Basic Sciences
In the first of this two tutorial series, Cardiac Implantable Electronic Device (Cardiac pacemaker and implantable cardioverter defibrillator or CIED) technology will be discussed along with indications for their use. Part two will cover the anaesthetic considerations for patients with these devices.
QUESTIONS
The answers, together with explanations will be published at the end next week’s tutorial.
- Which of the following statements are correct regarding pre-operative pacing?
a. If a patient presenting for elective surgery is found pre-operatively to have bi-fascicular block with 1st degree AV block, the patient should have a transvenous pacemaker before the operation irrespective of cardiovascular symptoms.
b. If a patient presenting for emergency surgery has symptomatic third degree heart block, the patient should always have a permanent pacemaker inserted before the surgery can safely proceed.
c. Asymptomatic Type II second degree AV block is NOT an indication for pre-operative pacemaker insertion before elective surgery.
d. Asymptomatic First degree AV block is extremely unlikely to progress to second degree block in the perioperative period. As a result they do not require pre-operative pacing. - List 5 potential adverse events that may arise if a patient with an implanted pacemaker is exposed to MRI?
- Which of the following statements are true regarding the perioperative management of pacemakers and ICDs?
a. A Magnet placed over a pacemaker device is a recommended alternative to formal device re-programming before an operation involving diathermy.
b. If pulseless shockable rhythm occurs intra-operatively in a patient with a program- inactivated Implantable Cardioverter-Defibrillator (ICD), the first step would be to page the cardiology technician to re-enable the ICD.
c. If a pulseless shockable rhythm occurs intra-operatively in a patient with an implanted pacemaker, the patient should immediately be externally defibrillated using standard energy levels.
d. On an X-ray film, one can most reliably distinguish between an ICD and a permanent implantable pacemaker (PPM) by looking at the generator box.
INTRODUCTION
CIEDs have revolutionized the treatment of patients with cardiac arrhythmias. In Canada there are currently over 200,000 patients with CIEDs and in the United States more than 100,000 electronic cardiac rhythm devices are implanted per year. Patients with these electronic devices represent unique challenges to the anaesthetist. Once a patient is identified as having a cardiac implantable electronic device, a pre-operative assessment must answer specific questions concerning:
- The type of the device and program mode.
- Whether the device is functioning properly.
- The patient’s dependence on the device.
- The probability of electromagnetic interference in theatre and how to minimize the risk.
The anaesthetist should then formulate a management plan in conjunction with the surgeons and cardiologists in order to avoid unnecessary morbidity or mortality. Recent position statements have been published to help the anaesthetist with perioperative management of patients with these devices (Healey JS et al. 2012 and ASA taskforce, 2011)
IMPLANTED CARDIAC PACEMAKERS
External pacemakers started to be developed in the 1950s. In the 1960s implantable transvenous pacemakers were introduced. Permanent cardiac pacing was originally designed for management of Stokes-Adams (Syncopal) attacks in patients with complete heart block. With advances in cardiology and technology, the indications for permanent pacing have since broadened (Table 1).
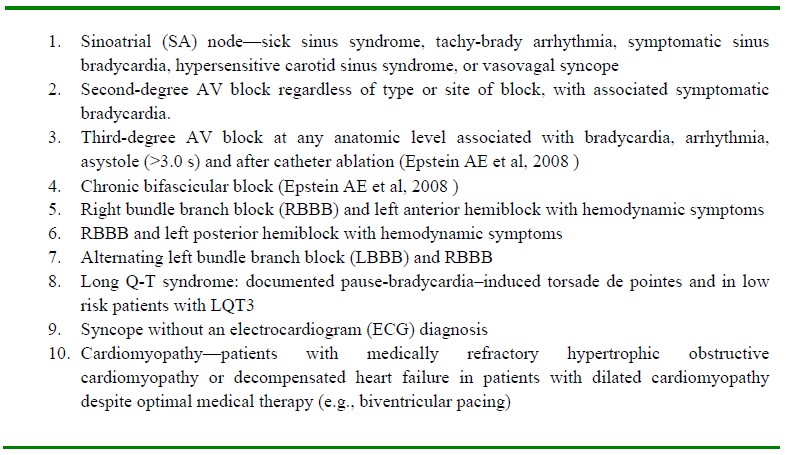
Table 1: Indications for insertion of a permanent implanted Pacemaker. Artificial pacing is generally indicated for the treatment of symptomatic bradycardia of any origin.
A permanent cardiac pacemaker (PPM) system consists of:
- A “pulse generator”: a device that generates electrical impulses.
- Leads and electrodes connected to the heart used for sensing & pacing.
The leads and electrodes can either be attached to the heart via the intravenous route (endocardial leads) or via a subcostal approach (epicardial or myocardial leads). The leads are then attached to the pulse generator device and implanted under the patient’s skin. It may also be inserted deep to muscle layers. The device is powered by a lithium-iodide battery. Electrical stimulation from the generator results in myocardial contraction.
Pacemaker mode codes
The fundamental information required to understand normal pacemaker behaviour is the pacemaker code. The currently used North American Pacing and Electrophysiology/British Pacing and Electrophysiology Group (NASPE/BPEG) pacemaker codes are used to describe pacemaker types and function. Table 2 delineates all pacemaker codes.
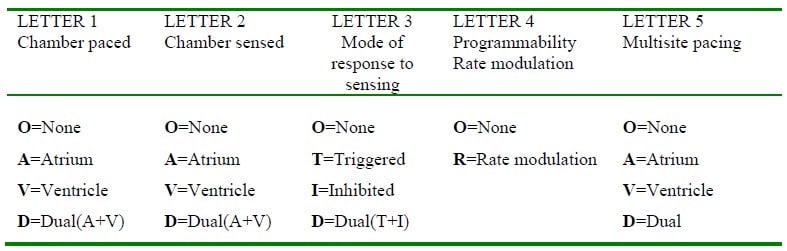
Table 2. The North American Pacing and Electrophysiology/British Pacing and Electrophysiology Group (NASPE/BPEG) pacemaker codes (2002). Letter 5 is the most recently introduced eg DDDRV represents a Dual paced, Dual sensed, Dual response Rate responsive biVentricular pacemaker
Pacing modes
Modern day pacemakers are programmable into one of the four modes of pacing:
- Asynchronous pacing
- Single-chamber demand pacing
- Dual-chamber atrioventricular (AV) sequential demand pacing
- Rate adaptive pacemaker
1. Asynchronous or fixed-rate modes:
These modes pace at a preset rate that is independent of the inherent heart rate. They can be atrial (AOO), ventricular (VOO), or dual chamber (DOO). Competition and ventricular fibrillation (VF) are the potential complications when normal heart rate reappears. If an impulse is generated at the same time as the patient’s own ‘T’ wave, theoretically this could induce ventricular fibrillation (R on T phenomenon).
2. Single-chamber demand pacing:
This mode paces at a preset rate only when the spontaneous heart rate drops below the preset rate. The ventricular-inhibited pacer (VVI) is the most popular type which is suppressed by normal electrical activity of the patient’s own QRS complex.
3. Dual-chamber AV sequential pacing:
This requires two pacemaker leads, one in the right atrium and one in the right ventricle. The atrium is stimulated to contract first; then, after an adjustable PR interval, the ventricle is stimulated to contract. DDD is the common type. Dual chamber pacemakers provide the important benefits of maintaining AV synchrony.
4. Rate adaptive pacemakers:
A rate adaptive pacemaker is considered for patients who do not have an appropriate heart rate response to exercise (“chronotropic incompetence”). This syndrome may be due to drug treatment with negatively chronotropic drugs such as Beta-blockers or due to pathologic process such as sick sinus syndrome.
Choice of Pacing Mode
The choice of pacing mode depends on the primary indication for the artificial pacemaker. A rough guideline has been delineated below.
- If the patient has Sino-atrial (SA) node disease and no evidence of disease of the Atrio- Ventricular (AV) node or bundle of His, an atrial pacemaker (AAI) could be placed.
- Accompanying disease of the AV nodal conduction requires a dual-chamber (DDD or DDI) system.
- Patients with sinus node disease, AV node disease, or lower conduction system disease whose heart rate do not respond to an increase in metabolic demands should be considered for placement of a rate-adaptive pacing system.
- Individuals experiencing episodes of symptomatic bradycardia due to SA node or AV node disease may benefit from placement of a single-chamber ventricular (VVI) pacemaker.
- Neurocardiogenic syncope (due to carotid sinus hypersensitivity), vasovagal syncope, and hypertrophic cardiomyopathy can be treated with dual-chamber pacemakers.
- Electromechanical asynchrony and intraventricular conduction block can be treated by cardiac resynchronization therapy using bi-atrial or bi-ventricular pacing.
It is imperative that the anaesthetist recognises those patients who require a prophylactic pacemaker before surgery can proceed. Table 3 summarises the requirement for pre-operative pacing.
Note: For emergency surgery where pacing is indicated but there is insufficient time for temporary or permanent pacing wires, the patient should have external transcutaneous pacing pads attached before surgery.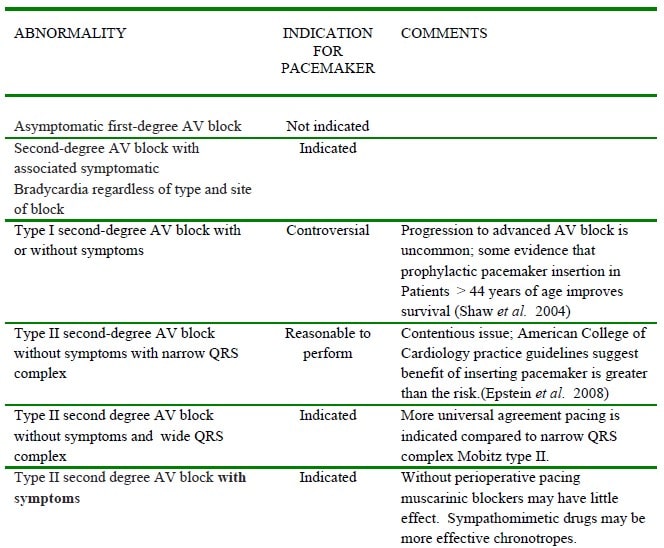
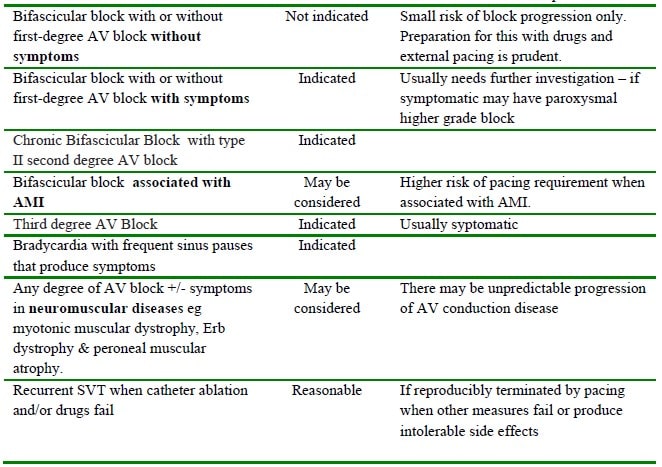
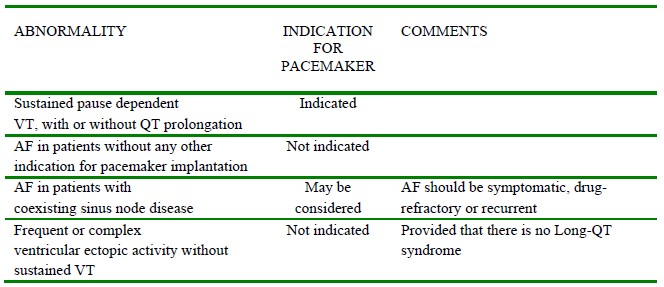
Table 3. Types of ECG abnormality and prophylactic pacemaker indication before anaesthesia. (Modified from Epstein AE et al, 2008). AMI =Acute myocardial infarction.
IMPLANTABLE CARDIOVERTER-DEFIBRILLATOR (ICD)
An ICD responds to dysrhythmia by delivering an internal electrical shock within 15 seconds. The ICD system consists of a pulse generator and leads for dysrhythmia detection and current delivery. In addition to internal defibrillation, an ICD can produce anti-tachycardia and anti-bradycardia pacing and synchronized cardioversion. Detailed diagnostic data concerning intracardiac electrograms and event markers are stored in the memory of the device and can be retrieved for analysis.
Modern ICDs have many programmable features, but essentially they measure each cardiac R-R interval and categorize the rate as normal, too fast (short R-R interval) or too slow. When the device detects a sufficient number of short R-R intervals within a period of time, it will declare a tachycardia episode. The internal computer will decide between anti-tachycardia pacing and shock based on its programmed algorithm.
NASPE/BPEG Generic Defibrillator (NBD) code
Like pacemakers, implantable cardioverter-defibrillators (ICDs) have a generic code to indicate lead placement and function. The NBD code is shown in Table 4.
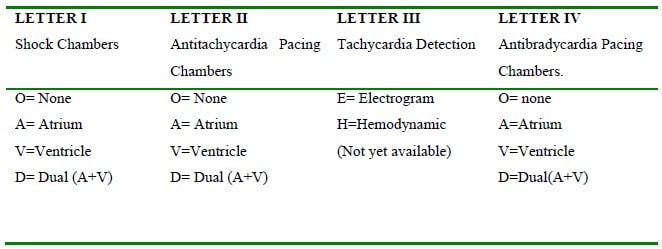
Table 4. NASPE/BPEG Generic Defibrillator (NBD) Code.
Indication for ICDs
Though initially ICDs were indicated for haemodynamically significant ventricular tachycardia (VT) or ventricular fibrillation (VF) but newer indications have been added in the list and continued to evolve (Goldberger Z and Lampert R 2006):
- Cardiac arrest resulting from VT/VF not resulting from a transient or reversible cause
- Spontaneous sustained VT with structural heart disease
- Syncope of undetermined origin with clinically relevant, haemodynamically significant sustained VT or VF induced at electrophysiology study (EPS)
- Ischemic cardiomyopathy (EF ≤30%) without a recent myocardial infarction (within the last 4 weeks) or revascularization in the past 3 months.
- Ischemic or non-ischemic dilated cardiomyopathy (EF ≤35%) with New York Heart Association (NYHA) class II or III heart failure symptoms stable for the past 9 months.
- Brugada syndrome—right bundle branch block (RBBB) and ST segment elevation leads V1 to V3
- Arrhythmogenic right ventricular dysplasia
- High risk patients with Q-T syndrome: High-risk patients are defined as those with aborted cardiac arrest or recurrent cardiac events (eg, syncope or torsade de pointes) despite conventional therapy (i.e. beta-blocker alone) and those with very prolonged QT interval (>500 ms).
- Hypertrophic obstructive cardiomyopathy
REFERENCES and FURTHER READING
- Healey JS et al. Society position statement: Canadian Cardiovascular Society/Canadian Anesthesiologists Society/Canadian Heart Rhythm Societyjoint position statement on the Perioperative management of patients with implanted pacemakers, defibrillators, and neurostimulating devices. Can J Anesth 2012; 59: 394-407.
- American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Cardiac Implantable Electronic Devices. Practice Advisory for the Perioperative Management of Patients with Cardiac Implantable Electronic Devices: Pacemakers and Implantable Cardioverter- Defibrillators. Anesthesiology 2011; 114 (2): 247-261.
- Yao FSF, Fontes ML, Malhotra V. Anesthesiology: Problem oriented patient management. 6th ed. New Delhi: Lippincott Williams & Wilkins (India); 2008.
- Goldberger Z, Lampert R. Implantable cardioverter-defibrillators: expanding indications and technologies. JAMA 2006;295:809-818
- Zipes DP, Libby P, Bonow RO, et al. eds. Braunwald’s heart disease, a textbook of cardiovascular medicine, 6th ed. Philadelphia: WB Saunders, 2005:787-802.
- Salukhe TV, Dob D. Pacemakers and defibrillators: anaesthetic implications. Br J Anaesth 2004;93:95-104.
- Atlee JL, Berstein AD. Cardiac rhythm management devices (part I). Anesthesiology 2001;95:1265- 1280
- Hines RL, Marschall KE. Stoelting’s Anesthesia & Co-Existing Disease. 5th ed. Nodia: Elsevier; 2009.
- Shinbane JS, Colletti PM, Shellock FG. Magnetic resonance imaging in patients with cardiac pacemakers: era of “MR Conditional” designs. Journal of Cardiovascular Magnetic Resonance 2011; 13(63) W457- 459.
- Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 Guidelines for Device- Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices): developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. Circulation 2008;117:e350–408
- Shaw DB, Gowers JI et al. Is Mobitz type 1 atrioventricular block benign in adults? Heart 2004; 90 (2): 169-174



