Intensive Care Medicine
QUESTIONS:
Before continuing try to answer the following questions. The answers can be found at the end of the article.
- The following antibacterial agents infer with protein synthesis
- Amoxycillin
- Erythromycin
- Tetracycline
- Trimethoprin
- Penicillin
- Cefuroxime is
- Bacteriostatic
- Active against gram positive organisms only
- Contain a beta lactam ring
- Active against Methacillin Resistant Staph Aureous (MRSA)
- Is resistant to stomach acid
- The Aminoglycoside antibiotics
- Are well absorbed from the GI tract
- Are toxic to the liver
- Shorten the duration of neuromuscular blocking drugs
- May cause deafness
- Affect bacterial wall formation
INTRODUCTION
Antibacterial and Antiviral drugs includes the antibiotics, which are drugs produced by micro-organisms, and chemotherapeutic agents which are chemically synthesised. Antibacterial drugs may be used to treat infection, or may be given prophylactically to prevent the development of infection. This latter use is common in some forms of surgery and anaesthetists are often responsible for the administration of prophylactic antibiotics. Therefore it is important to understand their pharmacology and the nature of any interactions with other drugs used in anaesthesia.
Antibacterial drugs bring about their action by one of two mechanisms. They can limit bacterial growth bacteriostatic effect, slowing growth and allowing the immune system to remove the bacteria from the body. Alternatively they cause bacterial death and are bacteriocidal. The principal being that host cells are undamaged by the drug. With antiviral drugs the virus replicates with in the host cells, so drugs are required to selectively inhibit the metabolic processes specific to viral replication. This can only be achieved to a limited extent.
ANTIBACTERIAL DRUGS MECHANISMS OF ACTION
Inhibitors of cell wall synthesis.
These drugs act on bacteria that have a cell wall consisting of a lattice work of murein. They prevent the cross linkage of the molecules that make up the lattice. Mammalian cells do not have these rigid cell walls so are unaffected.
Drugs in this group include:
The Penicillins
This is the oldest group of drugs, obtained from a mould, penicillium notatum. They inhibit the enzyme transpeptidase which forms the lattice cross links. Their action is bacteriosidal, because defects in the murein wall allows the bacteria to swell and burst. The penicillin molecule contains a beta-lactam ring, which confers its anti transpeptidase activity. In this original form it has a narrow antibacterial spectrum, confined to gram-positive bacteria, gram negative cocci and spirochetes. Many gram negative bacteria are unaffected by penicillin
Some bacterial produce penicillinase which cleaves the beta lactam ring and confers penicillin resistance on the organism.
Penicillins are well tolerated, but at high doses are neurotoxic and convulsions may be seen with sudden high concentrations in the brain. This is due to GABA antagonism and can occur after intrathecal or high dose intravenous administration.
Chemical manipulation of the penicillin molecule to give better bioavailability, penicllinase resistance and a wider spectrum has been performed.
Flucloxacillin is penicillinase resistant and orally absorbed.
The aminopenicillin amoxicillin has a wider spectrum being active against many gram negative organisms, it is combined with clavulanic acid which prevents the action of penicillinase.
Carboxypenicillins such as carbicillin, ticacillin, and acylaminopenicillins such as mezclocillin azlocillin and piperacillin have a very broad spectrum but are not acid stable, or penicillinase resistant.
They are active against Pseudomonas species.
Cephalosporins
These drugs also come from fungi and contain the beta lactam group in their molecules. These are classified in generations, the earliest first generation cephalosporin was cephalexin, which is a wide spectrum oral cephalosporin with a spectrum of activity largely in gram positive bacteria. It is bacteriosidal. The subsequent developments have been to produce wider spectrum of activity. The second generation includes cefuroxime wich has a broader spectrum including many gram negative species. Resistance to second generation cephalosporins is increasing. The 4th generation consists of one drug cefepime, which is active against Pseudomonus aeroginosa the 5th generation soon to be launched called ceftobiprol is active agains Methacillin resistant Staph Aureus. (MRSA)
Vancomycin
This drug is a glycopeptide structurally unlike any other antibacterial drug. It inhibits cell wall production but also affect cell synthesis.it is highly polar and not absorbed from the gut as a result it has been used to treat pseudomembranous enteroclitis caused by clostridium difficile. Reistance to this drug appears to be stable.
Inhibitors of Tetrahydrofolate Synthesis
Trimethoprin and Co-trimoxazole
These two drugs inhibit the conversion of dihydrofolate to Tetrahydrofolic acid by blocking dihydrofolate reducatase. Tetrahydrofolic acid is a co-enzyme in the synthesis of purine bases and thmidine. These are required for the synthesis of DNA and RNA. The effect is to limit cell growth. They are therefore basteriostatic.
Trimethoprin has a selectivity for bacterial dihrdrofolate reductase, but can affect human folate metabolism and rarely causes bone marrow depression. It is usually combined with a sulphonamide sulfamethoxazole, which also affects folate metabolism but at a different step in the pathway. The combined preparation is more effective than either alone, and example of pharmacological synergy.
Resistance to these drugs is rare.
Dapsone, acts by the same mechanism and is used prophylactically and as chemotherapeutic agent in leprosy, toxoplasmosis and acinomycosis.
Inhibitors of DNA function
Metronidazole and Rifampicin
Metronidazole damages DNA by complex formation with the DNA molecule and strand breakage. In anerobic organisms it is converted to a reactive metabolite which attacks the DNA. It bacteriocidal and also anti protozoal and anti amoebic. The drug is potentially mutagenic and tetratogenic and should be avoided in pregnancy and lactation.
Rifampin prevents RNA transcription and is bactericidal against mycobacteria species as well as gram positive and gram negative organisms. Resistance develops and it is reserved for the treatment of TB and leprosy.
Inhibitors of Protein Synthesis
Tetracyclines, Aminoglycosides, chloramphenicol and erythromycin.
Tetracyclines and aminoglycoside drugs both alter transcription of RNA and creation of proteins. They bind to ribosomes and prevent the initiation of protein synthesis. Tetracyclines are broad spectrum and bacteriostatic. The aminoglycosides induce the production of ‘false proteins’ and are bacteriocidal. They are active against gram negative orgamisms. Gentamycin is not active against anaerobes because oxygen is needed for its uptake into the bacterial cell. It is synergistic with the beta lactam containing antibiotics. The aminoglycosides are taken up in the tubular cells of the kidney and can cause renal tubular damage. They are also concentrated in the endolymph of the inner ear and can cause damage to the 8th cranial nerve. The toxic effects are associated with high peaks of serum concentration. Gentamicin levels may need to be monitored in renal impairment. If bolus doses are given they should be injected slowly over 5 minutes to prevent the peak concnetraion rising into the toxic range.
Chloramphenicol inhibits peptide sythetase, it has a bacteriostatic effect. It is toxic to bone marrow, particularly in babies. It is used in bacterial meningitis.
Erythromycin inhibits transfer RNA preventing the assembly of proteins. It is active against gram positives but most gram negative organisms are resistant to it. Clarithromycin is a derivative with better acid resistance and bioavailability, clindomycin is a semisynthetic analogue that is well absorbed orally. These drugs are bacteristatic.
Interactions between antibiotic drugs and anaesthetic agents.
Interactions can be pharmacokinetic or pharmacodynamic. Many antibacterial agents are highly protein bound and will displace other drugs, thereby affecting their toxicity and metabolism. Drugs which suppress synthesis of protein can affect the metabolism of other drugs.
Classically gentamicin and the other aminoglycoside antibiotics prolong the duration of action of muscle relaxant drugs. They may also worsen symptoms in myasthenia gravis.
ANTIVIRAL DRUGS MECHANISMS OF ACTION
In the last ten years the number of available antiviral drugs has increased from 5 to nearly 40.
The mechanism of action of these drugs is aimed at various targets in the viral replication process.
To replicate the virus needs to
- Enter the cell and separate from its protein coat
- Interact with the cell DNA and produce viral RNA
- Trascript the viral RNA into viral proteins and new DNA.
- Assemble the viral DNA and proteins into new viral particles
RNA viruses are simpler entities and need only replicate their own RNA and proteins for the outer coat.
The major target of these drugs is an enzyme called reverse transcriptase, which is involved in the synthesis of new viral molecules. The assembly of the viral particles requires a protease to cut larger protein molecules into the smaller molecules that make up the coat.
The three main classes of drugs used in the management of Human Immunodeficiency Virus infection are:
- The Nucleoside Reverse Transcriptase Inhibitors (NRTI)
- The Nucleotide Reverse Transcriptase Inhibitors (NtRTI)
- The Non Nucleoside Reverse Transcriptase Inhibitors (NNRTI)
They are usually used in combination therapy to reduce the incidence of viral resistance.
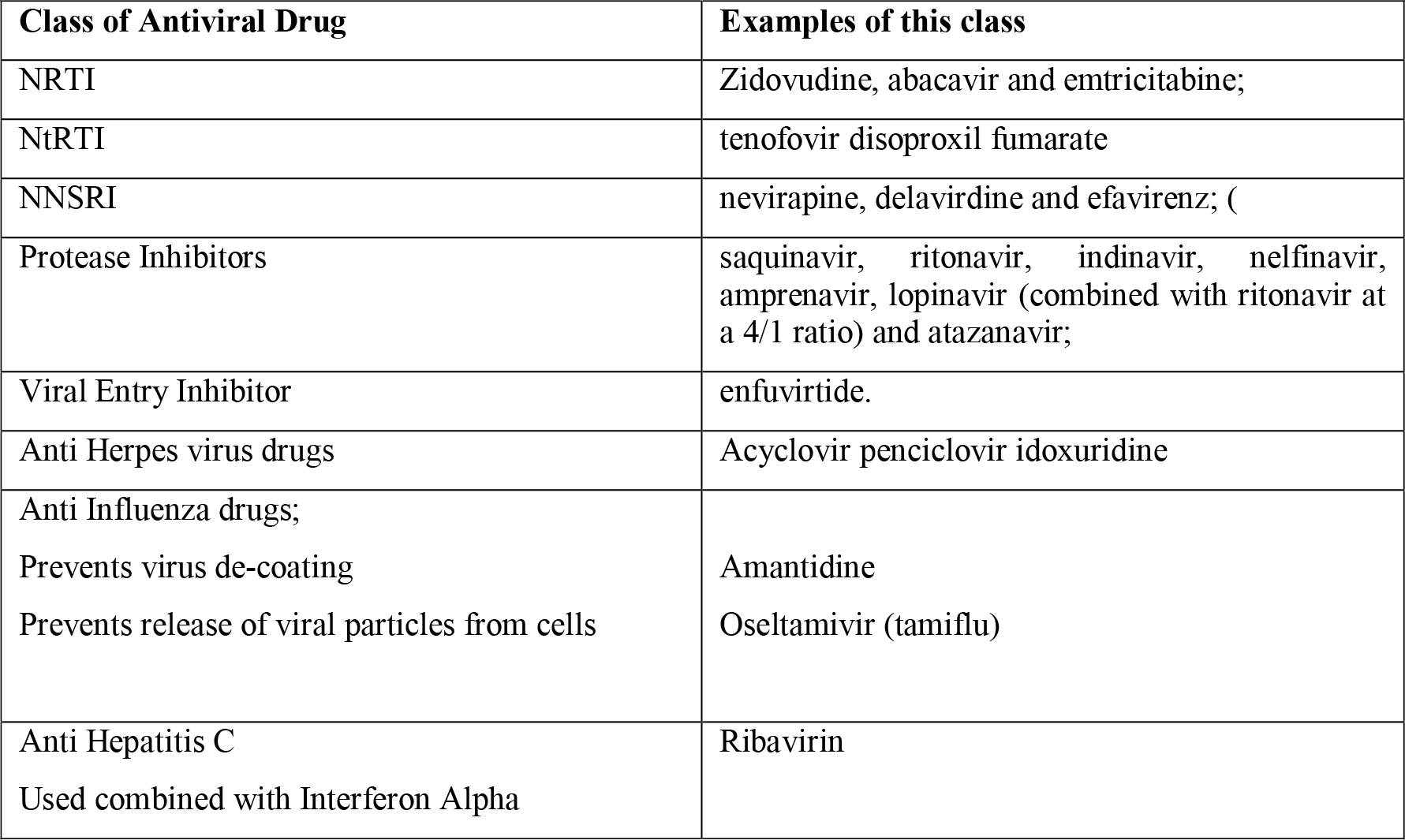
Table 1. Classification of antiviral drugs
All these drugs are toxic, with particular risks of liver and renal toxicity. In any patient presenting for anaesthesia on these drugs liver and renal Impairment should be considered.
There is evidence that Zivodudine does not interact with paracetamol, or non steroidal anti inflammatory drugs, and is also safe with codeine. There have been no other formal drug interaction studies with these drugs. The majority of the antiviral drugs require an acidic medium in the stomach for effective absorption. Patients give at acids or proton pump inhibitors as acid aspiration prophylaxisis should not take antivirals after they have received this therapy, but wait until after anaesthesia has been safely performed.
ANSWERS TO QUESTIONS
- FTFTF
- FFTFF
- FFFTF
WEBLINKS
The Merk Manuals On Line Library covers a n enormous range of pharmacology and is always worth a look!
REFERENCES and FURTHER READING
- Pharmacology for Anaesthesia and Intensive Care, Peck, Hill, Williams, Cambridge University Press.
- Antiviral Drugs in current clinical use, De Clercq E, Journal of Clinical Virology 30;2; 115-113 June 2004.



