Obstetrics Anaesthesia
QUESTIONS
- During pregnancy the following occur
a. FRC increases
b. stomach acidity increases
c. oxygen consumption remains the same as none pregnant
d. respiratory rate decreases
e. cardiac output increases < 5 % - Obesity
a. is not associated with an increase in difficult intubation
b. the dose /kg of suxamethonium is unchanged from none pregnant
c. is associated with an increase in diabetes
d. the risk of heart failure increases with duration of obesity
e. BMI >40 is associated with a reduction in life expectancy - Anaesthetic aspects of management of the obese pregnant woman include:
a. 1:250 risk of failed intubation
b. decreased risk of dural tap
c. increased risk of antenatal haemorrhage
d. decreased rate of LSCS with increasing BMI
e. increased rate of shoulder dystocia. - Regarding drugs for caesarean section,
a. morphine as a sole analgesic is ideal
b. halothane is a better choice than isoflurane
c. drugs with a high fat solubility are best avoided
d. the dose of atracurium is based on actual body weight
e. non-steroidal anti inflammatory drugs are useful in obese women with preeclampsia
INTRODUCTION
This tutorial examines the problems obesity presents in pregnancy, labour and delivery and the associated challenges of anaesthesia.
Obesity is a growing problem in the Western world and in parts of the developing world. The world health organisation (WHO) describes obesity, which is more common in women, as a pandemic. Alarming statistics are shown below:
- In 1990 the USA spent $ 46 billion dollars on obesity; 6.7% of the health care budget.
- In 2002 WHO estimated 2.5 million deaths were due to obesity, including 220,000 in Europe.
- Over the period 1993 to 2002, UK women aged 16-44 with a BMI> 30 increased from 12% to 18.3% and those with a BMI >40 increased from 9% to 17%.
Obesity can be quantified by using the body mass index (BMI).
BMI = Weight (Kg)/ (Height (m)) 2
BMI does not take into account frame size or the distribution of the fat. The WHO classification of obesity is shown below:
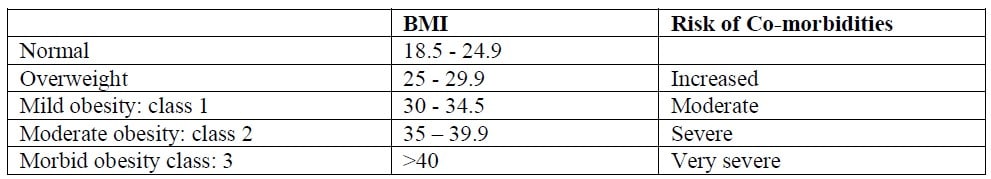
BMI over 40 is associated with a reduction in life expectancy. Physiological changes occur in both pregnancy and obesity which can be additive, resulting in significant challenges for the anaesthetist.
PHYSIOLOGICAL CHANGES IN OBESITY
It has been known for a many years that obesity is unhealthy. William Shakespeare wrote several hundred years ago in his play Henry IV; “I am fatter than others and so in bad health”.
Respiratory system
- Reduced functional residual capacity (FRC) with risk of hypoxia due to reduced reserves of oxygen.
- Reduced closing capacity.
- Restrictive respiratory pattern due to the additional weight on the thorax and restriction of diaphragm movement leading to impaired diaphragm function.
- Poor respiratory compliance resulting in fast, low volume breaths.
- Increased pulmonary resistance due to low lung volumes and possible hypoxia.
- Obstructive sleep apnoea (OSA). 50-90% of morbidly obese have some degree of OSA with risk of pulmonary hypertension and cor pulmonale. Resulting sympathetic stimulation may lead to hypertension.
- Increased risk of difficult airway and intubation. Increased breast tissue / fat pad on back makes head positioning difficult for intubation.
- Increased metabolic demand of breathing due to increased work of moving the chest / diaphragm.
- Risk of atelectasis and shunt / V: Q mismatch.
- Obese hypoventilation syndrome (Pickwickian syndrome) – 5-10% of morbidly obese.
- Increased risk of regurgitation and aspiration.
Cardiovascular
- Increase in blood volume.
- Increase in cardiac output proportional to degree of obesity; i.e. fat needs 2-3 mls blood/100g/min so extra 50 kg needs 1-1.5l/min extra cardiac output.
- Possible increase in haematocrit due to hypoxia.
- Hypertension; found in up to 60% of obese leading to increased afterload and left ventricular hypertrophy.
- Right ventricular hypertrophy secondary to OSA.
- Systolic and diastolic dysfunction.
- Increased arrhythmia due to fatty deposits in the myocardium.
- Increased preload due to increase in blood volume.
- Risk of myocardial ischaemia due to increased oxygen demand and reduced supply.
- Dilated cardiomyopathy; due in part to volume overload.
- Heart failure; increased risk with duration of obesity.
- Increase in ischaemic heart disease.
- Risk of supine hypotension due to aorto-caval compression.
Gastrointestinal
- Increased acid reflux.
- Increased residual volume of stomach.
- Increased gastric acidity.
- Increased risk of gallstones.
- Fatty infiltration of liver and possible abnormal Liver function tests
Metabolic
- Increased oxygen demand to counter the increased work of breathing.
- Increased plasma lipids which increases the risk of atheroma. Elevated lipids can lead to endothelial activation.
- Adipose tissue is active and produces many substances including leptin which is involved in appetite reduction by an action at the hypothalamus (leptin resistance is seen in obesity), interleukin 6 (IL6), TNF-alpha. Substances from fat are involved in the complement system, lipid/protein/glucose metabolism, steroid production, angiogenic function and inflammation.
Renal.
- Increased angiotensin converting enzyme and renin levels.
- Increased leptin which results in increased sodium absorption and renal vasodilation.
- GFR increases.
- High intra abdominal pressure can reduce renal blood flow.
Endocrine
- Leptin increases sympathetic drive via the hypothalamus, leading to hypertension, sodium and water retention.
- Insulin resistance leading to initially high levels of insulin that together with leptin and free fatty acids stimulate the sympathetic nervous system.
- Increase in diabetes; risk increases as BMI increases.
Musculoskeletal
- Difficulty in positioning the patient including the left tilt/lateral position to limit aortocaval compression.
- Risk of rhabdomyolysis (ischaemia and death of muscle due to reduced blood supply as a result of immobility) with prolonged surgery e.g. buttock ischaemia.
Coagulation
- Increased risk of deep vein thrombosis and thromboembolic events.
Pharmacokinetics
- Increased fat.
- Reduced total body water.
- Increase in lean body mass.
Psychological
- Increased depression and suicide.
Many of the physiological changes in pregnancy are similar to those observed in the obese. These physiological changes have been covered in detail in a previous tutorial and include:
- Increased oxygen consumption and carbon dioxide production
- increased respiratory rate
- decreased FRC
- difficult intubation and increased aspiration risk
- increased cardiac output
- increased heart rate
- left ventricular hypertrophy
- increased blood volume
The further physiological impact of obesity on pregnancy is therefore significant and results in high risk of complications during pregnancy, labour, delivery and during the post-partum period.
PREVENTION
Pubic health programs are essential to reduce the number of obese women in the community through encouragement of weight loss pre-pregnancy and targeting the number of obese children. Many women are unaware of the risks of pregnancy and obesity. In some groups including the Samoans, this is culturally difficult as obesity is equated with strength and status. In the Arab/African world the larger lady is seen as more desirable. Young girls may be force fed and given steroids to fatten them up as in Mauritania – some of these women die of hypertensive renal failure before getting pregnant.
Children of women who were obese in pregnancy have an increased risk of becoming obese as adults. The number of obese women who breast feed is less than lean women. Breast feeding protects against obesity in adulthood.
OBESITY AND PREGNANCY
Morbid obesity is often associated with infertility but many women become pregnant when weight is lost. The British infertility society advises against fertility treatment if BMI >35.
Obese women may already have pre-existing disease with end organ damage e.g. diabetes, hypertension and ischaemic heart disease.
Obesity is associated with increased maternal morbidity and mortality. Obesity increases almost all the complications of pregnancy and delivery:
- Increased miscarriage.
- Increased fetal abnormality e.g. cardiac and neural tube defects. Detection may be difficult due to sub-optimal view at ultrasound.
- Increased premature delivery.
- Gestational diabetes (risk increases with increasing BMI).
- Pre-eclampsia (risk increases with increasing BMI).
- Increased post partum haemorrhage.
- Peripartum cardiomyopathy.
- Increased risk of Caesarean section (CS). This risk increases as BMI increases and over 40% of women with BMI >40 may require caesarean delivery.
- Increased risk of thromboembolic events.
- Increased wound infection/ wound breakdown.
- Increased infection of the uterus (endometritis).
- Low vaginal delivery rate after LSCS with increased risk of uterine rupture.
- Increased rate of induction e.g. for large baby /diabetes/ pre eclampsia. Induction may often be unsuccessful in the obese.
- Increased augmentation of labour.
- Increased post natal depression reducing the chance of successful weight loss post delivery.
The uterus in the obese can be infiltrated by fat, like other organs including the liver and heart, and this may explain its poor contractile ability both pre and post delivery. Pushing can be ineffective and intra abdominal fat can obstruct labour.
The UK (BMI>35) and USA recommend that the obese pregnant woman is reviewed by the anaesthetist before delivery to discuss the risks and out line the options for pain relief and delivery. A management plan along with the results of relevant investigations e.g. ECG, respiratory function tests, echocardiography, should be clearly documented in the notes.
CONDUCT OF ANAESTHESIA
Departments should have clearly written guidelines on the management of obese women through their pregnancy, labour and delivery. Guidelines should include recommendations for:
- Early intravenous access (often more difficult in raised BMI)
- Thomboprophylaxis regimens
- Discussion and consideration of early insertion of regional anaesthesia
- Antacid prophylaxis
- Early referral to senior anaesthetist
- Availability of appropriate manual handling devices
Women should be weighed and their weight and BMI recorded clearly in the notes.
EQUIPMENT
- The operating table must be wide enough and able to handle the weight of the patient. It is possible to buy lateral extensions for the table and arm boards are useful.
- Manual handling equipment including hoists, slide sheets and wide wheelchairs should be available and unnecessary transfer of patients avoided. Staff should be trained in correct transfer of patients to limit injury.
- Electric beds that sit the patient up are ideal but costly and must be able to take the weight of the patient.
- Large gowns are required.
- Wide blood pressure cuffs are required to provide accurate readings (width of cuff should be 20% diameter of the arm). A small cuff will give a falsely high reading. Intra arterial monitoring of blood pressure may be needed if there are problems with non-invasive blood pressure monitoring.
- Large compression stockings/ mechanical calf compressors are needed for DVT prophylaxis.
- Long spinal and epidural needles must be available. The long epidural needles, 11cm, will suffice for the majority of patients. It may be necessary to use an epidural needle as an introducer for a spinal needle. A 120mm spinal needle for a standard 8 cm epidural needle and 150mm for a 11cm epidural needle. Epidural needles of 15 cm and spinal needles up to 175mm are available. Ultra sound imaging of the lumbar spine has been shown to assist location of the epidural and spinal space and this may be especially useful in obese women where surface landmark anatomy may be very difficult to identify
ANALGESIA FOR LABOUR
Regional analgesia has many advantages though is often challenging in the obese patient. It can provide the most effective form of pain relief and decrease respiratory and cardiovascular work during labour. Obese women are at increased risk of instrumental and caesarean delivery so a working epidural may reduce the risk of general anaesthesia.
Regional analgesia is often best performed early in labour to optimise positioning and may be easier in the sitting position since the midline may be identified more easily than in the lateral position. Regional anaesthesia has been described in patients with a BMI as high as 88, and there is increasing evidence that ultrasound may be beneficial in aiding epidural insertion. Regional analgesia can also help with the placement of a fetal scalp electrode as trans-abdominal monitoring of the fetal heart rate is often not possible in the morbidly obese.
There are specific issues concerning epidural and spinals in obese patients:
- More difficult to insert.
- Increased risk of the epidural catheter becoming displaced.
- Increased risk of inadvertent dural tap. There is a lower than expected post-dural puncture headache rate. It has been proposed that this is due to increased pressure in the epidural space due to high venous pressure and increased amount of epidural fat.
- This fat may result in higher than expected block levels.
Many obese women now receive ante-natal heparin and if so, they should be warned to omit the dose when labour commences. 12 hours should elapse following a prophylactic dose of low molecular weight heparin and 24 hours following a therapeutic dose prior to spinal/epidural insertion.
Alternative analgesia includes the following:
- Entonox (50% nitrous oxide in oxygen) can be useful.
- Intra muscular opiates. May result in variable absorption and effect.
- Patient controlled intravenous analgesia. Short acting drugs like remifentanil avoid the risk of long lasting sedation and respiratory depression.
ANAESTHESIA FOR OPERATIVE PROCEDURES
Regional anaesthesia
Regional anaesthesia may be challenging to perform and have additional risks in the obese patient but it is more preferable than general anaesthesia for operative procedures.
- Ideally, obese women considered to be at high risk of intervention should receive early epidural analgesia and its effectiveness monitored throughout labour.
- If the patient presents without a working epidural, a combined spinal epidural (CSE) may be preferable to single shot spinal as surgery is more often difficult and prolonged in the obese and a CSE allows a block to be extended if necessary.
- Adequate leftward tilt to avoid aorto-caval compression must be provided once supine. This may be difficult to achieve safely in the obese patient.
- The patient may find it difficult to lie flat and may need to be placed head up and oxygen may be required.
High regional block may be more common in the obese so a CSE technique with a smaller dose of spinal anaesthetic with an epidural top up to the required level may be preferable. The epidural needle may aid spinal placement by acting as a long spinal introducer needle, however there is a higher failure rate of epidurals compared to spinals. A spinal catheter has the advantage of providing a block that can be extended but insertion of spinal catheters can be technically difficult.
General anaesthesia.
General anaesthesia presents many challenges and should be avoided if possible for a number of reasons:
Airway and ventilation challenges
- It is well known that failed intubation is more common in the pregnant (1:250) than nonpregnant woman (1:2000) and pregnant women are at increased risk of regurgitation and acid aspiration.
- The airway should be thoroughly assessed as soon as the obese woman presents to the delivery suite. If difficult airway management is predicted, early epidural placement should be advised.
- Due to a reduced FRC and increased oxygen consumption, pregnant obese women desaturate rapidly following induction.
- Rapid sequence intubation with pre-oxygenation, thiopentone, suxamethonium and cricoid pressure is usual. Suxamethonium dose should be based on the patient’s total body weight, using the usual dose of 1- 1.5mg/Kg. The recent arrival of sugamedex, which rapidly reverses the neuromuscular block of rocuronium may lead to the increased use of rocuronium in this group of patients.
- Adequate head and neck positioning for intubation can be very difficult in the obese parturient and time should be taken to ensure the best position is achieved prior to induction. The ‘ramped’ position may be more effective in the obese. In this position, pillows are placed under the upper thoracic region as well as the head to ensure the opening of the ear is in line with the sternal notch. A slightly ‘head up’ position may be more comfortable for the patient and improve FRC.
- Adequate pre-oxygenation is essential: 3 minutes of tidal volume breathing or 4-6 vital capacity breaths of 100% oxygen with a tight fitting face mask.
- Measures to avoid aorto-caval compression should be taken as above.
- If the patient is in the ramped position or placed head up, the anaesthetist may need to stand on a step behind the patient. Both of the patient’s arms placed on arm boards may allow the breasts to fall toward the axillae and aid placement of the laryngoscope as well as reduce pressure on the chest wall.
- A full range of difficult intubation equipment should be immediately available including. bougies, stylets, different laryngoscopes etc. A short-handled laryngoscope may be especially useful in the obese to aid placement. A polio laryngoscope blade should also be available.
- Awake fibreoptic intubation is an option if general anaesthesia is required and difficult intubation is predicted. This may be challenging and care must be taken if intubating via the nose since bleeding is more likely in the pregnant patient.
- Once intubated, airway pressures may be high. Positive End Expiratory Pressure (PEEP) can help with oxygenation and head up positioning may improve respiratory compliance.
Drugs
Effective dosing of drugs is a challenge and there is confusion as to which weight to base drug calculations on: total body weight (TBW), lean body weight (LBW) or ideal body weight (IBW). LBW increases in obesity due to the additional muscle that develops to carry the extra weight of the body. Which weight to use for drug calculation depends on the properties of the individual drug including its fat solubility which affects its volume of distribution.
Analgesia
Effective analgesia is essential to manage post operative pain, encourage mobilisation and help reduce the risk of thromboembolic complications. Analgesia should be multi-modal and regular. Simple analgesia e.g. paracetamol and non-steroidal anti-inflammatory drugs, if not contraindicated, should be prescribed regularly and may help reduce the requirements for opioids and limit their associated side effects . Local anaesthetics either as wound infiltration, bilateral ilio-ingunial blocks or transversus abdominis plane (TAP) blocks should be used.
Care should be taken at extubation. Assessment of reversal of neuromuscular blockade should be made prior to wake up. Traditionally patients have been extubated on their side following anaesthesia for caesarean section. In the obese, however it may be preferable to extubate women awake in the sitting position to optimise ventilation. This is also the best position for post operative care.
Post operative care
Problems can occur once the woman has left theatre and the immediate postoperative care of the obese parturient must be by a suitably trained person. Transfer to a High Dependency Unit for appropriate monitoring and possible CPAP administration may be required. Post operative physiotherapy should be organised and pressure relieving mattresses should be used to prevent pressure sores. Post-operative oxygen therapy may reduce the risk of hypoxia which in turn reduces infection. If the patient is normally on CPAP at night this should be continued. Women should be encouraged to mobilise as soon as possible as this helps with respiratory mechanics and prevention of thromboembolic complications.
PREVENTION OF VENOUS THROMBOEMBOLISM
Obese parturients are at high risk of thromboembolic complications and this risk is increased if they have undergone an operative procedure. Early mobilisation should be encouraged, dehydration avoided and calf compression devises used in all patients. In addition, post delivery heparin thromboprophylaxis should be prescribed. e.g. enoxaparin 40mg prescribed daily for 5-7 days or until mobilising normally if <90 kg and twice daily if >90kg. Heparin should be given 4 hours after spinal, epidural insertion or removal of epidural catheter to avoid the risk of spinal/epidural haematoma.
SUMMARY
Obesity is associated with many physiological changes which can result in a reduced ability to cope with the demands of pregnancy, labour and delivery. These women are at high risk and present a real challenge to the anaesthetist and all the team involved in their care. Management should be planned in advance and the necessary equipment and expertise available.
ANSWERS TO MULPTIPLE CHOICE QUESTIONS
- a) f b) t c) f d )f e) f
- a) f b) t c) t d) t e) t
- a) t b) f c) f d) f e) t
- a) f b) f c) t d) f e) f
FURTHER READING
- Saravanakumar K, Rao S.G, Cooper G. Obesity and obstetric anaesthesia. Anaesthesia 2006; 61: 36-48
- Obesity and pregnancy. 2008. Royal Society of Medicine. Editors Rees M, Karoshi M, Keith L



