Covid-19
QUESTIONS
Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation. Please answer True or False:
- A 69-year old woman presents to the emergency department with a 3-day history of worsening stridor. A mobile lesion obstructing 70% of the glottis is seen on fibreoptic nasal endoscopy
a. Immediate medical management in the form of humidified oxygen, nebulised adrenaline and intravenous steroids should be considered
b. Transfer of the patient to theatre does not require specialist staff or equipment
c. Induction in the anaesthetic room is ideal
d. Face mask ventilation is likely to be easy
e. Examination of the neck and identification of the cricothyroid membrane using ultrasound is advisable - The following statements are correct with regard to endotracheal intubation
a. Direct laryngoscopy is likely to be easy with a base of tongue tumour
b. Videolaryngoscopy may produce a good view of the glottis however intubation may still be difficult
c. Awake fibreoptic intubation may result in complete obstruction in a critical airway
d. Transnasal humidified rapid inspiratory ventilatory exchange (THRIVE) can be used in conjunction with direct and indirect laryngoscopy
e. The United Kingdom National Audit project on Major Airway Complications recommended multiple attempts at laryngoscopy in patients with head and neck pathology - Regarding induction of anaesthesia
a. Inhalational induction of anaesthesia using a spontaneously breathing technique is always the best option in an obstructed airway
b. Elective narrow-bore needle cricothyroidotomy may be considered as an option prior to induction
c. Awake tracheostomy can be a difficult procedure in an obstructed airway
d. The introduction of Sugammadex means that all patient should have an intravenous induction
e. Knowledge of human factors in complex airway management is less important than technical expertise
Key Points
- It is important to identify the nature, level and speed of onset of airway obstruction when planning a management strategy
- Fibreoptic nasendoscopy, CT, and MRI should be considered where time allows to investigate the extent of the obstructing lesion
- Management of airway obstruction requires a multidisciplinary approach, with senior anaesthetic and surgical input from an early stage
- A key consideration in the management strategy is whether the airway should be secured awake
- Anaesthetists should be familiar with and regularly practice can’t intubate can’t oxygenate (CICO) drills
- Appreciation of human factors are instrumental to the successful management of a difficult airway
INTRODUCTION
Obstruction of the airway at its most extreme is an anaesthetic emergency requiring immediate intervention. In advanced life support algorithms, it usually refers to loss of airway patency in the unconscious patient or blockage by a foreign body in the event of choking. In these cases, airway opening manoeuvres or back blows and abdominal thrusts to relieve an obstruction may be life-saving before hypoxia and cardiac arrest ensue. In the context of this article, we will be discussing management of airway obstruction relating to pathology of the head and neck.
Airway obstruction may present acutely or chronically depending on the site, degree of narrowing and cause. The anatomical level can broadly be categorised as supraglottic, glottic (laryngeal) or subglottic (Figure 1). The obstruction may be due to luminal pathology such as inflammation, tumour or haematoma or it may result from external compression and distortion. Central airway compromise due to anterior mediastinal masses can pose difficulties by nature of the obstruction being sited distal to surgical airway rescue1. Management of the obstructed airway is particularly challenging and accounted for 40% of all cases (72 out of 184 patients) reported to the 4th UK National audit project of major airway complications (NAP 4)2. Important recommendations arising from the review of these cases have been instrumental in guiding the assessment, planning and management strategies of patients with an obstructed airway to optimise their outcome.
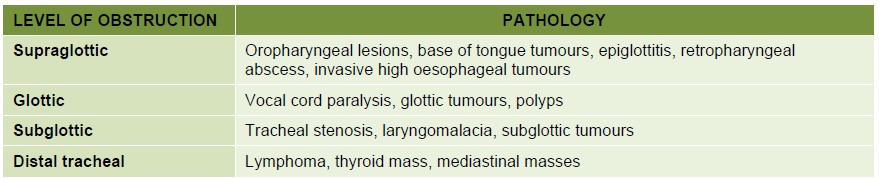
Figure 1. Potential pathological causes of airway obstruction
PATIENT ASSESSMENT
Symptoms and signs
A thorough history should be taken if the urgency of the situation allows. There may be a history of previous airway problems and / or previous radiotherapy to the head and neck. Anaesthetic records and any difficult airway alert forms should be reviewed.
Symptoms and signs generally reflect the site, extent of narrowing and its speed of onset (Figure 2). In an acute obstruction, for example due to trauma, epiglottitis or Ludwig’s angina (cellulitis of the floor of the mouth and submandibular tissues), stridor and dyspnoea are commonly encountered. Stridor is a harsh, high-pitched noise created by turbulent airflow through a partially obstructed airway. It implies a reduction in airway diameter of at least 50%3. In the inspiratory phase, stridor points to obstruction at a supraglottic or glottic level, whereas biphasic inspiratoryexpiratory stridor implies subglottic compromise4. Expiratory stridor or wheeze classically suggests tracheal or tracheobronchial obstruction. Stertor is a term to describe heavy snoring respiration and is usually generated from obstruction at a nasopharyngeal level whereas gurgling may suggest an oropharyngeal origin1. Other pertinent symptoms of airway obstruction include hoarseness, voice change, a preference for sitting up, nocturnal dyspnoea, orthopnoea, worsening fatigue, dysphagia and drooling.
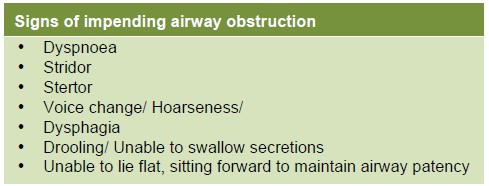
Figure 2. Table showing signs of airway obstruction
Chronic obstruction may present insidiously as patients become gradually conditioned to progressive narrowing of the airway. Adequate alveolar minute ventilation can be achieved at rest through an orifice as little as 3 millimetres when respiratory muscles have become trained1. A patient who appears uncompromised and asymptomatic in this situation is falsely reassuring. Stridor and sudden deterioration may only occur as critical obstruction is reached. Slow-growing tumours of the pharynx, base of tongue, vocal cords, those causing external compression such as from the thyroid and mediastinum, and some neuromuscular diseases may evolve in this way.
In addition to the above symptoms, patients with a mediastinal obstruction may report chest pain or fullness, sweats, symptoms of superior vena cava obstruction, postural cough and syncope5. Alternatively they may be asymptomatic with incidental finding of a mass reported on imaging.
Examination
The posture adopted by the patient should be noted. They may be dyspnoeic, using accessory muscles of respiration and require supplementary oxygen. Assessment of the airway should include mouth opening, dentition, tongue protrusion, Mallampati classification, jaw subluxation and neck movement. The neck should also be examined for masses, mobility of the trachea, airway distortion and any potential difficulties for front of neck access (e.g. previous radiotherapy)6.
Investigations
Fibreoptic nasendoscopy (Figure 3) should be performed where possible; either in clinic, at the bedside or in theatre, depending on the urgency of the situation. This is usually well tolerated by the patient. Inspection of the larynx in this way can provide important information about the nature, level and degree of obstruction, attachment to surrounding structures and any movement of the lesion during respiration. It may also enable anticipation of the effects of traumatising the lesion if it appears vascular or friable. These findings should be discussed with the surgical team to help formulate a management strategy. It is important to anticipate that induction of anaesthesia and postural change may worsen the degree of obstruction seen.
Ultrasound examination of the neck may provide additional information about the lesion and degree of airway distortion, especially if no landmarks are palpable. It is also valuable for identifying and marking the cricothyroid membrane and noting any overlying vascular structures if front-of-neck access is contemplated6.
MR and CT imaging is recommended where time and the patient conditions allow (lying flat may result in worsening of symptoms) to further investigate the extent of any lesion2 (Figure 4). Imaging is particularly helpful in delineating a mediastinal mass. A CT will demonstrate the position and extent of the airway obstruction.
Awake CT-guided needle biopsy may be an option to avoid manipulation of the airway under anaesthesia. Patients with cardiovascular symptoms or signs should be investigated using echocardiography as this may be a feature of mediastinal masses5.
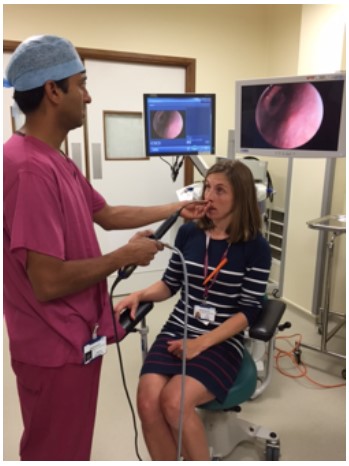
Figure 3. The authors undertaking fibreoptic nasendoscopy
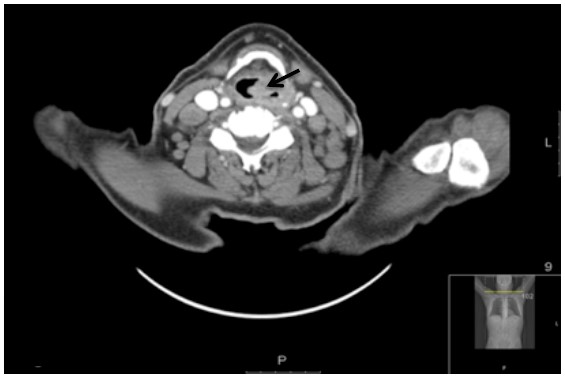
Figure 4. CT image of a supraglottic lesion (black arrow) in an 82-year old man, demonstrating the level and extent of airway obstruction
MULTIDISCIPLINARY TEAM, PLANNING AND HUMAN FACTORS
Management of patients with an obstructed airway requires senior anaesthetic and surgical input from an early stage2. The case should be jointly assessed where possible to clarify the level, extent and likely cause of the obstruction. In chronic cases, imaging should ideally be reviewed in a multidisciplinary team setting and chaired by radiologists with head and neck expertise.
For patients requiring urgent intervention, theatre staff should be alerted to prepare specialist teams and equipment. Plans should be made to secure the airway in theatre alongside the rest of the team rather than in the anaesthetic room2. Inter or intra hospital transfer of an unstable patient should be done by medical personnel with airway expertise. Equipment must be immediately available for airway maintenance or attempt to secure the airway if necessary. In extreme cases such as central airway obstruction, a patient may require transfer to a specialist centre capable of instituting cardiopulmonary bypass (CPB) before induction of anaesthesia. This decision should be made early by the multidisciplinary team, as using CPB as a back-up plan in the event of complications is unlikely to yield successful outcome5.
Careful consideration of the relative risks and benefits of the proposed airway strategy, preparation of equipment, and contingency planning are key to the successful management of an anticipated difficult airway. Clear role assignment and briefing of the multidisciplinary team, and an appreciation of human factors are vital7. The leader should be clearly identified (usually the most senior anaesthetist present) and should ensure clear communication and good teamwork as the clinical situation may rapidly change.
MANAGEMENT STRATEGIES
In an emergency situation the nature of the obstruction may be unknown and the location, expertise and equipment may be lacking. Optimising the ability to oxygenate is fundamental to all airway stratgies1. Immediate medical management should include high-flow humidified oxygen and consideration of intravenous corticosteroids. Nebulised adrenaline and Heliox (79% helium / 21% oxygen mixture) may also be indicated although the latter does restrict the amount of oxygen that can be given. Where it becomes necessary to secure the airway, assistance from an anaesthetist skilled in advanced airway techniques should be urgently sought. The Difficult Airway Society (DAS) guidelines for the management of an unanticipated difficult intubation should be followed8. Anaesthetists should be familiar with and regularly practice “cant-intubate, can’t oxygenate” drills, including front of neck access.
The Aintree Difficult Airway Management (ADAM) website9 is a useful aid to decision making. It identifies 10 devices which can potentially facilitate management of the difficult airway, ranging from conventional direct laryngoscopy to videolaryngoscopy, rigid and flexible fibreoptic laryngoscopy and needle or surgical cricothyroidotomy. A difficult airway scenario can be selected from a drop down menu and a problem list is completed. The ADAM website then generates a management matrix which rates the utility of each device as recommended by a panel of experts from 1 – 5 (1 – minimally hazardous, 5 – extremely hazardous). The summary rating is the worst hazard rating for each device. It then allows for a printable contingency plan to be generated with observed problems and steps to intubation with the device. This website can be accessed free of charge by registered medical professionals who can request a login at http://adam.liv.ac.uk/adam8/login.aspx (Figure 5 and 6).
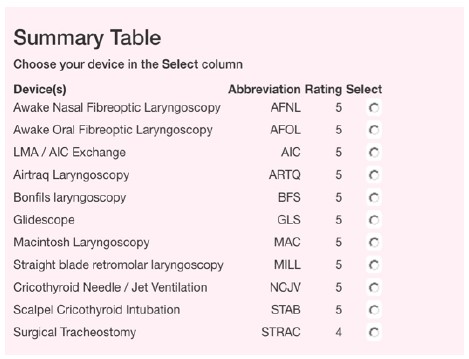
Figure 5. This is an example of the ADAM difficult airway device summary table that is generated for the scenario of a supraglottic laryngeal tumour. The summary matrix gives the “worst score” for the device (1 – minimal hazard, 2 – 4 increasing hazardous, 5 – extremely hazardous). In this scenario all devices have some aspect of their use that is hazardous, by clicking ‘select’ a contingency plan is generated for that device, with problems that may be encountered and steps on how to use the device (see figure 7).
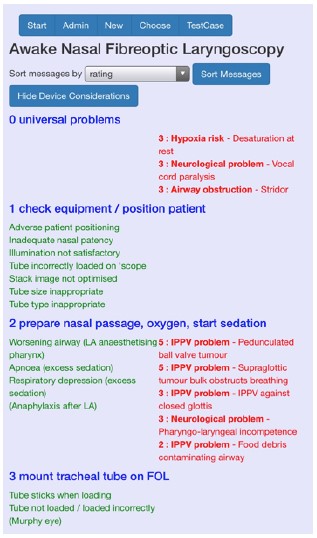
Figure 6. Awake Nasal Fibreoptic laryngoscopy has been selected which gives a contingency plan. Blue text = sequence of steps required for a successful intubation, green text = everyday problems in using the device, red = observed problems for this case and the ADAM rating for them (NB only the start of the plan is illustrated here).
AIRWAY STRATEGIES
There are four main options to consider when planning an airway strategy (Figure 7):
- Inhalational induction
- Intravenous induction
- Awake fibreoptic intubation
- Awake tracheostomy
NAP-4 identified that the site of obstruction in particular has a great influence on the efficacy and suitability of a technique2. We will consider these four techniques in turn.
Inhalational induction of anaesthesia
Inhalational induction of anaesthesia has classically been described as the preferred route in a patient with upper airway obstruction10 and specifically in patients with central airway obstruction5. Theoretically, this technique preserves spontaneous ventilation and should the patient completely obstruct due to airway collapse, the uptake of vapour would cease and awakening would ensue. In practice with severe obstruction, the onset of induction is slow and may precipitate laryngospasm or apnoea with subsequent hypoxia1,3. NAP 4 emphasised the risks of inhalational induction with reports of 23 out of 27 cases becoming significantly compromised. In some cases, this necessitated rescue front-ofneck access2. Reports demonstrated that in the event of compromise, patients did not rapidly waken as suggested. It is therefore vital to have a contingency plan in place when this technique is considered. This may involve administration of neuromuscular blockade and mask ventilation if possible pending intubation1. The use of halothane to facilitate instrumenting of the airway under deep inhalational anaesthesia has all but disappeared in the UK but is a technique employed in many low to middle income countries due to its ready availability and the lack of advanced airway equipment. Inhalational induction is still commonly used in difficult paediatric airways where there is less likely to be airway collapse and it is possible to maintain airflow.
Intravenous induction of anaesthesia
The choice between inhalational and intravenous induction can be difficult and both scenarios may fail1. Carefully planned back-up techniques are therefore paramount. There is physiological evidence to suggest that in the case of extra-thoracic intraluminal laryngotracheal stenosis, positive-pressure ventilation after intravenous induction is preferable to spontaneous ventilation11. The advent of Sugammadex to potentially reverse deep neuromuscular blockade in the event of failed intubation may enhance contingency planning. That said, awakening and effective spontaneous ventilation cannot be guaranteed. The use of a muscle relaxant gives the best intubating conditions and also optimum access to the neck if a “can’t intubate, can’t oxygenate” (CICO) situation develops. Careful consideration of the intubation technique should be made prior to induction of anaesthesia and may involve direct intubation, the use of videolaryngoscopy, flexible or rigid fibreoptic layngoscopy (see section on devices). Alternatively, the recently published technique of Transnasal Humidified Rapid-Insufflation Ventilator Exchange (THRIVE)12 or NO-DESAT!13 where high flow oxygen is delivered via nasal cannula may be considered in isolation or to complement oxygenation prior to intubation. This technique has many benefits however its role in the acutely obstructed airway remains unclear and it may give the clinician a false sense of security.
Awake fibreoptic intubation (AFOI)
Depending on operator expertise, equipment availability and the site and extent of airway obstruction, AFOI can be used successfully14. Its use should be considered carefully after discussion with the surgical team and following nasendoscopy. It may not be the best option if there is a potential to cause complete airway obstruction; the so-called “cork-in-bottle” situation3, for example in glottic tumours where the aperture of the airway may be greatly reduced. It may also be ill-advised if the anatomy is grossly distorted, there is a risk of bleeding, the patient would struggle to co-operate or if there is a risk of airway compromise due to either over-sedation or local anaesthetic topicalisation. AFOI in patients with an obstructed airway therefore remains controversial1. Indeed, NAP 4 reported failure of this technique in 14 of 23 head and neck cases2.
Awake tracheal access
The decision to perform an awake surgical tracheostomy under local anaesthetic depends on urgency, experience, location, and the ability to perform contingency plans1. Indications may include severe stridor, a fixed hemi-larynx, advanced tumours, gross anatomical distortion, a larynx not seen on fibreoptic nasendoscopy, or where surgical intervention will render the post-operative calibre of the airway poor1,3,15. Several cases reported to NAP 4 were criticised for failing to perform tracheostomy prior to induction of anaesthesia2. This technique may be technically very challenging depending on the underlying pathology and the ability of the patient to tolerate lying supine. A recent study described the outcome of 68 patients requiring emergent awake tracheostomy due to upper airway obstruction (85% of cases due to malignancy)16. Although 19 cases were lost to follow-up, the procedure was considered to be safe and effective in securing the airway in these patients, with long-term complications reported in only three cases (tracheitis and granuloma).
Where awake tracheostomy is not deemed necessary, elective narrow-bore needle cricothyroidotomy may be considered as an option prior to induction allowing a cannula to be left in situ. This may be used for jet ventilation in the event of failure to secure an endotracheal tube and conversion via a Seldinger technique (for example, using the Melker cricothyroidotomy set) to a wide-bore cricothyroidotomy if necessary. It is important to note the diameter of the cannula if non-standardised equipment is being used to ensure compatibility with the Seldinger set. In the CICO situation, NAP-4 warned of a significant failure rate with cannula cricothyroidotomy, and the new DAS guidelines8 recommend a surgical approach when emergency front-of-neck access is required.
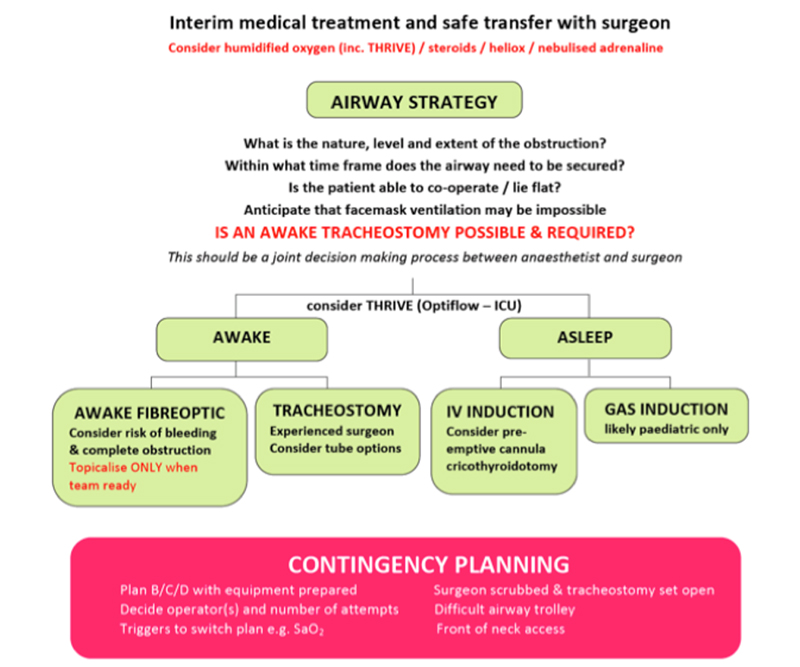
Figure 7. A cognitive aid to planning an airway strategy in an obstructed airway 17
ENDOTRACHEAL INTUBATION DEVICES
Broadly speaking, endotracheal intubation devices can be divided into four main categories. Each device has advantages and disadvantages and no single device is ideal for every difficult airway scenario9. The choice ultimately relies on the site and nature of the obstruction, device availability and operator preference and expertise.
Direct Laryngoscopy
Macintosh blade direct laryngoscopy is a well-established technique which affords the operator a wide view of the larynx and surrounding structures. A gently inserted bougie may be useful to aid intubation. Straight blade retromolar laryngoscopes may be preferred to directly elevate the epiglottis. NAP-4 recommends that multiple attempts at direct laryngoscopy in patients with head and neck pathology should be avoided as this may lead to complete airway obstruction.2 Supraglottic pathology may make access to the vallecula and therefore laryngoscopy, difficult.
Indirect Videolaryngoscopy
There are a range of videolaryngoscopes currently available and comparison of devices is ongoing. They can be divided into channeled (e.g Airtraq) and non-channelled (e.g Storz C-MAC, GlideScope). The image is transmitted from the tip of the instrument providing an indirect view of the larynx. The advantages are that the view is magnified and depending on the angulation of the blade allows an improved view. There is also the benefit that members of the operating team can see the difficulties being encountered which improves communication and team work. The role of videolaryngoscopy in the obstructing lesion is unclear as despite a good view of the larynx the operator may encounter difficulty advancing the endotracheal tube through the cords18. Indirect videolaryngoscopy has more recently been used in awake patients as the force of laryngosopy is reduced and this technique may become more popular as experience increases.19, 20.
Flexible Fibreoptic Laryngoscopy (nasal or via LMA)
Asleep fibreoptic laryngoscopy is an alternative strategy depending on the nature of the obstruction. It’s use via an LMA and passage of a pre-mounted Aintree Exchange catheter has been advocated in preference to the intubating LMA9. A case report described successful airway rescue using this technique via a ProSeal LMA in a patient with severe supraglottic swelling following carotid endarterectomy21. This technique should be rehearsed in simulation if it is the chosen plan A or back-up strategy to optimise chances of success.
Rigid Fibreoptic Laryngoscopy
Rigid optical stylets such as the Bonfils fibrescope can be advantageous when negotiating laryngeal pathology. It’s utility lies in the ability to gently push obstructing lesions to one side to enter the trachea and deploy the pre-mounted tube9. This technique requires training and should be considered carefully if there is a risk of causing bleeding and worsening obstruction.
EXTUBATION CONSIDERATIONS
NAP-4 identifies extubation and early recovery as a period of risk for patients with head and neck pathology. In these cases it is important to appreciate that the obstruction may not be effectively relieved by surgery due to residual disease, haematoma or swelling. Risk of bleeding remains a possibility and demands a high index of suspicion in the postoperative period. The report recommends that the surgical team remain immediately available at extubation until the patient is effectively managing their own airway2. Staged extubation kits are available for consideration in some patients. These contain a wire which can be placed via the endotracheal tube prior to extubation and an airway catheter which can be passed over the wire in the event of airway compromise. Its use should be discussed with the surgical team since it involves instrumentation of the airway and may risk disrupting surgical site haemostasis.
SUMMARY
Management of the obstructed airway requires careful assessment, planning and execution to optimise success. Involvement of the multidisciplinary team at an early stage is recommended. The NAP-4 report has significantly impacted our approach to safely managing these cases (Figure 8). In particular it identifies potential pitfalls to be wary of and the need for detailed contingency planning with a multidisciplinary approach.
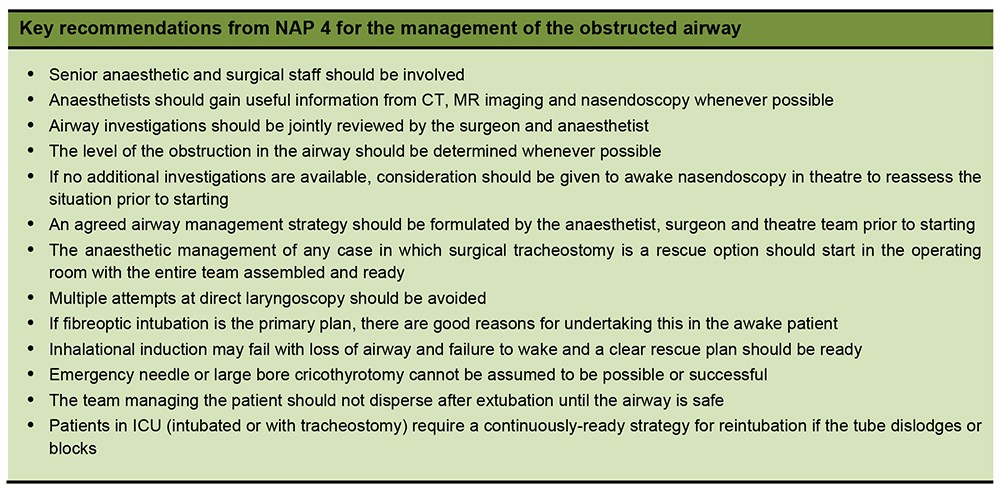
Figure 8. Summary table of recommendations from NAP 42
ANSWERS TO QUESTIONS
- A 69-year old woman presents to the emergency department with a 3-day history of worsening stridor. A mobile lesion obstructing 70% of the glottis is seen on fibreoptic nasal endoscopy
a. True. Immediate medical management involves maximizing oxygenation of the spontaneously breathing patients. Nebulised adrenaline may improve airflow by causing bronchodilation and IV steroids may reduce oedema.
b. False. Transfer to theatre will need to be done with experienced staff who have advanced airway skills along with appropriate equipment in case the patients deteriorates during the transfer.
c. False. Induction in patients with a compromised airway should ideally be done in theatre with all members of the anaesthetic and surgical team present in case the patient deteriorates and needs front of neck access. This was highlighted in NAP4.
d. False. In a patient with worsening stridor and a glottic lesion, face mask ventilation may be difficult as following general anaesthesia loss of airway tone may result in the glottic lesion completely obstructing the airway
e. True. This may be useful in case emergency front of neck access is necessary. - The following statements are correct with regard to endotracheal intubation
a. False. Access to the vallecula may be impossible with a base of tongue tumour making direct laryngoscopy difficult.
b. True. Videolaryngoscopy may give an improved view of the glottis however tube advancement may still be difficult as a good indirect view does not necessarily correspond with ease of intubation.
c. True. Awake fibreoptic intubation may result in the “cork in bottle’ effect where a partially obstructed airway becomes completely obstructed.
d. True. THRIVE can be used to optimise apnoeic oxygenation when the airway is being instrumented.
e. False. NAP 4 found that repeated attempts at laryngoscopy and intubation often resulted in airway oedema and deterioration from a difficult airway to a compromised airway - Regarding induction of anaesthesia
a. False. Inhalational induction, although still used in children, can result in complete obstruction of the airway in adults as gas flow across the obstruction is limited. This results in less anaesthetic being delivered and potentially suboptimal intubating conditions
b. True. Elective narrow-bore needle cricothyroidotomy may be considered prior to induction as a rescue technique if intubation is difficult.
c. True. In a hypoxic patient who is struggling to maintain adequate gas exchange an awake tracheostomy may be difficult due to compliance and difficulty in positioning
d. False. Although Sugammadex may mean that muscle relaxants can be reversed quickly an awake technique may be the preferred option in the compromised airway.
e. False. Human factors are as important as technical expertise. NAP 4 found that there were numerous examples where human factors contributed to a poor outcome.
REFERENCES AND FURTHER READING
- Patel A and Pierce A. Progress in management of the obstructed airway. Anaesthesia 2011, 66(suppl 2) 93-100
- Cook TM, Woodall N, Frerk c. Major Complications of Airway Management in the United Kingdom: Report and Findings 4th National Audit of the Royal College of Anaesthetists and the Difficult Airway Society. London: National Patient Safety Agency, 2011
- Rees L and Mason RA. Advanced upper airway obstruction in ENT surgery. BJA CEPD Reviews 2002 vol 2 (5) 134-8
- Society for Head and Neck Anaesthesia. Round table discussion: the management of patients with the partially obstructed airway. www.shanahq.com 2013, accessed November 2015.
- Slinger P and Karsli C. Management of the patient with a large anterior mediastinal mass: recurring myths. Current opinion in anaesthesiology 2007, 20 (1) 1-3
- Dinsmore J, Heard AM and Green RJ. The use of ultrasound to guide time-critical cannula tracheotomy when anterior neck airway anatomy is unidentifiable. Eur J Anaesthesiol. 2011 Jul;28(7):506-10
- Gleeson S, Groom P and Mercer S. Human factors in complex airway management. BJA Education 2015, 1-7
- Frerk C, Mitchell VS, McNarry AF et al. Difficult Aiway Society 2015 guidelines for the management of unanticipated difficult intubation in adults. BJA 2015, 115 (6): 827-48
- The Aintree Difficult Airway Management website. Available from http://adam.liv.ac.uk/adam8/login.aspx
- Pinnock C, Lin T and Smith T. Fundementals of Anaesthesia, second edition 2003, Greenwich Medical Media Limited
- Nouraei SA, Giussani DA, Howard DJ et al. Physiological comparison of spontaneous and positive-pressure ventilation in laryngotracheal stenosis. Br J Anaesth. 2008 Sep;101(3):419-23
- Patel A, Nouraei SA. Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia. 2015 Mar;70(3):323-9
- Levitan R. NO-DESAT! (nasal oxygen during efforts securing a tube). epmonthly.com/article/nodesat. accessed February 2016
- Leslie D, Stacey M. Awake intubation. BJA CEACCP 2015, 15 (2); 64-7
- English J, Norris A, Bedford N. Anaesthesia for airway surgery. BJA CEACCP 2006, 6 (1); 28-31
- Fang CH, Friedman R1, White PE et al. Emergent Awake tracheostomy–The five-year experience at an urban tertiary care center. Laryngoscope. 2015; 125(11):2476-9
- Bryant H, Frampton S, Dinsmore J, Turner M. A cognitive aid to planning an airway strategy in an obstructed airway. Portsmouth anaesthetic department.
- Batuwitage B, McDonald A, Nishikawa K, Lythgoe D, Mercer S, Charters P. Comparison between bougies and stylets for simulated tracheal intubation with the C-MAC D-blade videolaryngoscope. Eur J Anaesthesiol. 2015 Jun;32(6):400-5
- Kramer A, Müller D, Pförtner R et al. Fibreoptic vs videolaryngoscopic (C-MAC® D-BLADE) nasal awake intubation under local anaesthesia. Anaesthesia 2015; 70: 400-6.
- Fitzgerald E, Hodzovic I, Smith AF. ‘From darkness into light’: time to make awake intubation with videolaryngoscopy the primary technique for an anticipated difficult airway? Anaesthesia. 2015 Apr;70(4):387-92
- Cook TM, Silsby J, Simpson TP. Airway rescue in acute upper airway obstruction using a ProSeal Laryngeal mask airway and an Aintree catheter: a review of the ProSeal Laryngeal mask airway in the management of the difficult airway. Anaesthesia. 2005 Nov;60(11):1129-36.



