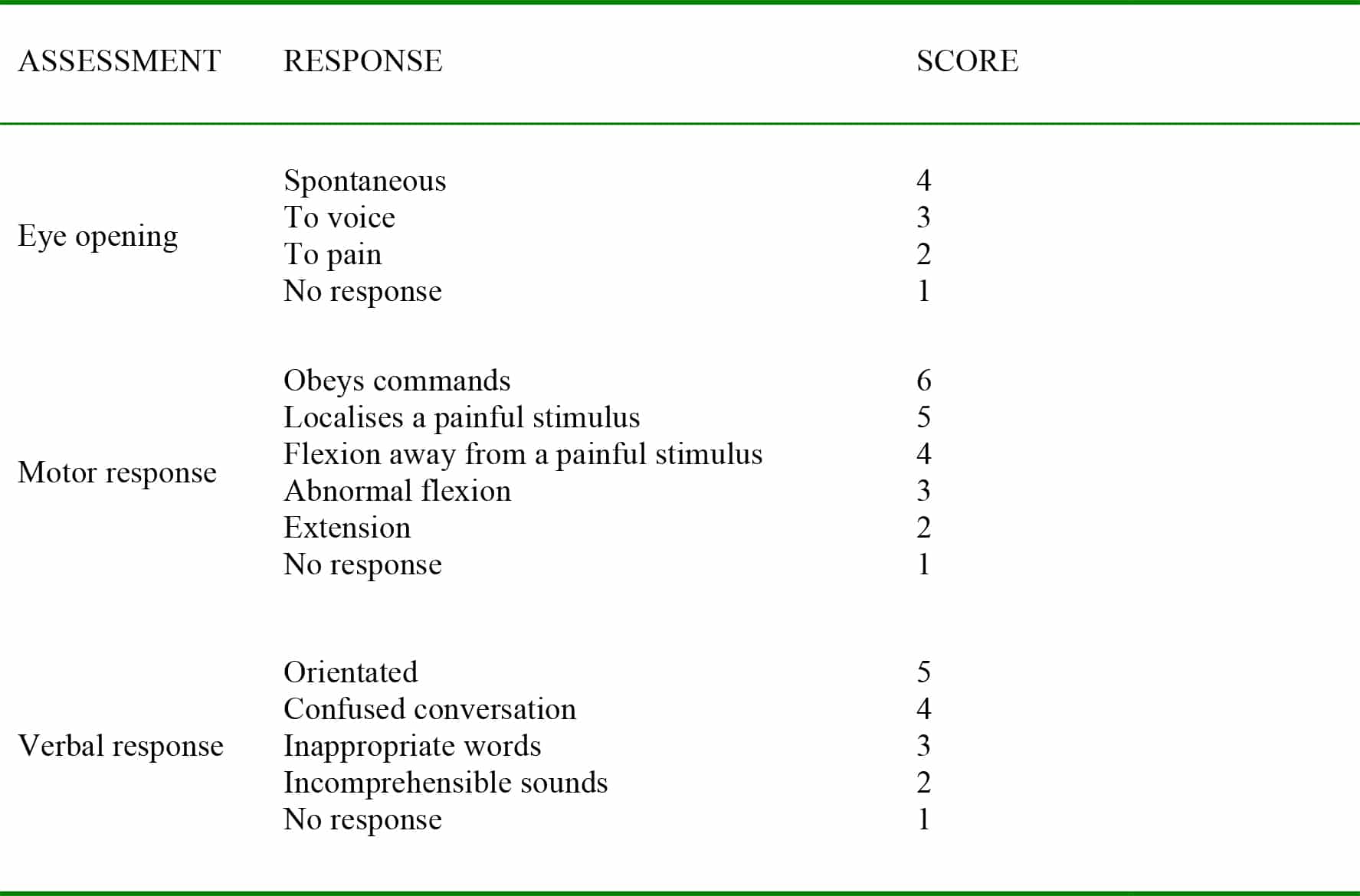
Table 1: Glasgow Coma Score3
Pupillary size and response to light should be assessed and recorded. Ipsilateral pupillary dilatation, unreactive to light, may indicate life-threatening intracranial pressure. In this situation, pupillary dilatation results from compression of the oculomotor nerve against the tentorium. Alternative causes include ocular trauma and the administration of certain drugs.4
Early symptoms and signs associated with raised intracranial pressure include headache, nausea and vomiting, seizures, papilloedema and focal neurology. Late signs of raised intracranial hypertension include a decrease in conscious level, hypertension and bradycardia (Cushing’s reflex) and an abnormal respiratory pattern. Pupillary dilatation, decorticate posturing (leg extension, arm flexion) and decerebrate posturing (leg and arm hyperextension) occur prior to coning and brain death.
Following head injury, the diagnostic investigation of choice is a CT scan of the head. Indications for patients requiring an urgent CT scan are listed in Box 1.
In addition to the these indications, other indications, for example amnesia of events occurring more than thirty minutes prior to injury, warrant CT scanning, but less urgently. Frequent assessment and reassessment of patient status, in particular conscious level and pupillary responses, are essentially. Deterioration in patient condition may warrant urgent imaging.1
Box 1: Guidelines for urgent CT scanning in head injury1
- GCS < 13 on initial assessment
- GCS < 15 on assessment 2 hours post-injury
- Definite or suspected open or depressed skull fracture
- Signs of basal skull fracture (e.g. Battle’s sign)
- Post-traumatic seizure
- Focal neurological deficit
- >1 episode of vomiting
- Any history of amnesia or loss of consciousness post-injury in a patient who is coagulopathic (clotting disorder, warfarin treatment)
Indications for involvement of the neurosurgical team following head injury are listed in Box 2 below. The exact definition of “surgically significant abnormalities” is determined by the local neurosurgical unit.
Box 2: Guidelines for neurosurgical referral in head injury1
- Presence of new, surgically significant abnormalities on imaging
- GCS ≤ 8 after initial resuscitation
- Unexplained confusion lasting > 4 hours
- Deterioration in GCS after admission
- Progressive focal neurological signs
- Seizure without full recovery
- Definite or suspected penetrating injury
- CSF leak
Initial Management
Airway
Indications for intubation following head injury are listed in Box 3 below. If the cervical spine has not been cleared manual in-line stabilisation is required for intubation.
The dose and type of induction agent(s) chosen should be selected with the aims of rapidly securing the airway with minimal haemodynamic disturbance and minimal rise in ICP. With the exception of ketamine, all intravenous induction agents cause a reduction in cerebral blood flow, cerebral metabolism and intracranial pressure. In circumstances where ketamine is the only available induction agent it should be used with caution as it causes a rise in intracranial pressure. The use of intra-arterial monitoring, sited pre-induction, allows more rapid detection and treatment of hypotension.7
In the uncomplicated airway a modified rapid sequence induction using a pre-determined dose of thiopentone or propofol together with an opioid (alfentanil, fentanyl) and suxamethonium can be used. The use of an opioid obtunds the pressor response to laryngoscopy and the associated, potentially life threatening rise in intracranial pressure. A vasopressor, such as metaraminol, should be readily available to counter any hypotension.
Although suxamethonium may itself cause a rise in intracranial pressure, this is rarely clinically significant as is offset by the reduction in intracranial pressure caused by the induction agent. The benefits of suxamethonium in facilitating adequate intubating conditions, as well as its short duration of action are often deemed to outweigh this risk in practice. With the availability of sugammadex, rocuronium can be used as an alternative to suxamethonium. Following intubation and confirmation of endotracheal placement, the tube should be well secured in a fashion that ensures venous return is not obstructed. This is most easily achieved using tape rather than a cloth tie.
Box 3: Indications for Intubation Post-Head Injury1, 10
- Airway
- Loss of airway reflexes
- Significant bleeding into the airway
- Breathing
- Hypoxia – PaO2 < 13kPa (98mmHg) on oxygen
- Hypercarbia – PaCO2 > 6kPa (45mmHg)
- Spontaneous hyperventilation causing PaCO2 < 4kPa (30mmHg)
- Irregular respirations
- Disability
- GCS ≤ 8
- Seizures
- Other
- Before transfer to neurosurgical unit AND
- Bilateral fractured mandible
- Deteriorating conscious level (a decrease of 1 or more points in the motor component of the GCS)
- Before transfer to neurosurgical unit AND
Breathing
Both hypoxia and hypo- and hypercapnia should be avoided in patients with head injuries as these worsen outcome. Hypoxia, as defined as a SaO2 < 90% or PaO2 < 8kPa (60mmHg), increases morbidity and mortality from severe traumatic brain injury. A target PaO2 > 13kPa (98mmHg) should be aimed for. In the ventilated patient this may require use of PEEP. Whilst this will increase ICP to a degree, hypoxia is more likely to have a detrimental effect on patient outcome.8, 10
Hypercapnia, through increasing cerebral blood flow, causes a rise in ICP. Conversely, hypocapnia, although lowering ICP, also lowers cerebral perfusion and may worsen ischaemia. To achieve adequate cerebral perfusion, without significantly increasing ICP, a PaCO2 of 4.5 – 5.0kPa (34-38mmHg) is targeted. In the patient with clinical or radiological evidence of intracranial hypertension modest hyperventilation can be instituted, but maintaining PaCO2 above 4kPa (30mmHg).9, 10
In the ventilated patient, arterial blood gas analysis should be used calibrate end-tidal CO2 to PaCO2. Where appropriate changes in ventilatory settings should be instituted to ensure the above target is achieved. Continuous capnography should be used in all ventilated patients.
Circulation
Hypotension increases morbidity and mortality in severe traumatic brain injury. A cerebral perfusion pressure of 50 – 70 mmHg should be targeted. In cases where the ICP is not measured but suspected to be raised, maintenance of a mean arterial pressure of over 80mmHg should ensure an adequate cerebral perfusion pressure in all but the most severe cases of raised intracranial pressure. Once normovolaemia has been achieved a vasopressor, such as metaraminol or noradrenaline, may be required to maintain mean arterial pressure at this level and offset the hypotensive effect of any anaesthetic agents used.4, 8, 10
A carefully considered fluid strategy is required. The aim is to achieve a balance between maintaining normovolaemia and end-organ perfusion without worsening cerebral oedema through excessive fluid administration. With increased sodium content, 0.9% sodium chloride (Na+ 154 mmol/l) is often used, with careful attention required to avoid causing a hyperchloraemic acidosis. Hypotonic fluids, such as 5% dextrose, should be avoided.
Disability
Without an ICP monitor the first signs of raised ICP may be “late signs” of hypertension, bradycardia and pupillary dilatation. If above targets are being achieved and the patient is adequately sedated, nonsurgical therapeutic strategies may include the use of osmotherapeutic agents, such as mannitol or hypertonic saline, cooling, moderate hyperventilation (PaCO2≥ 4kPa or 30mmHg) and the use of thiopentone. Management of intracranial hypertension will be discussed in detail later.
Both hypoglycaemia and hyperglycaemia can worsen brain injury. A blood glucose of 4 – 8 mmol/l is targeted. Seizures increase cerebral oxygen consumption and can produce cerebral ischaemia. Seizures should be treated promptly with appropriate anti-epileptics (e.g. phenytoin, 18mg/kg). In certain situations the neurosurgical team will recommend the administration of anti-epileptics prophylactically. As cerebral metabolic rate is directly related to body temperature, hyperthermia can also increase cerebral oxygen consumption. Hyperthermia, a temperature of greater than 37ºC, should be avoided.
Box 4: Summary of Therapeutic Targets in Managing Severe Head Injury
- PaO2 > 13kPa (98mmHg)
- PaCO2 of 4.5 – 5.0kPa (34- 38mmHg)
- A lower PaCO2 , ≥ 4kPa (30mmHg), should be targeted with clinical or radiological signs of intracranial hypertension
- MAP ≥ 80 mmHg (in the absence of ICP monitoring)
- Glucose 4 – 8 mmol/l
- Temperature < 37°C
- If ICP monitoring in situ
- CPP 50 – 70mmHg
- ICP < 20mmHg
MANAGEMENT OF RAISED INTRACRANIAL PRESSURE
ICP above 20mmHg requires urgent treatment. In the absence of ICP monitoring, the first indication of intracranial hypertension may be haemodynamic and pupillary signs.8
In the patient with a lesion amenable to surgery awaiting transfer from a non-neurosurgical centre these signs, if new, mandate immediate discussion with the neurosurgical team and emergent expedition of the transfer. In the patient without a lesion amenable to surgery initially, depending on the underlying injury and duration of time since last imaging, consideration should be given to re-imaging and / or further discussion with the neurosurgical team. Whilst awaiting transfer, and for those patients who do not have a lesion amenable to surgery, medical treatment of intracranial hypertension should be initiated.
A systematic approach to assessment and management is essential in these patients. In our regional neurointensive care unit a protocol for the management of the severely head injured patient exists. The introduction of protocolized management in such patients is associated with a reduction in mortality of approximately 7%.11
Initially, the patient should be re-assessed to ensure basic therapeutic targets are achieved (PaCO2 ~ 4.5kPa (34mmHg), PaO2 > 13kPa (98mmHg), temperature < 37ºC). Any obvious cause for intracranial hypertension, such as obstruction of venous return or lightening of sedation leading to coughing, should be treated. 2, 5
Osmotherapeutic agents, such as mannitol (0.25 – 0.5g / kg) or aliquots of hypertonic saline (e.g. 100mls 5% saline), may be used to lower ICP. Both agents, through an increase in serum osmolality, cause water to move from the intracellular and interstitial spaces to the intravascular space. As well as reducing cerebral oedema and intracranial pressure, this increase in intravascular volume produces an increase in cardiac output and a reduced blood viscosity. All of these features contribute to an improvement in cerebral blood flow and oxygen delivery.2, 5
For the patient awaiting or undergoing transfer, the only feasible additional therapy is the use of moderate hyperventilation. Ventilation is increased to achieve a target PaCO2 of approximately 4kPa (30mmHg) with the aim of further reducing ICP through reducing cerebral blood flow. However, whilst hyperventilation reduces ICP, the resultant cerebral vasoconstriction can worsen perfusion. Aggressive hyperventilation (PaCO2 < 3.5kPa / 26mmHg) may worsen outcome. Figure 3, above, illustrates the relationship between cerebral blood flow and PaCO2.2, 3
Within the intensive care environment additional refractory therapies may be employed. Therapeutic hypothermia, cooling to 34ºC, can be induced. This reduces cerebral metabolic rate and cerebral oxygen consumption. A neuromuscular blocker is required to prevent shivering. Other side-effects of cooling include immunosuppression, coagulopathy and pancreatitis.2
Thiopentone can also be used to suppress cerebral metabolism. An induction dose of 3 – 5 mg/kg is given followed by an infusion of 3 – 5mg/kg/hour. EEG monitoring is used to ensure that burst suppression is achieved. A final intervention for intracranial hypertension refractory to other therapies is decompressive crainectomy. In this procedure a bone flap is removed from the skull in an attempt to decompress cerebral swelling.2, 5
CONCLUSION
In conclusion, severe traumatic brain injury is a not uncommon emergency presentation and is associated with significant mortality and morbidity. In addition, patients may present with head injuries in isolation or in conjunction with other injuries. A systematic approach to initial assessment and management is required for such patients. Key to the management of the head injured patient are strategies aimed at preventing, or at least minimising, secondary brain injury through maintenance of an adequate cerebral blood flow and avoiding conditions which increase cerebral oxygen consumption.
ANSWERS TO QUESTIONS
- Following severe head injury (true or false):
- Cerebral blood flow can fall to 50% of normal – True. Following severe head injury cerebral blood flow can fall from approximately 50mls/100g brain tissue/min to 25mls/100g brain tissue/min.
- Target PaCO2 should be 3.5 – 4.0kPa (26-30mmHg) – False. Target PaCO2 should be between 4.5kPa and 5.0kPa (34- 38mmHg). In the presence of clinical or radiological evidence of raised intracranial pressure modest hyperventilation can be used, but maintaining PaCO2 > 4kPa (30mmHg).
- Cerebral perfusion pressure should be maintained above 70mmHg – False. Target cerebral perfusion pressure should be between 50 and 70mmHg.
- Hypo- and hyperglycaemia worsen outcome – True.
- A temperature above 37°C worsens outcome – True.
- Following severe head injury indications for intubation include (true or false):
- GCS ≤ 8- True.
- The presence of significant bleeding into the airway – True.
- Hypercarbia – pCO2 > 6kPa (45mmHg) – True
- GCS ≤ 13 prior to inter-hospital transfer – False.
- A deterioration in GCS ≥ 2 prior to inter-hospital transfer – True
- Symptoms and signs of elevated intracranial pressure may include (true or false)
- Nausea and vomiting – True. Although non-specific, nausea and vomiting may represent an early symptom of raised intracranial pressure
- Papilloedema – True
- Pupillary constriction – False. Raised intracranial pressure causing oculomotor nerve compression causes pupillary dilatation and is a late sign of raised intracranial pressure
- Hypotension and bradycardia – False. Hypertension and bradycardia is a late sign of raised intracranial pressure.
- Decerebrate posturing – True
REFERENCES and FURTHER READING
- National Institute for Health and Clinical Excellence NICE Clinical Guideline 56: Head Injury. Triage, assessment, investigation and early management of head injury in infants, children and adults (2007) http://www.nice.org.uk/nicemedia/live/11836/36259/36259.pdf
- Girling, K Management of head injury in the intensive-care unit Continuing Education in Anaesthesia, Critical Care and Pain (2004); 4: 52 – 56
- American College of Surgeons Advanced Trauma Life Support for Doctors (Student Course Manual), Eighth Edition, p20 – 21, p131 – 151 Published by the American College of Surgeons, Chicago (2008)
- Moppett, I Traumatic brain injury: assessment, resuscitation and early management British Journal of Anaesthesia (2007); 99: 18 -31 http://bja.oxfordjournals.org/content/99/1/18.full.pdf+html
- Marik, P; Varon, J and Trask, T. Management of Head Trauma. Chest. 2002; 122; 699 – 711 http://chestjournal.chestpus.org/content/122/2/699.full.pdf+html
- Hill, L and Gwinnutt, C (2007) Cerebral Physiology Part 1 – Cerebral Blood Flow and Pressure http://totw.anaesthesiologists.org/wp-content/uploads/2007/10/69-Cerebral-Physiology-part- 1.pdf
- Allman, K and Wilson, I Oxford Handbook of Anaesthesia, Third Edition, p404, p406 Published by Oxford University Press, Oxford (2011)
- Brain Trauma Foundation, American Association of Neurological Surgeons (AANS), Congress of Neurological Surgeons (CNS) and AANS/CNS Joint Section on Neurotrauma and Critical Care Guidelines for the Management of Severe Traumatic Brain Injury, Third Edition (2007) http://www.braintrauma.org/pdf/protected/Guidelines_Management_2007w_bookmarks.pdf
- Power, I and Kam, P Principles of Physiology for The Anaesthetist, p42 – p43 Published by Arnold Publishers, London (2001)
- The Association of Anaesthetists of Great Britain and Ireland Recommendations for The Safe Transfer of Patients with Brain Injury (2006) http://www.aagbi.org/publications/guidelines/docs/braininjury.pdf
- Clayton, T; Nelson, R and Manara, A. Reduction in mortality from severe head injury following introduction of a protocol for intensive care management. Brit J Anaesth. 2004; 93;761 – 767 http://bja.oxfordjournals.org/content/93/6/761.full.pdf+html



