Basic Sciences
QUESTIONS
This is the second of a two-part tutorial which discusses anaesthesia for patients with cardiac pacemakers and implantable cardioverter-defibrillators (ICD), collectively termed cardiac implantable electronic devices (CIEDs). Below are the questions published in part one. The answers, together with an explanation can be found at the end of this tutorial.
- Which of the following statements are correct regarding pre-operative pacing?
a. If a patient presenting for elective surgery is found pre-operatively to have bifascicular block with 1st degree AV block, the patient should have a transvenous pacemaker before the operation irrespective of cardiovascular symptoms.
b. If a patient presenting for emergency surgery has symptomatic third degree heart block, the patient should always have a permanent pacemaker inserted before the surgery can safely proceed.
c. Asymptomatic Type II second degree AV block is NOT an indication for preoperative pacemaker insertion before elective surgery.
d. Asymptomatic First degree AV block is extremely unlikely to progress to second degree block in the perioperative period. As a result they do not require pre-operative pacing. - List 5 potential adverse events that may arise if a patient with an implanted pacemaker is exposed to a MRI?
- Which of the following statements are true regarding the perioperative management of pacemakers and ICDs?
a. A Magnet placed over a pacemaker device is a recommended alternative to formal device re-programming before an operation involving diathermy.
b. If a pulseless shockable rhythm occurs intra-operatively in a patient with a programinactivated Implantable Cardioverter – Defibrillator (ICD), the first step would be to page the cardiology technician to re-enable the ICD.
c. If a pulseless shockable rhythm occurs intra-operatively in a patient with an implanted pacemaker, the patient should be immediately externally defibrillated using standard energy levels.
d. On an X-ray film, one can most reliably distinguish between an ICD and a permanent implantable pacemaker (PPM) by looking at the generator box.
ANAESTHESIA FOR PATIENTS WITH IMPLANTABLE CARDIAC DEVICES
The presence of an artificial cardiac pacemaker or ICD in a patient scheduled for surgery unrelated to the device introduces special considerations for preoperative evaluation and subsequent management of anaesthesia.
PREOPERATIVE EVALUATION
In addition to the routine systematic workup (paying particular attention to cardiovascular status), the anaesthetist needs to establish the presence and location of the CIED and the reason for its insertion. This is achieved by taking a focused history including review of the medical records. Physical examination should include a search for scars over the chest and upper abdomen and a chest X-ray confirms the presence and location of device. The anaesthetist then needs to answer the following questions:
- What is the type of the device and program mode?
- Is the device functioning properly?
- How dependent is the patient on the device (as an anti-bradycardia function)?
- What is the probability of electromagnetic interference in theatre and how do we minimise the risk?
1. Defining the type of device
This might be accomplished by:
- Obtaining the manufacturer’s identification card from the patient or other source
- Ordering chest x-ray studies if no other data are available. The presence of shocking coil(s) in the right ventricle and sometimes also in the superior vena cava indicates an implanted ICD. (Healey JS et al. 2012)
- Referring to supplemental resources like vendor’s database, pacemaker clinic records,
consultation with cardiologist
2. Determining if the device is functioning properly
Pacemakers can fail early or late after insertion. Early failure is often due to displaced or broken electrodes whereas late failure is often attributed to premature battery failure. The pacemaker function should be checked where possible by the pacemaker technologists who can interrogate the device before proceeding to surgery. If interrogating the device is not an option, one can slow the intrinsic heart rate to a rate below that of the pacemaker by carotid massage or a Valsalva; a functioning pacemaker will then takeover the heart rate.
If the rate does not slow down enough for the pacemaker to take over the ventricle, common practice used to be to test the device by placing a magnet over it to convert it to a fixed-rate pacing mode. In this mode, pacing spikes march through the rhythm strip with no regard for the intrinsic electrical activity of the heart. However, magnets are not recommended, as the pacemaker response to a magnet is unpredictable and maybe hazardous to the patient (see below).
3. Determining patient’s dependency on CIEDs
Patients’ dependency on pacemaker or ICD can most reliably be determined by consultation with the cardiologist or pacemaker technician, however pacemaker dependency may also be suggested by one or more of the following:
- A verbal history or an indication in the medical record that the patient has experienced a bradyarrhythmia that has caused syncope or other symptoms requiring CRMD implantation.
- A history of successful atrioventricular nodal ablation that resulted in CRMD placement
- A CIED evaluation that shows no evidence of spontaneous ventricular activity when the pacemaker function of the CIED is programmed to VVI pacing mode at the lowest programmable rate (ASA taskforce special article, 2011).
- The ECG will show pacing spikes if the patient is dependent on the pacing function.
4. The Probability of electromagnetic interference intra-operatively.
The main concern of electromagnetic interference (EMI) in patients with implanted cardiac devices is pacemaker malfunction or (rarely) burn to the myocardium or even VF. With regard to pacemaker malfunction, the effect could be:
-
- Inhibition of pacing
- Asynchronous pacing
- Reset to Back-up mode
In addition to this, EMI in patients with ICDs can cause inappropriate or inhibition of tachycardia therapy. Sources of electromagnetic interference are explained in the section below.
ELECTROMAGNETIC INTERFERENCE
The principle sources of EMI that affect implantable devices are found within the hospital environment. Radio frequency waves with frequencies between 0 and 109 Hz (e.g. AC power supplies and electrocautery) and microwaves with frequencies between 109 and 1011 Hz (including ultra high frequency radio waves and radar) can cause device interference. Higher frequency waves such as Xrays, gamma rays and infrared and ultraviolet light do not cause interference. If EMI is likely to occur during surgery, pre-operatively the conventional pacing function of a pacemaker should be altered by changing to an asynchronous pacing mode and suspending special algorithms, including rate-adaptive functions.
The three groups of patients most at risk from EMI interference are:
- Patients who have a pacemaker dependent rhythm (eg complete AV block may become severely bradycardic or asystolic from EMI).
- Patients with an ICD (should have anti-tachyarrhythmia functions suspended).
- Patients with pacemakers with a rate-responsive function (eg those triggered by respiration).
Electrocautery/diathermy
Electrocautery remains one of the most common causes of EMI; it uses radio frequency current to cut or coagulate tissues and is usually applied in a unipolar configuration between the handheld instrument (cathode) and the anode plate attached to the patient’s skin. The radio frequency is usually between 300 and 500 kHz. The EMI generated by electrocautery that may affect the device is related to the distance and orientation of the current to the patient’s device and leads. Measures to reduce the risk of EMI should be applied (see below).
External defibrillators
One of the largest amounts of electrical energy to which implanted devices may be exposed is from external cardioversion or defibrillation. Such energies are liable to damage generator circuitry and cardiac tissue in contact with leads. The high energies involved in cardioversion/defibrillation may override these mechanisms. More commonly, backup or reset modes are activated. For generators positioned in the left pectoral region, apex-anterior or apex-posterior positions are advised. For generators positioned in the right pectoral region, apex-posterior positions are more appropriate.
Radiofrequency (RF) ablation.
Transvenous radiofrequency ablation is a common therapy in patients with dysrhythmias associated with accessory pathways or ectopic foci. General consensus is to ensure the RF ablation cluster electrode is placed as far as possible away (at least 5 cm) from the device or leads (ASA taskforce, 2011).
Transcutaneous electrical nerve stimulation
Transcutaneous electrical nerve stimulation (TENS) is a widely used method of analgesia. The unit delivers electrical impulses via several skin electrodes at a frequency of 20-110 Hz in rectangular pulses of 1-200 V at 0-60 mA. Each pulse lasts 20 ms. This electrical impulse theoretically may cause pacemaker inhibition. In general, TENS can be used safely in patients with bipolar pacemakers and defibrillators, although use in close proximity to the device is not advised.
Electroconvulsive therapy (ECT)
ECT appears safe for patients with pacemakers because little current flows within the heart due to high impedance of body tissues. However, the seizure and succinylcholine fasciculations may generate sufficient myopotentials for pacemaker inhibition (unipolar devices) or ventricular tracking (adaptiverate devices). It is advisable to consult with the ordering physician, the patient’s cardiologist, a cardiac rhythm management device (CRMD) service or the device manufacturer. It might be required to program the pacemaker to nonsensing mode for a pacemaker-dependent patient. All ICDs should be programmed so that tachycardia detection is disabled before ECT and reprogrammed to its original programmed parameters afterwards. Presence of external pacemaker should be made available.
Extracorporeal shockwave lithotripsy
ESWL is no longer contraindicated for patients with pacemakers. The only exception to the general statement is the abdominally placed pacemaker generators which are placed in the blast path of shock wave. Although most pacemakers are not affected by ESWL, sometimes it may cause pacemaker malfunctions that include the following:
- Switching to magnet mode (Yao FSF, 2008)
- Reaching upper rate limit
- Pacing irregularly
- Over-sensing of asynchronous shocks
- Damage to rate-sensing piezoelectric crystal
- Intermittent inhibition of ventricular output in dual-chamber pacemaker
- Electromagnetic interference.
A dedicated pacemaker programmer should be available in the lithotripsy suite should pacemaker malfunction be caused by the shock waves. In addition, an alternative means of pacing, such as transcutaneous pacing, should also be available in case the pacemaker becomes permanently damaged. It is best to disable tachycardia detection of an ICD during ESWL and to thoroughly test ICD following the procedure. Finally, lithotripsy often triggers on the R-wave; as a result, some suggest disabling the atrial pacing before the procedure.
Radiation therapy.
To avoid potential pacemaker failure and runaway pacemaker, the generator device should be outside the field of radiation (ASA taskforce, 2011). Occasionally, this may mean surgical relocation of the device before radiation therapy can start.
Magnetic Resonance Imaging
During magnetic resonance imaging (MRI), a large magnetic field is generated with an electromagnet. Potential adverse events can occur and are seen in table 1:
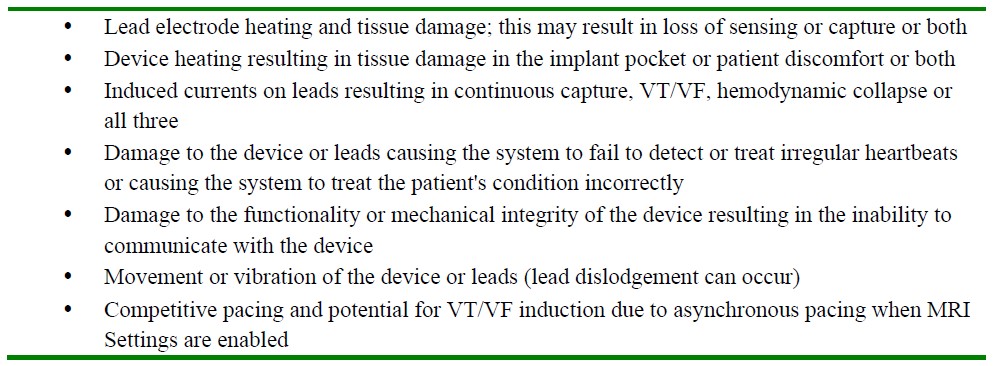
Table 1: Potential adverse events if a patient with an implanted pacemaker is exposed to a MRI (adapted from the MRI Procedure Information for the St. Jude Medical™ MR Conditional Pacing System)
For these reasons, traditionally the presence of a CRMD was an absolute contraindication to entering the MRI room. Recent Advances in cardiac device technology however have led to the first generation of MRI conditional devices (Shinbane J et. al. 2011).
If a patient with a CRMD is being considered for an MRI, not only is it imperative that the device itself is “MR conditional”, but the leads also need to be designed for use in an MRI. Consultation with the MRI technologist, cardiac pacemaker technologist and cardiologist is imperative before a patient is allowed to enter the scanner. If MRI is considered absolutely essential, often the device has an “MRI mode” for which could be activated before entering the magnet room. This may involve reprogramming the pacemaker to its lowest voltage and pulse width or to OOO mode, provided the patient has an adequate underlying rhythm. In addition to adequate monitoring facilities and resuscitation equipment, an external defibrillator with pacing facility should be available (but kept outside the scanning room).
Overall, if a patient is likely to be exposed to EMI, pre-operative consultation with the cardiologist/pacemaker technician is essential. From the cardiology department, it is reassuring to have knowledge that the pacemaker is functioning well preoperatively and the battery is not running out. Reliable information can be obtained with regard to the patient’s dependence on the pacemaker/ICD and a decision can be made as to whether reprogramming the pacing function to an asynchronous mode or disabling the rate responsive function is advantageous. In addition, the anti-tachyarrhythmia function (if present) could be suspended.
If the pacemaker technician/cardiologist is not available, an alternative (although not recommended) is to place a magnet over the device.
Effect of a magnet over pacemakers and ICDs
A magnet correctly applied to a pacemaker often results in asynchronous fixed-rate pacemaker function at a predetermined rate without rate responsiveness. Unfortunately in practice the effect of the magnet is variable; the pacemaker response varies depending on manufacturer, specific programming and remaining battery life. In addition, the “magnet rate” may also be too fast for some patients and some pacemakers may have no (or temporary) magnet response.
The response of an ICD to a magnet placement is different from the response of a pacemaker. Magnets will often disable tachyarrhythmia detection and therapy which are enabled when the magnet is removed. Magnets rarely alter bradycardia pacing rate and function. As with magnets and pacemakers, there are potential disadvantages in using magnets with ICDs; for most ICDs, there is no reliable means to detect appropriate magnet placement. In addition, some ICDs may have no response to a magnet or the device can be permanently disabled. It is for this reason, the ASA taskforce (2011) cautions against the routine use of magnets with ICDs.
If a magnet is used, the effect of a magnet on a pacemaker or ICD should be always checked before proceeding to surgery or other procedures.
In addition to the cardiology department, the anaesthetist should liaise with the proceduralist to reduce the risk of electrocautery. To reduce the risk, bipolar diathermy (or even ultrasonic/harmonic scalpel) is considered a safer alternative to unipolar diathermy. If unipolar diathermy has to be used, the cautery tool and return pad should be positioned so that the current does not pass near the implanted device or leads. This is probably the safest practice although good evidence for this is lacking and electromagnetic interference may still occur. There is some evidence that infrequent short bursts at the lowest feasible energy may reduce EMI. Temporary pacing and defibrillation equipment should be available in the perioperative period.
INTRAOPERATIVE MANAGEMENT
Management of anesthesia in patients with artificial cardiac pacemakers includes (1) proper intraoperative monitoring and (2) ensuring the availability of equipment and drugs to maintain an acceptable intrinsic heart rate should the artificial cardiac pacemaker or ICD unexpectedly fail.
Monitoring
Intraoperative monitoring should include both continuous ECG and peripheral pulse monitoring/pulse oximetry. The “artifact filter” on the ECG monitor should be disabled in order to detect the pacing spikes because Some IEDs may produce artifacts and interfere with the recording of an ECG. The ECG monitor should be kept in diagnostic mode instead of monitoring mode because the former has got wider frequency response range (0.05-100 Hz) which enables assessment of QRS morphology and more accurate ST segment analysis.
Drugs & Equipment
A complete array of drugs and equipment must be immediately available for cardiopulmonary resuscitation. The minimal requirements include, ECG monitor, a transcutaneous external pacing and DC defibrillator, and the usual drugs for resuscitation.
Emergency defibrillation
Defibrillation in a patient with a permanent cardiac pacemaker is managed in the conventional manner with standard energy levels and defibrillation pads placed far away from the device (antero-posterior is the most common pad position).
If the patient has an ICD, some specific actions depend on whether the device has been magnet disabled or programming disabled preoperatively. In either case, the first step is to advise the proceduralist to terminate all sources of electromagnetic interference.
- If the ICD has been magnet disabled, the magnet should be removed to re-enable antitachycardia therapies. The patient and monitoring should then be observed for the ICD to perform appropriate cardiac rhythm therapy; 10-12 seconds should allow enough time for the ICD to charge. If ICD function has not been restored, emergency external defibrillation/cardioversion would be required (as described above).
- If the ICD has been programming disabled, the device should be reprogrammed to enable therapies if the programmer is immediately available. As above, wait for 10-12 seconds while the ICD charges and initiates a shock. If the programmer is not immediately available or if the ICD fun
The anaesthetist should be prepared to provide external transcutaneous pacing following shock delivery (see below).
Transcutaneous Cardiac Pacing
Patient with symptomatic bradycardia or severe conduction block require immediate pacing. Transcutaneous pacing is a recommended treatment for symptomatic bradydysrhythmia with a pulse. The cutaneous chest and back electrodes are placed over areas of lesser skeletal muscle mass and lowdensity constant-current impulses should be delivered. This improves the likelihood of effective cardiac stimulation and minimizes painful skeletal muscle or cutaneous stimulation. Transcutaneous pacing should be considered a temporizing measure until transvenous cardiac pacing can be instituted.
Impact of Anaesthetic drugs or techniques on CRMD function
There is no evidence that anaesthetic drugs alter the stimulation threshold of artificial cardiac pacemakers. But it is advisable not to use nitrous oxide in a patient with newly implanted pacemaker as it causes an expansion of gas in the pocket, which leads to loss of anodal contact and pacing system malfunction.
It is also prudent to avoid hyperventilation as the alkalosis could acutely change the serum potassium concentrations which ultimately can alter the threshold of cardiac pacemakers.
Factors which may alter the threshold of cardiac pacemakers:
- Hyperkalemia
- Hypokalemia
- Arterial hypoxemia
- Myocardial Infarction
- Catecholamines
Succinylcholine could interfere with the stimulation threshold of CRMD because:
- It could increase in stimulation threshold due to acute increase in serum potassium concentration.
- Contraction of skeletal muscle groups (myopotentials) could inhibit the pacemaker.
Clinical experience however suggests that suxamethonium is usually a safe drug in the patient with a pacemaker or ICD despite inhibition of CRMD function, as the effect is transient.
Postoperative management
Cardiac rate and rhythm should be continuously monitored throughout the immediate postoperative period. Back-up pacing capability and cardioversion-defibrillation equipment should be immediately available at all times.
Postoperative interrogation and restoration of CRMD function is an essential part of postoperative management; this usually requires a pacemaker technician. For an ICD, all anti-tachyarrhythmic therapies should be restored.
SUMMARY
The assessment and management of a patient who has an implanted cardiac device requires special attention and necessitates specific precautions. Consultation and co-ordination with cardiologist, pacemaker technician and proceduralist is the key avoiding perioperative complications in these patients. The anaesthetist should know how to safely manage perioperative dysrhythmias with drugs, external pacing and defibrillation.
ANSWERS TO QUESTIONS.
- ..
a. False: if the patient is asymptomatic, perioperative pacing is not required for patients with bifascicular block with 1st degree AV block (incorrectly termed “trifascicular block”). If the patient is symptomatic, this indicates there may be intermittent higher grade block which often requires further investigation and perioperative pacing.
b. False: Although desirable, permanent pacemaker insertion is not always possible before emergency surgery; however either temporary transvenous pacing with an external generator or external pacing pads should be in place before surgery.
c. False: It is not universally agreed, however The American guidelines suggest the risk:benefit ratio for pacemaker insertion is in favour of pacing for both narrow and broad QRS complex type II second degree AV block before elective surgery.
d. True - See Table 1
- ..
a. False: Pacemaker companies and specialists do NOT recommend magnet placement over a device. If a magnet is used, the results are not 100% predictable for both pacemakers and ICDs.. Pacemakers have no “standard” response to magnet placement; it does not always place the pacemaker in an asynchronous mode, it may re-program the device and it may run the risk of pro-arrhythmic “R on T” phenomenon. It is much better for the device to be altered by a cardiology technologist (unless advised to place a magnet by the treating cardiologist or pacemaker specialist).
b. False: In this scenario, the device should be re-enabled if the technologist is immediately present, however if not, the patient should be externally defibrillated. Similarly, in a situation where the ICD was magnet disabled (not recommended), the magnet should first be removed to re-enable the ICD. If the patient is not shocked by the device within 12-15 seconds, then conventional external defibrillation should be performed.
c. True: Although it should be remembered that the pads should be placed as far from the device as possible; antero-posterior pad positioning is the most common.
d. False: The Shocking coil is the most reliable indicator of the type of device, not the generator itself.
REFERENCES and FURTHER READING
- Healey JS et al. Society position statement: Canadian Cardiovascular Society/Canadian Anesthesiologists Society/Canadian Heart Rhythm Societyjoint position statement on the Perioperative management of patients with implanted pacemakers, defibrillators, and neurostimulating devices. Can J Anesth 2012; 59: 394-407.
- American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Cardiac Implantable Electronic Devices. Practice Advisory for the Perioperative Management of Patients with Cardiac Implantable Electronic Devices: Pacemakers and Implantable Cardioverter-Defibrillators. Anesthesiology 2011; 114 (2): 247-261.
- Yao FSF, Fontes ML, Malhotra V. Anesthesiology: Problem oriented patient management. 6th ed. New Delhi: Lippincott Williams & Wilkins (India); 2008.
- Goldberger Z, Lampert R. Implantable cardioverter-defibrillators: expanding indications and technologies. JAMA 2006;295:809-818
- Zipes DP, Libby P, Bonow RO, et al. eds. Braunwald’s heart disease, a textbook of cardiovascular medicine, 6th ed. Philadelphia: WB Saunders, 2005:787-802.
- Salukhe TV, Dob D. Pacemakers and defibrillators: anaesthetic implications. Br J Anaesth 2004;93:95-104.
- Atlee JL, Berstein AD. Cardiac rhythm management devices (part I). Anesthesiology 2001;95:1265-1280
- Hines RL, Marschall KE. Stoelting’s Anesthesia & Co-Existing Disease. 5th ed. Nodia: Elsevier; 2009.
- Shinbane JS, Colletti PM, Shellock FG. Magnetic resonance imaging in patients with cardiac pacemakers: era of “MR Conditional” designs. Journal of Cardiovascular Magnetic Resonance 2011; 13(63) W457- 459.
- Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices): developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. Circulation 2008;117:e350–408
- Shaw DB, Gowers JI et al. Is Mobitz type 1 atrioventricular block benign in adults? Heart 2004; 90 (2): 169-174



