QUESTIONS
Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation.
- Delayed surgery for neck of femur fractures (NOFs) beyond what period of time is associated with increased mortality and morbidity?
a. 10 hours
b. 24 hours
c. 48 hours
d. 72 hours - Which of the following do the 2011 Association of Anaesthetists of Great Britain and Ireland (AAGBI) guidelines consider to be an unacceptable reason for delaying surgery?
a. Haemoglobin concentration less than 8 g/ dL
b. Uncontrolled diabetes
c. Chest infection with sepsis
d. Lack of facilities or theatre space - On examination of a patient with a NOF fracture, you have discovered a heart murmur. In this case, the 2011 AAGBI guidelines recommend a preoperative echocardiogram is indicated if:
a. Patient has a previous history of ischaemic heart disease
b. Patient is breathless at rest or on low level exertion
c. Patient has never had an echocardiogram before.
d. Patient has an abnormal ECG
INTRODUCTION
Several large systematic reviews of neck of femur fracture (NOF) surgery have demonstrated that operative delays beyond 48 hours results in increased morbidity and mortality1-3. Surgery beyond the 48-hour period has been shown to more than double the risk of postoperative complications such as pneumonia, urinary tract infections, deep vein thrombosis and pulmonary embolism4, whilst earlier surgery results in reduced mortality and postoperative complications5.
Reasons for operative delay can be grouped into system-based or medical-based delays. System-related delays include waiting for routine medical consultations or the unavailability of operating rooms or surgeons. Medical delays include stabilisation of medical problems such as unstable blood sugar levels in diabetic patients or reversing anticoagulation.
Timely surgery for NOFs presents a challenge for healthcare systems as it involves large numbers of elderly patients with significant comorbidities. To manage this complexity, a protocol-driven and multidisciplinary approach is ideal. This tutorial is largely based on the recently released Association of Anaesthetists of Great Britain and Ireland (AAGBI) guidelines regarding NOF surgery. They are unique because they are specifically directed towards helping anaesthetists manage patients with hip fracture.
FACILITIES AND SERVICES REQUIRED
Multidisciplinary management
A multidisciplinary group could contain trauma co-ordinators, general practitioners, community nurses, emergency staff, bed managers, orthopaedic nursing staff and surgeons, anaesthetists, orthogeriatricians, physiotherapists, occupational therapists, social workers, rehabilitation services and trauma coordinators.
Planned care pathways
Patients with a hip fracture who arrive in the emergency department should have a planned care pathway which includes prioritised anaesthetist and orthopaedic reviews as well as instructions on the management of pre-operative issues such as fasting and anticoagulation. The pathway should also include prompt notification of bed managers and trauma coordinators to reduce chances of delay.
Trauma coordinators
Trauma coordinators can reduce pre-operative delays, facilitate interdisciplinary communication and start discharge planning. Together with mulidisciplinary trauma meetings in the morning before the start of operating lists, they can effectively reduce delays.
Protected trauma lists
These are separate from general emergency lists and should be provided daily. The AAGBI recommends that hip fracture surgery should be prioritised unless in the cases of life or limb-threatening trauma.
Consultant-delivered service
The AAGBI recommends that patients with hip fracture be ideally anaesthetised and operated on by consultants with clinical experience in treating the unwell, older patient in order to reduce operative time and poor surgical outcomes.
Operating department
Room temperature should be between 20 to 23 °C with a humidity of 50-60%. A dedicated radiographer will help reduce delay. An adequate stock of surgical implants, consumables and instruments should also be prepared.
PRE-OPERATIVE MANAGEMENT
Analgesia
Surgical fixation is the best analgesic in hip fractures. Start with simple analgesics such as paracetamol and progress to opioids only after urea and electrolytes have been checked. Regional analgesia using nerve blocks offers effective pre-operative pain relief and reduces the risk of opioid-induced side effects.
Pre-operative assessment
Seventy percent of patients with a NOF will have an ASA score of 3-4, making pre-operative assessment by an anaesthetist mandatory9. Thirty five percent will have one comorbidity, 17% will have two and 7% will have three or more10. The most common comorbidities are cardiovascular disease (35%), respiratory disease (14%), cerebrovascular disease (13%), diabetes (9%), malignancy (8%) and renal disease (3%)10. The anaesthetic assessment allows for planning of anaesthetic technique, assessment and communication of peri-operative risk, and pre-optimisation.
Early input from orthogeriatricans is also recommended. Orthogeriatric input can identify patients at increased risk of peri-operative morbidity and mortality, help optimise patients before surgery and facilitate the commencement of early rehabilitation and discharge planning.
Routine pre-operative investigations
Full blood count and group & hold
Pre-operative anaemia is present in 40% of patients. The AAGBI suggest the use of a higher blood transfusion trigger in the elderly, such that in the case of Hb < 90g/L (or Hb < 100g/L with a history of ischaemic heart disease), two units of blood should be transfused.
Leukocytosis and neutrophilia are common and may present a reaction to trauma rather than infection. A platelet count of less than 80 x 109/L is a relative contraindication to neuraxial anaesthesia. Platelet count less than 50 x 109/L will usually need a platelet transfusion.
Urea and electrolytes
Hyper- and hypokalemia, as well as hyponatraemia are common.
Coagulation studies
Request coagulation tests only if clinically required.
Electrocardiogram (ECG)
ECG is required in all patients with a NOF.
Chest X-ray (CXR)
CXR is not necessary for all patients but may be useful in those with pneumonia or heart failure.
Atrial fibrillation (AF)
Patients in AF should ideally have a ventricular rate less than 100 beats per minute. Exacerbants such as electrolyte abnormalities or sepsis should be treated.
Anticoagulation
Aspirin should be withheld during inpatient stay unless indicated for unstable angina or stroke.
Those on clopidogrel should not have their surgery delayed or have prophylactic platelets. The AAGBI suggests generally not stopping clopidogrel on admission especially in patients with drug eluting stents. This suggestion may differ to the practice at your hospital. Hence, an individual approach balancing the risks of interrupting clopidogrel therapy will need to be tailored to each patient.
Hospital guidelines regarding the peri-operative management of warfarin should be followed. Aim for an International Normalised Ratio (INR) of less than 2 for surgery and less than 1.5 for neuraxial anaesthesia. Use vitamin K or prothrombinex to reverse warfarin if necessary. Peri-operative cover with heparin is usually required. Warfarin should be recommenced 24 hours after surgery.
If unsure about the management of anticoagulation, haematologist advice should be sought promptly.
Chest infection
Chest infections require prompt antibiotics and the AAGBI recommend proceeding to surgery under regional anaesthesia if possible.
Diabetes
Hyperglycaemia is not a reason to delay surgery unless the patient is ketotic and/or dehydrated. Hospital guidelines concerning the peri-operative management of diabetes should be followed.
Heart murmur
There is debate regarding the postponement of surgery pending echocardiography in light of unrecognised aortic stenosis. The majority of clinicians favour proceeding to surgery with modificatiton of their techniques toward general anaesthesia and invasive blood pressure monitoring.
Echocardiography may be indicated in order to:
- Establish left ventricular function if the patient is breathless at rest or on low level exertion
- To investigate severity of an ejection systolic murmur heart in the aortic area, particularly if two or more of the following are present:
a. Unexplained syncope or pre-syncope
b. Slow rising pulse
c. Absent second heart sound
d. Left ventricular hypertrophy on ECG without hypertension
Implantable cardioverter defibrillators (ICD) and pacemakers
With both devices there are risks of perioperative failure and of unipolar diathermy resulting in delivery of an arrhythmogenic shock to the myocardium. The AAGBI recommend early consultation with a cardiologist to identify the specific type of device and to develop a plan for intra-operative management.
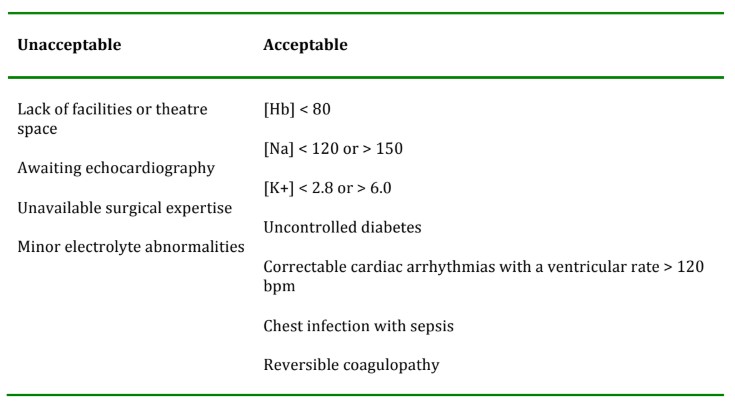
Table 1. Acceptable and unacceptable reasons for delaying surgery in hip fractures.
INTRA-OPERATIVE MANAGEMENT
Anaesthetic choice
There is little evidence to support the use of one anaesthetic technique over another for patients undergoing hip fracture surgery. Anaesthetists tend to use the technique that they are familiar with. Approximately half of anaesthetists use neuraxial anaesthesia and the rest use general anaesthesia. The AAGBI recommends that peripheral nerve blockade always be considered whether a spinal or general anaesthesia is used.
Neuraxial anaesthesia
The AAGBI recommends the use of either spinal or general anaesthesia but not a combination of the two as the latter is associated with falls and hypotension. Lower doses of intrathecal bupivacaine (<10mg) may reduce associated hypotension. Intrathecal fentanyl is preferred to morphine as it is associated with less respiratory and cognitive depression.
General anaesthesia
It is recommended that reduced doses of intravenous induction agents be administered. Inhalational induction is generally well tolerated by the elderly and may facilitate a haemodynamically stable induction. There remains debate about whether mechanical ventilation is preferrable to spontaneous.
Peripheral nerve blockade
Peripheral nerve blockade can reduce post-operative analgesia requirements. Blockade of the femoral, obturator and lateral cutaneous nerve of the thigh can provide adequate analgesia. The psoas compartment block / lumbar plexus block is the most reliable method of blocking all three. Femoral nerve blocks do not reliably block all three nerves but can reduce postoperative analgesia requirements and be more easily placed with ultrasound guidance. The facsia iliaca block is an alternative technique, which covers all three nerves and requires a similar level of skill to the femoral nerve block.
Monitoring
Have a low threshold for obtaining further monitoring equipment for this patient group.
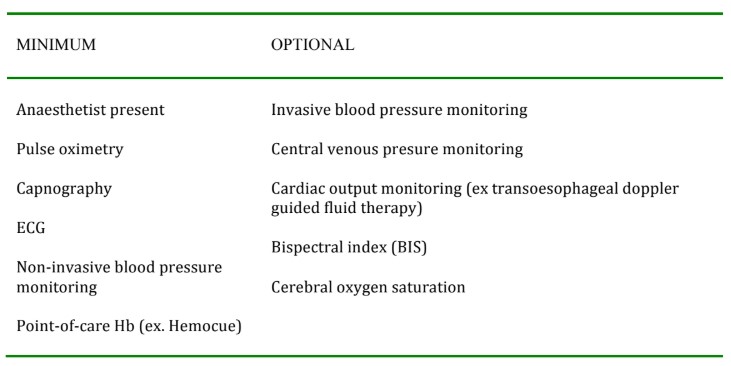
Table 2. Minimum and optional monitoring.
Supplemental pain relief
Opioids and non-steroidal anti-inflammatory drugs should be used with caution. Codeine should not be used because its variable pharmacokinetics make its efficacy and safety difficult to predict in an individual7. Paracetamol should be given in the perioperative perioid.
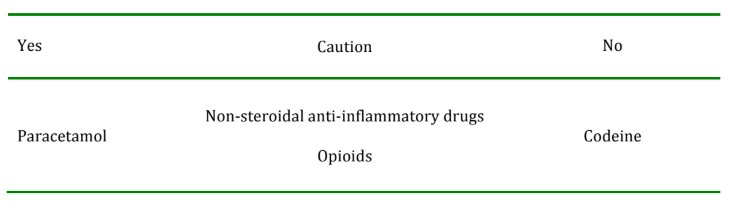
Table 3. AAGBI recommendations for supplemental pain relief
Thromboprophylaxis
Patients should have low molecular weight heparin administered the evening prior to daytime trauma lists. This precaution allows for an appropriate window of time to minimise the risk of bleeding related to neuraxial anaestheisa. Thromboprophylactic stockings or intermittent calf compressors should be used intraoperatively. Regional anaesthesia, prompt surgery and early mobilisation will also reduce the risk of deep vein thrombosis.
Antibiotics
Administer within one hour prior to skin incision. Follow your hospital’s antibiotic protocols.
Pressure care
Elderly patients should be positioned to avoid pressure sores if possible.
Thermoregulation
Active warming techniques should be used as elderly patients are prone to intra-operative hypothermia.
Intravenous fluids
Many patients are hypovolaemic from fasting prior to their surgery. Preoperative intravenous fluids should be prescribed.
POST-OPERATIVE MANAGEMENT
Nursing
These patients should ideally be in a ward with a nurse to patient ratio of 1:4.
Analgesia
As the peripheral nerve blockade wears off, administer paracetamol regulary with carefully prescribed opioid analgesia as required.
Hypoxia
Supplemental oxygen should be provided in the first 24 hours after the operation. Early mobilisation will improve oxygenation and respiratory function.
Fluid balance
Hypovolaemia is common post operatively and oral fluid intake should be encouraged over the intravenous route.
Urinary tract infections (UTI)
UTI’s are common and urinary catheters should be removed as soon as possible to reduce the risk of infection. Early mobilisation will also reduce the risk of UTI’s.
Postoperative confusion
Cognitive dysfunction or an acute confusional state occurs in 25% of patients with hip fracture. This can interrupt management and rehabilitation. Physicians specalised in the care of the elderly should be involved. Haloperidol or lorazepam should be used as only short-term symptom control. An underlying cause of the acute confusion should be sought and treated.
Malnutrition
Many patients with hip fracture are malnourished on admission to hospital. Dietitians should be inolved and nutritional supplements should be provided.
Rehabilitation
Rehabiltation aims to return the patient to their pre-morbid level of activity. Rehabilitation should start as early as possible and be co-ordinated with an orthogeriatrican.
IMPORTANT POINTS
- Surgical repair of hip fractures should occur within 48 hours of hospital admission
- Surgery is the best analgesia for a hip fracture
- The value of investigations need to be carefully weighed against the risk of delaying surgery further
- Patients with hip fracture require multidisciplinary care
- Audit projects are required for quality improvement
ANSWERS TO QUESTIONS
- C
- D
- B
WEBLINKS
- Sample patient information sheets regarding hip fractures which can be modified to suit your specific hospital: http://docroncheung.blogspot.com.au/2013/04/sample-patient-information-leaflets-on.html
- Information and tutorial on the fascia iliaca block: http://neuraxiom.com/fascia_iliaca_block.html
REFERENCES and FURTHER READING
- Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth 2008; 55:146-154.
- Khan SK, Kalra S, Khanna A et al. Timing of surgery for hip fractures: a systematic review of 52 published studies involving 291,413 patients. Injury 2009; 40: 692-7.
- Moja L, Piatti A, Pecoraro V, Ricci C, Virgili G, Salanti G et al. Time matters in hip fracture surgery: patients operated within 48 hours have better outcomes. A meta-analysis and meta-regression of over 190,000 patients. PLoS ONE 2012; 7(10): e46175.
- Sircar P, Godkar D, Mahgerefteh S, et al. Morbidity and mortality among patients with hip fractuers surgically repaired within and after 48 hours. Am J Ther 2007; 14:508-513.
- Simunovic N, Devereaux PJ, Sprague S, Guyatt GH, Schemitsch E, Debeer J, Bhandari M. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ 2010 Oct 19;182(15):1609-16.
- Griffiths R, Alper J, Beckingsale A, Goldhill D, Heyburn G, Holloway J et al. AAGBI Guidelines: Management of proximal femoral fractures 2011. Anaesthesia 2012; 67, 85-98.
- Iedema, J. Cautions with Codeine. Aust Prescr 2011;34:133-5.
- Gurkan I, Wenz JF. Perioperative infection control: an update for patient safety in orthopedic surgery. Orthopedics 2006; 29 (4)
- The National Hip Fracture Database. National Report, 2010. http://www.rcseng.ac.uk/news/docs/NHFD%20(final).pdf
- Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. British Medical Journal 2005; 331: 1374-9.



