Basic Sciences
Self assessment:
Complete these questions before reading the tutorial. Discuss the answers with your colleagues.
- How long should children be fasted pre-operatively?
- For what reasons may you need to give fluids intra-operatively?
- How do you calculate fluid requirements?
- What is the maintenance requirement for:
- a 3 day old 3 kg neonate
- a 16 kg child
- a 44 kg child
- Define isotonic and hypotonic
- List the intravenous fluids you know. Which are isotonic, which are hypotonic?
- What factors may cause hyponatraemia peri-operatively?
- What are the signs and symptoms of hyponatraemia?
- Which children are at risk of hypoglycaemia?
- What fluids can you use for:
- maintenance infusion?
- correction of hypovolaemia?
- replacement of intraoperative losses
Introduction
The majority of fit paediatric patients undergoing minor surgery will not require intravenous fluids per-operatively.
These patients should be kept nil by mouth as short a time as possible to minimise the discomfort of hunger and thirst. In elective surgery clear fluids should be allowed up to 2 hours pre-operatively, breast milk to 3 hours. All other food or fluids (including formula milk) should be withheld for 6 hours pre-anaesthetic.
Patients undergoing longer or more major procedures, or who are compromised by an underlying illness will need intravenous fluids.
When should fluids be given?
Fluids are given for three reasons: resuscitation, maintenance or replacement of ongoing losses.
Resuscitation of a dehydrated or hypovolaemic patient should occur prior to surgery where possible to ensure an adequate circulation before giving an anaesthetic.
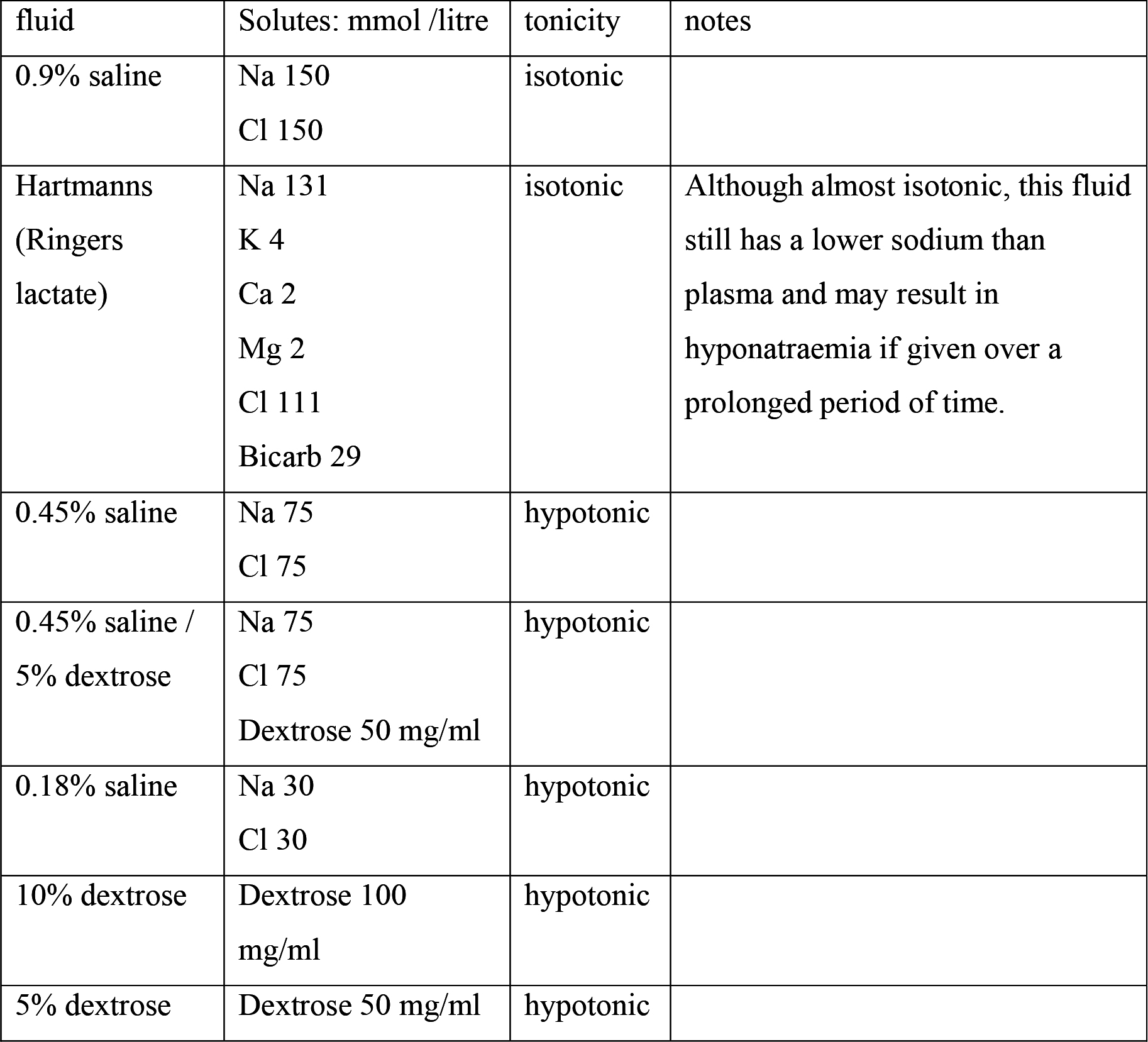
Hypovolaemia may be corrected rapidly using isotonic saline (0.9%), colloid or blood as appropriate. Dehydration should be corrected more slowly (over 24-48 hours) and preferably with oral fluids. The choice of intravenous fluid used will depend on the measured plasma sodium. Too rapid correction with hypotonic fluid may cause hyponatraemia and result in cerebral oedema which can be fatal.
Maintenance may be with any clear fluid. However some of these are hypotonic solutions which may cause hyponatraemia if given in large amounts or over a long period of time.
An isotonic fluid contains the same amount of solute as plasma so exerts an equal osmotic force. e.g. 0.9% saline or Hartmanns solution (Ringers lactate). Dextrose is metabolised in blood, so although 5% dextrose is isosmolar to plasma, once metabolised it becomes effectively free water. 0.45% or 0.18% saline, and dextrose solutions are therefore hypotonic.
When the body is subject to stress such as surgery, pain, nausea or hypovolaemia, levels of antidiuretic hormone (ADH) rise. This causes water retention by the kidneys which dilutes and lowers plasma sodium levels. A rapid or large drop in sodium results in cell swelling and oedema. This can manifest as raised intracranial pressure, coning and death.
This suggests that perioperative maintenance fluids should be given as 0.45% saline, 0.9% saline or Hartmanns. Hypotonic fluids should not be used if the sodium is less than 140 mmol/l. If the plasma electrolyes are not known it is probably safer (in the short term) to give 0.9% saline to a patient with a high sodium, than to give hypotonic fluids to a hyponataemic patient. Hypotonic fluids should not normally be given at greater than maintenance rates (except in neonates, see below).
Replacement of ongoing losses during or after surgery should be with an isotonic fluid, colloid or blood. Increased fluid evaporation occurs in pyrexia, from an open wound (up to 20 ml/kg/hour) or by breathing dry anaesthetic gasses. Respiratory fluid loss can be reduced by using a circle system or HME (heat moisture exchanger).
Blood or other fluid loss may be difficult to measure and the clinical state should be monitored continuously (heart rate, capillary refill time and blood pressure). In a warm, stable child with good analgesia increased heart rate and prolonged capillary refill time indicate fluid loss. Hypotension occurs relatively late when due to hypovolaemia.
When should dextrose solutions be used?
Dextrose may be required to prevent hypoglycaemia while the child is fasted for theatre. However the stress response to starvation and surgery causes a rise in blood sugar, and per-operative hypoglycaemia is actually rare in most children, even those not given dextrose fluids. The exceptions to this are: neonates less than 48 hours old; neonates who have a dextrose infusion stopped; and children below the 3rd centile in weight. These children should be given dextrose maintenance infusions without prolonged interruption. The choice of dextrose containing fluid will depend on local preference and measured blood glucose and electrolytes. Premature neonates may need 10% dextrose, older babies 5% dextrose. This may be with saline 0.45% (or 0.9% if the sodium is low). Most other children can be given dextrose-free fluid. Any child thought to be at risk of hypoglycaemia should have their blood glucose checked regularly.
Calculation of fluids
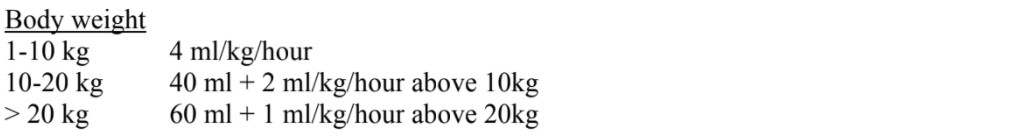
Maintenance fluid rate may be calculated many different ways. A simple method follows:
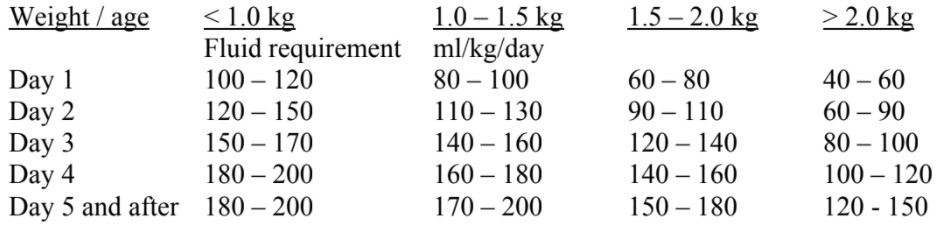
Neonates (up to 44 weeks post conceptual age) have different requirements. They are born physiologically “waterlogged” then lose this fluid over the first week of life.
Premature or small babies have a larger surface area to weight ration so will lose more fluids by evaporation and therefore have higher maintenance requirements. This fluid is usually given as 10% dextrose with or without saline to maintain blood sugar.
Post-operative fluids and monitoring
Monitoring of fluid status should continue post-operatively. Maintenance fluids should be continued until the child is able to take adequate amounts orally. Ongoing losses should be measured and replaced.
Symptoms of raised intracranial pressure include nausea, vomiting, reduced consciousness, respiratory depression and seizures. Nausea, vomiting and drowsiness may be attributed to the side effects of surgery, anaesthesia and analgesia but by the onset of seizures and respiratory depression due to hyponatraemic encephalopathy, it may be too late.
Suggested fluid regime
- Maintenance infusion calculated on weight basis using 0.9% or 0.45% saline.
- Additional fluid to correct deficits, measured or suspected ongoing losses: 0.9% saline, colloid or blood.
- Dextrose if neonate, malnourished or a measured blood sugar is low. Give as 5% or 10% dextrose at 120 mg/kg/hour.
Conclusions:
- The majority of fit paediatric patients undergoing minor surgery will re-establish oral intake in the early postoperative phase and will not need routine intravenous fluids.
- Hypotonic fluids should be used with care and must not be infused in large volumes or at greater than maintenance rates.
- Hypovolaemia should be corrected with rapid infusion of isotonic saline, while dehydration is corrected more slowly over 14-72 hours as appropriate.
- Ongoing losses should be measured and replaced.
- Plasma electrolytes and glucose should be measured regularly in any child requiring large volumes of fluid or who remains on intravenous fluids for more than 24 hours.
Further reading
- Wilson CM. Perioperative fluids in children. Update in Anaesthesia Issue 19 (2005) www.world-anaesthesia.org.
Answers to questions:
- How long should children be fasted for pre-operatively?
- See text
- For what reasons may you need to give fluids intra-operatively?
- Resuscitation, maintenance and replacement. See text
- How do you calculate fluid requirements?
- The “4-2-1 rule” is a quick method for calculating fluids except in neonates who have different requirements. See text.
- What is the maintenance requirement for:
- a 3 day old 3 kg neonate
- 80-100 ml/kg/24 hours. See table.
- a 16 kg child
- 52 ml/hour. [40ml + (2 x 6ml)]. See text.
- a 44 kg child
- 84 ml/hour. [60ml + (24 x 1ml)]. See text.
- Define isotonic and hypotonic
- an isotonic fluid exerts the same osmotic force as plasma. A hypotonic fluid exerts a lower osmotic force than plasma. This is either because the concentration of solutes is lower than in plasma, or because the solute is metabolised, diluting the plasma and leaving free water to move into cells. This may result in hyponatraemia (a low plasma sodium).
- List all the fluids you know. Which are isotonic, which are hypotonic?
- What factors may cause hyponatraemia peri-operatively?
- Stress causing a rise in ADH levels and water retention. Rapid infusion of hypotonic fluids (at greater than maintenance rates). Prolonged infusion of hypotonic fluids. NB prolonged infusion of isotonic fluids may also result in hypernatraemia. Any patient on intravenous fluids should have their plasma electrolytes checked on a regular basis (at least every 24 hours).
- What are the signs and symptoms of hyponatraemia?
- Oedema, including cerebral oedema. The signs of raised intracranial pressure may be mistaken for the side effects of anaesthesia. See text.
- Which children are at risk of hypoglycaemia?
- See text
- What fluids can you use for:
- maintenance infusion?
- correction of hypovolaemia?
- replacement of intraoperative losses
- See text.
Please e-mail any questions to: catharinewilson@yahoo.co.uk



