General Topics
QUESTIONS
Before continuing to read this ATOTW, try the following questions.
- Which of the following neurosurgical pathologies are more common in pregnancy?
a. Bleeding from arteriovenous malformations
b. Gliomas
c. Pituitary tumours
d. Bleeding from intra-cerebral aneurysms
e. Meningiomas - Pregnancy is normally associated with:
a. An increase in intracranial pressure
b. A normal PaCO2 of 30-32 mmHg
c. A reduction in factors II, V and X.
d. Decreased renal excretion of bicarbonate.
e. Reduced platelet count. - Regarding pharmacology in pregnancy:
a. MAC values are 10% greater.
b. Phenytoin dose may need to be increased.
c. Gastrointestinal absorption of drugs is increased.
d. Larger doses of induction agents are required due to bigger volumes of distribution.
e. Pseudocholinesterase levels are reduced. - Regarding the conduct of anaesthesia:
a. 15 degrees left lateral tilt should be applied from 24 weeks gestation to prevent aortocaval compression
b. Ephedrine is the vasopressor of choice.
c. Fetal heart rate monitoring is a useful predictor of fetal wellbeing from 20 weeks gestation.
d. Hyperventilation to manipulate PaCO2 and cerebral vascular tone should be within limits of 25-30 mmHg.
e. Esmolol is an effective way to reduce pressor responses to laryngoscopy with no impact on fetal wellbeing.
INTRODUCTION
Until 2006 in the UK, non-obstetric causes of maternal mortality and morbidity have been increasing [1]. The latest Confidential Enquiry report (2006-08) however, demonstrates a reduction in maternal mortality related to non-obstetric aetiologies. Pathology of the central nervous system (CNS) remains a leading cause of indirect maternal mortality although the incidence is relatively constant at 30-40 deaths per triennium [1]. Although rare, women may present with pathology requiring neurosurgical intervention. Neuro-anaesthesia may therefore be indicated for procedures such as intracranial surgery, spinal surgery and diagnostic and therapeutic interventions.
WHY DO WOMEN PRESENT FOR NEUROSUGERY?
Intracranial Haemorrhage
Intracerebral haemorrhage accounted for five deaths and sub-arachnoid haemorrhage (SAH) six deaths in the last Confidential Enquiry report [1]. SAH occurs in 10-20:100 000 pregnancies with devastating consequences, some reports quoting maternal mortality rates between 35-83% [2] Presentation is the same as in the nonpregnant population with sudden onset severe headache (97% of cases), often accompanied with preceding sentinel headaches in the previous weeks. There is a spectrum of subsequent neurological sequelae ranging from, isolated cranial nerve lesions, to a rapid reduction in Glasgow Coma Scale (GCS) and unconsciousness. Most SAHs are thought to occur due to intracranial aneurysms (ICAs). Rupture of ICAs is believed to occur with a higher incidence during pregnancy [2]. In addition, the risk of aneurysmal rupture rises each trimester, from 6% in the first trimester to 55% by the third [3]. Ninety per-cent occur during pregnancy but only 2% during labour and delivery [2].
Arteriovenous malformations (AVMs) are not more prevalent during pregnancy. Unlike intra-cerebral aneurysms, AVMs have the highest associated risk of bleeding in the second trimester when changes in cardiovascular status are at a maximum. Should bleeding result, there is an increased risk of re-bleeding (25%) during the same pregnancy, compared with re-bleeding during the same year in non-pregnant women (3-5%) [4]. As such, treatment targets are in the prevention of re-bleeding, either by embolisation, surgery or stereotactic radiosurgery.
Trauma
Trauma is another leading cause of incidental death during pregnancy. Trauma in itself complicates 6-7% of pregnancies [5,6] and may well involve cranial or spinal injury that will necessitate surgery. The parturient involved in a multi-trauma will present significant clinical challenges in the care of mother and fetus. The emphasis is on maternal resuscitation and in life-threatening multi-trauma, Caesarean section may be performed to improve maternal haemodynamics. Fetal compromise may also be the result of maternal hypoxia, hypovolaemia, acidosis, acute blood loss, infection or as a result of drugs used during the resuscitation process.
Primary Central Nervous System Tumours
There is no increased risk of developing primary central nervous system tumors during pregnancy and the incidence is around 6 per 100 000 pregnancies [4]. Some tumours such as meningiomas may express oestrogen or progesterone receptors and as such rapidly increase in size in the pregnant state. Previously asymptomatic and undiagnosed tumours, therefore, may become symptomatic due to an increase in size. In addition, immunological tolerance and haemodynamic changes may also result in tumours becoming symptomatic in the pregnant state. Choriocarcinoma is an aggressive gestational tumour that metastasizes to the brain. Presentation is variable and may include focal neurological defects, seizures or signs of raised intracranial pressure. The pituitary gland undergoes cellular hyperplasia during pregnancy but pituitary tumours are not more common. In addition, the endocrine aberrations resulting from pituitary tumours often result in infertility, and tumour resection is often performed pre-conception. Certain pituitary tumours, however, may warrant surgical resection during pregnancy. These are typically those associated with excessive andrenocorticotropic hormone or thyroid stimulating hormone.
Spinal Pathology
Symptomatic disc herniation is reported to have an incidence of around 1:10 000 pregnancies [7]. Hormonal changes including increased concentrations of relaxin and altered body posture are argued to exacerbate previous spinal problems but there is no increased risk of de novo disc herniation in the pregnant group [7]. It is also important to note that in those with symptomatic disc herniation due to nerve root compression, 85% of patients will get better with conservative management within 6 weeks [8]. In contrast, women presenting with worsening neurological deficit may require surgical intervention and those with a cauda equina syndrome represent a surgical emergency.
In addition to disc herniation, parturients may present for surgery as a result of newly symptomatic spinal tumours or more rare complications such as vertebral canal haematoma (either spontaneous or following neuraxial procedures), vertebral canal abscess or for vascular malformations.
Ventriculoperitoneal Shunt Revision
Pregnancy is associated with an increased rate of VP shunt complications [8]. This is thought to be due to a combination of increased intra-abdominal pressure and anatomical changes resulting in shunt displacement or occlusion. Management of VP shunt complications will be dependent upon symptoms, gestational age and guided by clinical status and imaging.
CHANGES IN MATERNAL PHYSIOLOGY AND THE IMPLICATIONS FOR ANAESTHESIA
Pregnancy brings about significant physiological changes within the woman. Such changes are largely the result of progesterone and oestrogens secreted initially by the corpus luteum (up to 12 weeks gestation) and later by the placenta. The physiological changes are important for placental development, fetal development and in preparing both fetus and mother for delivery. Such alterations in physiological status have major ramifications regarding safe anaesthetic conduct for the parturient to ensure not only maternal safety but also fetal wellbeing.
Cardiovascular System Changes
The cardiovascular system changes in pregnancy essentially involve increases in heart rate, stroke volume and cardiac output with a reduction in systemic vascular resistance (SVR). Vascular smooth muscle relaxation is mediated by progesterone and oestrogens resulting in vasodilation and reduction in SVR in the region of 20%. Systolic and diastolic pressures fall as a result. Reflex increases in heart rate and increases in stroke volume due to plasma expansion result in an increased cardiac output (30-50%). These changes are necessary to provide adequate utero-placental perfusion and anticipate blood loss during delivery. Uterine blood flow increases from around 100ml/min to 400ml/min at term.
Aortocaval compression describes compression of the maternal aorta and inferior vena cava by the gravid uterus from around 20 weeks of gestation (Figure 1). This compression is dependent on maternal position and is worse in the supine position where venous return and cardiac output are significantly reduced. The resultant drop in maternal cardiac output causes reflex increases in maternal SVR further impairing utero-placental perfusion. Utero-placental perfusion is not autoregulated and is dependent upon uterine perfusion pressure (arterial pressure minus uterine venous pressure). Maternal positioning needs careful consideration during all phases of peri-operative care.
Respiratory System Changes
Pregnancy has implications for both the upper and lower respiratory system. Endocrinological changes result in capillary engorgement and oedema of the upper airways. As a result airways are smaller and more vulnerable to trauma and further oedema. From an anaesthetic perspective, airway management is more difficult in the paturient. The incidence of failed intubation is quoted to be around 1:250, around ten times that of the nonpregnant population. As the uterus increases in size, there is reduction in lung volumes. Expiratory reserve volume, residual volumes and subsequently functional residual capacity (FRC) are all reduced by approximately 20% at term. This reduction in FRC combined with significant increases in maternal oxygen consumption result in rapid desaturation even after pre-oxygenation. As such, due care and attention is required in the management of the parturient with regards to airway and ventilation.
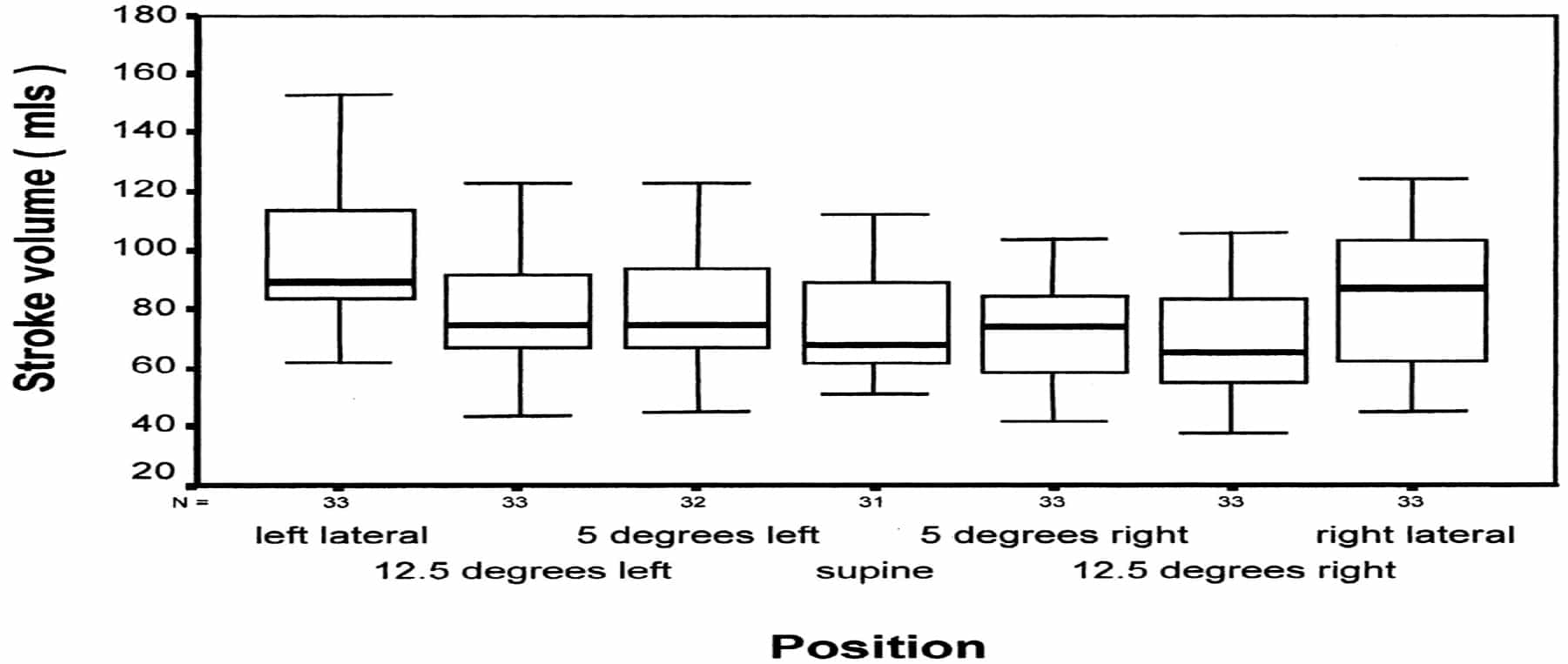
Figure 1: Box plot of maternal stroke volume related to position (from Bamber J H, Dresner M Anesth Analg 2003;97:256-58)
Progesterone mediated increases in respiratory rate and minute volume result in a reduced arterial partial pressure of carbon dioxide (PaCO2) of around 30mmHg. Maternal pH, however, remains within normal limits due to compensatory renal excretion of bicarbonate. Plasma bicarbonate levels are subsequently lower (~ 4 mmol/L) compared to non-pregnant levels. During anaesthesia PaCO2 levels should be maintained within these norms. As PaCO2 is often manipulated during neurosurgery to alter cerebrovascular tone and cerebral perfusion pressure, it is particularly important to be aware of these pregnancy induced changes, so that manipulation is appropriate. Manipulation of PaCO2 in addition to affecting cerebral perfusion pressure also impacts upon uterine perfusion pressure. Significant reduction in PaCO2 below 25mmHg reduces utero-placental perfusion and shifts the maternal oxygen-haemoglobin dissociation curve to the left, with resultant reduced oxygen delivery to the fetus.
Haematological System Changes
As a consequence of progesterone and oestrogens, renal excretion of renin and the activation of the aldosteronerenin- angiotensin system results in sodium retention and increases in plasma volume by up to 45%. There is also an increase in red cell mass (20%) due to increased erythropoietin production, although increases in red blood cell mass are not in line with the increase in plasma volume and a ‘dilution anaemia of pregnancy’ results. White cell count also increases as does platelet production but there is also an increased rate of platelet consumption with subsequent counts being normal. All clotting factors (excluding XI and XIII) are increased during pregnancy. As such pregnancy is associated with a hypercoagulable status which has significant implications regarding effective thromboembolic prophylaxis in the peri-operative period. Thromboembolic disease has been a leading cause of maternal mortality and morbidity for several years.
ANAESTHESIA FOR NEUROSURGERY
Timing of Surgery
Pregnant women presenting for non-obstetric surgery represent a unique clinical situation where the health of the mother is paramount but equally careful consideration needs to be given to her care regarding fetal wellbeing. At gestational ages greater than 24 weeks consideration must be given to early delivery and about the timing of delivery related to any neurosurgical intervention should that decision be reached. Figures 2 and 3 provide examples of such dilemmas for the management of SAH and primary CNS system tumours. Options include: i) delivery by Caesearean section proceeded by neurosurgery as continuous procedures, ii) delivery by Caesarean section with neurosurgery at a later date iii) maintain pregnancy and proceed with neurosurgery. At gestational ages <24 weeks there is no option to deliver and neurosurgical intervention can proceed. Optimising maternal physiology and consideration for fetal wellbeing should result in the best outcomes. Fetal management following surgery is then based around obstetric indications.
Conduct of Anaesthesia
The safe management of the parturient and the preservation of fetal wellbeing during anaesthesia are closely linked to a knowledge of and appreciation for the physiological changes described above. The best approach is likely to involve coordinated multidisciplinary team (MDT) involvement from the outset with clear plans regarding timing of surgery, timing of delivery and maternal and fetal management. As such obstetric, midwifery, obstetric anaesthetists, critical care and neonatal teams should be included in the planning and provision of maternal and fetal care in the peri-operative period. In the neurosurgical emergency, however, such MDT involvement may not always be possible.
The majority of neurosurgical procedures require general anaesthesia. There is no specific requirement for a particular induction or maintenance agents but rapid sequence induction (RSI) may be indicated. This will be dictated by gestational age and GI symptoms of the mother. Avoidance of pressor responses to laryngoscopy is vital especially in SAH. Induction of anaesthesia, therefore, should include the use of short acting opioids such as fentanyl (2-5 mcg/kg) or remifentanil (1 mcg/kg given over 60 seconds). Magnesium sulphate is also a good choice of drug for blunting the response to laryngoscopy. It is the drug of choice in eclamptic and pre-eclamptic patients and doses of 30-60mg/kg are effective. The literature also describes the use of lignocaine (1 mg/kg) and short acting beta-blockers such as esmolol (0.5-1 mg/kg). Lignocaine is, however, less effective than remifentanil and beta-blockers have been associated with fetal bradycardia. It is also important to note that ketamine increases uterine tone and should be avoided if possible. There is conflicting evidence in the literature regarding the impact of general anaesthesia (in particular agents working via GABA receptors) on neonatal neuro-behavioral performance. Research to date is based upon animal models, conflicting factors are numerous and there is debate about subsequent application to human neonates. Anaesthetic choice should therefore be base upon clinical requirements and agent familiarity.
With reduced oesophageal barrier pressures, pregnant women are very prone to acid reflux and subsequent aspiration on induction of anaesthesia. RSI is recommended from early in the second trimester. In the post partum period, progesterone levels fall within hours and gastric emptying time rapidly returns towards normal unless prolonged by other factors. The requirement for RSI in the post partum period, therefore, requires consideration but is recommended up to 48h post partum. Decisions about RSI will also be dependant upon the acute clinical picture. Antacid prophylaxis should be given prior to induction of anaesthesia. For example oral ranitidine 150-300mg one hour prior to surgery or 50mg intravenously if the oral route is not appropriate or surgery imminent.
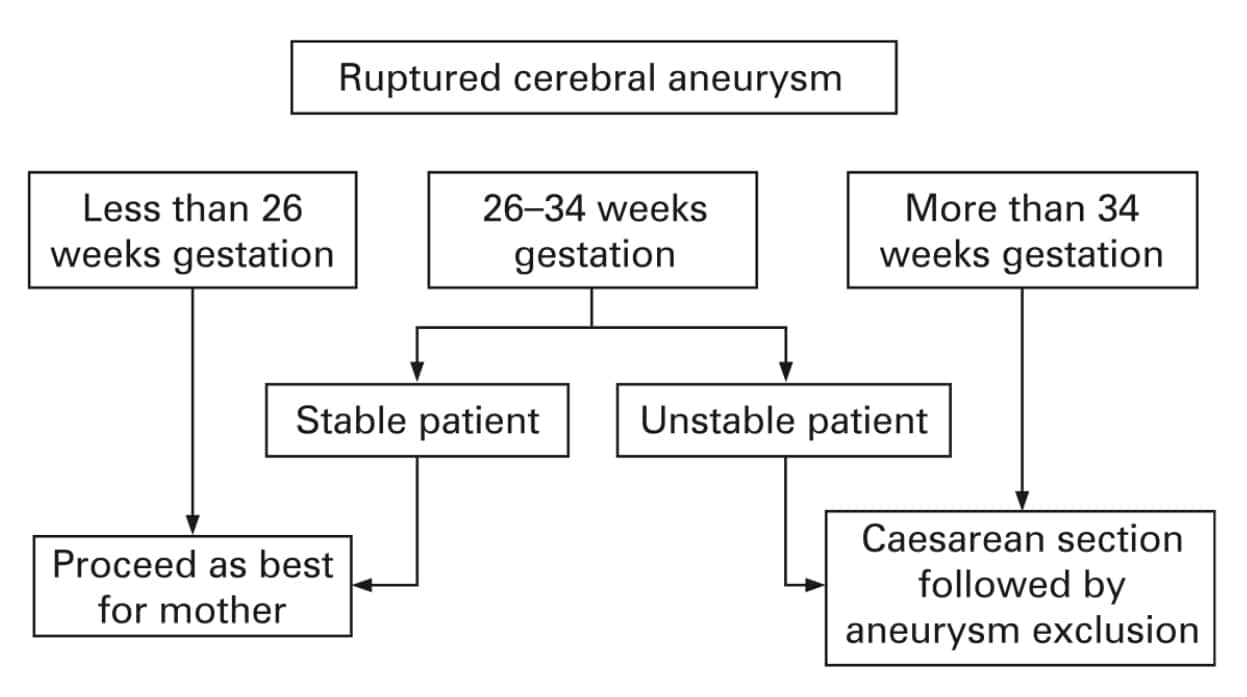
Figure 2: Strategy for the management of a ruptured cerebral aneurysm (from J Ng, N Kitchen. Neurosurgery and Preganancy. J Neurol Neurosurg Psychiatry 2008;79:745–52)
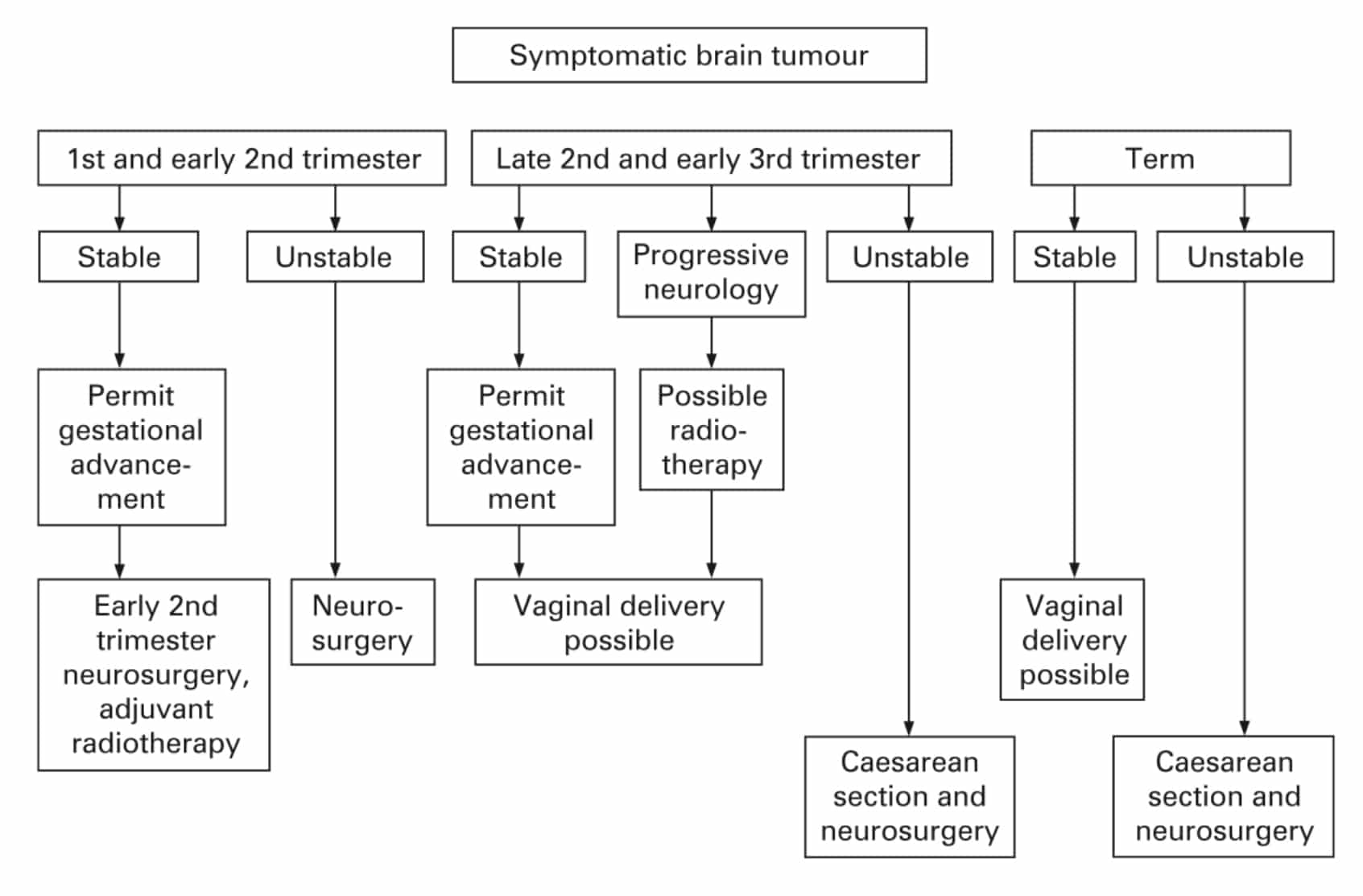
Figure 3: Strategy for managing intracranial tumours (from J Ng, N Kitchen. Neurosurgery and Preganancy. J Neurol Neurosurg Psychiatry 2008;79:745–752)
In addition 30mls of 0.3 M sodium citrate should be given orally within 30 minutes of induction of general anaesthesia if appropriate. Altered body habitus, airway and respiratory anatomical changes means that intubation is more likely to be problematic. Increased oxygen consumption results in rapid desaturation and thorough airway assessment is mandatory. In the 4th National Audit Project (NAP4), there were four cases of failed tracheal intubation at the time of emergency Caesearean section [9]. One patient had a surgical tracheostomy and two had failed attempts at cricothyroidotomy. There where no deaths but one patient had a cardiac arrest during the airway incident and another may have suffered an acute cardiac event secondary to prolonged hypoxia. Recommendations made in NAP4 suggest that major airway complications in obstetric patients are rare, but the physiology of pregnancy, active labour and isolated location may increase their complexity when they occur. In addition non-anaesthetic theatre personnel should be made aware of the considerable difficulty of these cases. As non-obstetric and non-anaesthetic physicians may not fully understand anaesthetic issues for parturients, decisions regarding the management of complex patients require close collaboration when forming initial and back-up plans.
Difficult airway algorithms do not specifically address the obstetric population and as such difficult airway equipment should be available and airway drills regularly rehearsed. Meticulous pre-oxygenation is paramount prior to RSI and placing patients in a head up ‘ramped’ position may facilitate intubation (Figure 4). Suxamethonium administration will result in a transient increase in ICP but its use in RSI is warranted where intubation may be potentially difficult and securing the airway safely and quickly are key objectives.
From 20 weeks gestation, aortocaval compression can occur in the supine position and to prevent this, the woman should be positioned with at least 15 degrees left lateral tilt either with a wedge under the right hip or by tilting the operating table to the left. It is worthwhile to note that anaesthetic assistants who do not practice obstetric anaesthesia regularly, may well apply cricoid pressure directly downwards and as such push laryngeal structures off to the side (left) worsening laryngoscopy views. The plan for intubation needs to be discussed fully with all staff involved including rescue plans should intubation prove difficult or impossible.

Figure 4: The Oxford Head Elevating Laryngoscopy Pillow (HELP)
As discussed previously, ventilatory parameters will be influenced by the normal maternal compensated respiratory alkalosis. Manipulation of maternal PaCO2 has implications for oxygen delivery to the fetus both in terms of uterine perfusion and the p50 point of the maternal oxygen-haemaglobin dissociation curve. Hyperventilation to manipulate maternal ICP remains an option although it is recommended that PaCO2 should be kept between 25-30 mmHg.
Haemodynamic stability and the avoidance of large swings in blood pressure in the peri-operative period is beneficial for maternal, fetal and neurosurgical reasons. As such it is prudent to site invasive arterial pressure monitoring prior to induction. Hypertension related to laryngoscopy can be provided by short acting opioids and magnesium sulphate given at induction is also effective and may be beneficial in pre-eclamptic states. Maternal positioning to avoid aortocaval compression is paramount and ideally patients should be managed in the full left lateral position if surgically feasible. Large bore intravenous access is required and central venous access should be sited on a case by case basis if vasoactive substances or central venous pressure monitoring is required. Blood pressure should be manipulated within ‘normal’ limits but it is important to note that some neurosurgical pathology may be the result of pregnancy induced hypertensive states and should be manipulated to ‘normal’ levels. Ephedrine is no longer the vasopressor of choice in the parturient. The use of selective alpha agonists such as phenylephrine are associated with better maternal cardiovascular stability and improved fetal acid-base status [10,11].
Spinal surgery represents a particular conundrum regarding patient positioning. Normally spinal surgery is carried out in the prone position. Whilst the prone position provides good utero-placental perfusion, the mechanics are challenging in the pregnant population. There are a few case reports of spinal surgery carried out prone under regional anaesthesia, where the women positioned themselves prone prior to surgery. [12].
If the patient is going to be extubated following neurosurgery then as with induction, due care is required to prevent reflux and aspiration of stomach contents. In the last Confidential Enquiry into maternal deaths, one maternal death was associated with asphyxia, secondary to aspiration of stomach contents on extubation [1]. Patients should be fully awake and airway reflexes intact.
Pharmacokinetic and Pharmacodynamic Considerations
Alongside profound physiological changes, there are also pharmacodynamic and pharmacokinetic changes related to absorption, distribution, metabolism and excretion of drugs. Pregnancy is associated with a state of general malabsorption of drugs from the gastrointestinal (GI) tract. Dilutional hypoalbuminaemia is associated with a decrease in drug binding capacity and an increase in volume of distribution for many drugs. Changes to hepatic enzyme systems result in up-regulation of some but reduced activity in others. Glomerular filtration rate is also significantly increased in pregnancy and as such the rate of renal drug excretion is increased although this is somewhat balanced by changes in tubular reabsorption. Phenytoin is used commonly in neurosurgical patients and has been relatively well studied in pregnancy. It has been shown to be poorly absorbed from the GI tract and undergoes increased plasma clearance. As such dosing in pregnant women needs particular consideration and monitoring to achieve therapeutic plasma concentrations. Pregnancy is also associated with lower anaesthetic requirements, with the minimum alveolar concentration (MAC) of inhalational agent being reduced by up to 30%. Intravenous induction agents are also often required in lower doses. It is important to note, however, that the incidence of awareness in the pregnent population is higher. This is in part due to the emergency nature of a large proportion of obstetric surgery, reduced induction to incision times to minimise fetal transfer and a higher maternal cardiac output resulting in rapid redistribution of induction agents.
Other drugs commonly administered in the peri-operative period include steroids (dexamethasone), osmotic diuretics (mannitol) and calcium channel antagonists (nimodipine) in the case of SAH to prevent cerebral vasospasm. In animal studies, maternal administration of mannitol results in significant increases in maternal osmolality, with subsequent fetal dehydration and contraction of blood volume. In human studies, increases in maternal and fetal plasma osmolality have also been demonstrated, although the effects on fetal outcome are unknown. Ultimately if it is being administered to treat severe or life threatening intracranial hypertension then its use is warranted. The evidence base for the use of specific calcium channel antagonists in pregnancy is limited. Animal studies have demonstrated that nimodipine may increase the risk of intra-uterine growth retardation and congenital abnormalities but no comparative studies in humans are available. The parturient is somewhat protected from cerebral artery vasospasm in their relatively haemodiluted and hypervolaemic state. However, the known benefits of nimodipine in preventing spasm are likely to outweigh any potential risk to the fetus and should be administered as clinically indicated. Steroid administration is routinely used for fetal lung development in the event of pre-term labour. Betamethasone is currently the steroid of choice due to better fetal outcomes but maternal administration of dexamethasone in a neurosurgical setting is safe.
FETAL OUTCOMES
Whilst maternal wellbeing is the primary objective, the prevention of fetal harm is also a major clinical goal. This may be compromised by maternal hypotension, maternal hypoxaemia, utero-placental hypoperfusion and aberrations in acid base status. In addition consideration needs to be given to the direct effects of anaesthetic and analgesic drugs together with indirect effects such as teratogenicity during the most vulnerable period of fetal organogenesis (15-56th day). The Swedish Catalogue of Registered Pharmaceutical Specialities (FASS) [13] has data regarding most medicines and their impact on fetus, placenta and utero-placental blood flow. The impact of general anaesthetic on neonatal neurobehavioral development has been discussed previously.
The use of fetal heart rate monitoring in the emergency setting is debatable. As a predictor of fetal mortality it is only useful after 24 weeks gestation. The use of fetal heart rate variability as an indicator of fetal wellbeing is also only useful after 26 weeks gestation and can be significantly impacted upon by general anaesthesia. In the acute peri-operative period, fetal heart rate monitoring needs careful consideration and discussion with obstetricians regarding its value. The benefit of any clinical monitor depends on the expertise and understanding of the clinician using it. If there are no personnel to interpret changes in fetal heart rate then its use is limited. In addition, if there is no facility for definitive obstetric care in the event of evidence for significant fetal compromise then its value is also questionable. Fetal heart rate monitoring may be of use to assess the effects of changes in maternal physiology and wellbeing in the peri-operative period and may guide interventions such changes in maternal position and manipulation of cardiorespiratory parameters.
Neurosurgical pathology may require exposure to radiation either for diagnostic imaging or for radiological intervention such as coiling of aneurysms. As such, the fetus may well be exposed to recurrent, cumulative radiation doses. Recommendations of the International Commission on Radiological Protection (2007) suggest no deterministic effects of significance would occur below radiation doses of 100 mSv and that no radiological procedure would result in fetal doses above 100 mSv. For example a head CT exposes a fetus to 0.01-0.1mSv, with a risk of childhood cancer of 1:1 000 000 per examination. A CT angiogram and coiling results in a greater radiation dose with estimates ranging up to 10mSv exposure to the mother. Estimating fetal doses is difficult and is very dependent on gestational age. Almost certainly the benefit of exposure is likely to outweigh fetal risk, but consideration should be given prior to any radiological intervention.
CONCLUSION
The requirement for neurosurgery in the parturient is a rare occurrence. When these patients do present, however, their care is likely to be complex and challenging. As such, a multi-disciplinary approach should be adopted throughout their period of care. The emergency nature of neurosurgical conditions require departments to be familiar with the management of pregnant patients. Protocols should be developed for such emergencies with established lines of communication and referral between specialties.
ANSWERS TO QUESTIONS
- a. F – the risk of bleeding from AVMs is not more common during pregnancy but should bleeding occur the chance of re-bleeding is higher.
b. F
c. F
d. T
e. F – meningiomas are not more common but may grow rapidly and become symptomatic due to the expression of oestrogen and progesterone receptors. - a. F
b. T
c. F – all factors are increased excluding XI and XIII
d. F – there is increased renal excretion of bicarbonate to compensate for the respiratory alkalosis
e. F – platelet production and consumption both increase with resultant normal levels - a. F – MAC values decrease by up to 30%
b. T
c. F
d. F
e. T - a. F – aorto-caval compression can occur from 20 wks gestation
b. F – phenylephrine is the vassopressor of choice
c. F – it is only a useful predictor of fetal mortality after 24 wks gestation
d. T
e. F – Esmolol has been associated with fetal bradycardia
REFERENCES and FURTHER READING
- Centre for Maternal and Child Enquiries (CMACE). Saving Mothers’ Lives: reviewing maternal deaths to make motherhood safer: 2006–08. The Eighth Report on Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG 2011; 118 (Suppl. 1): 1–203
- Dias MS, Sekhar LN. Intracranial hemorrhage from aneurysms and arteriovenous malformations during pregnancy and the puerperium. Neurosurgery 1990;27:855–65.
- Hunt HB, Schifrin BS, Suzuki K. Ruptured berry aneurysms and pregnancy. Obstet Gynecol 1974;43:827–37.
- Wang LP, Peach MJ. Neuroanesthesia for the Pregnant Woman. Neurosurgical Anesthesiology 2008;107(1):193-200.
- Shah AJ, Kilcline BA. Trauma in pregnancy. Emerg Med Clin N Am 2003;21:615–29
- Weinberg L, Steele R G, Pugh R, Higgins S, Herbert M, Story D. The pregnant trauma patient. Anaesth Intensive Care 2005;33:167–80.
- Fast A, Shapiro D, Ducommun EJ, Friedmann LW, Bouklas T, Floman Y. Low back pain in pregnancy. Spine 1987;12:368–71.
- Ng J, Kitchen N. Neurosurgery and pregnancy. J Neurol Neurosurg Psychiatry 2008;79:745–752.
- Cook T, Woodall N, Frerk C. 4th National Audit of the Royal College of Anaesthetists and the Difficult Airway Society: Major complications of airway management in the United Kingdom 2011. http://www.rcoa.ac.uk/index.asp?PageID=1089 (accessed 23/03/2012)
- Ngan Kee WD, Lee A, Khaw KS, Ng FF, Karmakar MK, Gin T: A randomized double-blinded comparison of phenylephrine and ephedrine combinations given by infusion to maintain blood pressure during spinal anesthesia for cesarean delivery: Effects on fetal acid-base status and hemodynamic control. Anesth Analg 2008; 107:1295–302.
- Cooper DW, Carpenter M, Mowbray P, Desira WR, Ryall DM, Kokri MS. Fetal and maternal effects of phenylephrine and ephedrine during spinal anesthesia for caesarean delivery. Anesthesiology 2002;97:1582–90.
- Brown MD, Levi ADO. Surgery for lumbar disc herniation during pregnancy. Spine 2001;26:440–3.
- http://www.fass.se/LIF/miljo_splash/index_en.jsp (accessed 23/03/2012)



