General Topics
KEY POINTS
- Bariatric surgery is the most effective treatment for morbid obesity resistant to conservative measures. Multiple comorbidities such as diabetes, hypertension, obstructive sleep apnoea, depression and arthritis are common and difficult to optimise.
- Anaesthetists are often challenged by difficult intravenous access, safe airway management, safe patient transfer, drug dosing and the assessment and treatment of the unwell obese patient.
- ‘Ramping’ for safe airway management, drug dosing based on ideal and adjusted body weight, use of multimodal analgesia with titration of opioids, prevention and treatment of postoperative nausea and vomiting and facilitation of early mobilisation underpin the clinical anaesthesia practice.
INTRODUCTION
Overweight and obesity are defined as abnormal or excessive fat accumulation that can impair health. Once considered a problem of high-income countries, overweight and obesity are now a global epidemic, with tripling of obesity rates since 1975 in low- and middle-income countries and 2.8 million deaths attributed to it each year.1
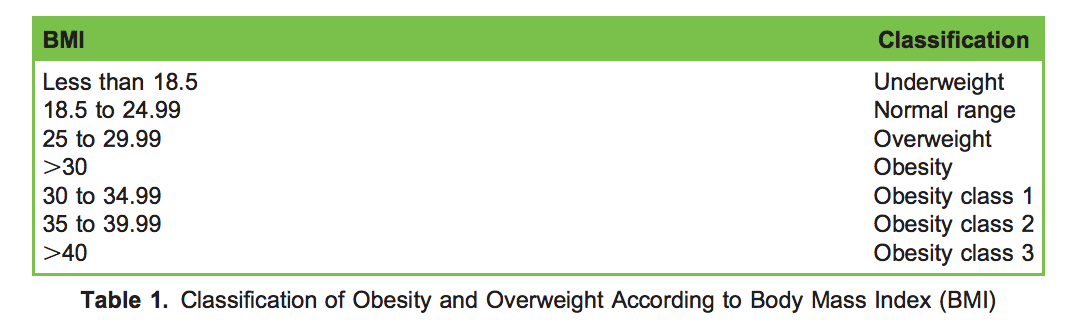
Obesity is a result of several factors: genes, diet, levels of physical activity and the surrounding environment, as well as social and cultural factors. Obesity increases the risk of, and is associated with, several comorbidities including cardiovascular disease, hypertension, diabetes, musculoskeletal disorders, obstructive sleep apnoea (OSA), dyslipidaemia, gastrooesophageal reflux disease (GORD), cancers, depression and anxiety. Severely obese individuals have increased risk of hospitalisation and need for social care, resulting in increased cost of health care. Body mass index (BMI; weight in kilograms divided by the square of height in metres, kg/m2 ), is commonly used to classify overweight and obesity in adults (Table 1).
Bariatric surgery is the most effective and safe treatment for morbid obesity, particularly when conservative measures of weight management have failed, with established safety and significant regression of obesity-associated diseases such as diabetes and hypertension.2–5 Globally, more than 800 000 operations performed from 61 countries have been reported by the International Federation for the Surgery of Obesity and Metabolic Disorders.6 The median age of operative candidates was 43 years, the median BMI was 44.3 kg/m2 , and 77.1% were women, with a wide variation in country-specific gender ratios and BMI. Preoperatively, 23.3% had diabetes, 41% hypertension, 16.5% depression, 25% GORD and 18% sleep apnoea.
More than 90% of the operations were performed laparoscopically, with a median stay of 2 days or less. Average weight loss was 31.1% 1 year after surgery, and 64.2% of patients taking medication for type 2 diabetes no longer needed their medication; this correlated with the amount of weight loss achieved. There were similar reductions in the need for medication for hypertension and dyslipidaemia (45.4% and 51.8%, respectively, no longer required their medication). Patients also saw an improvement in other obesity-related conditions such as sleep apnoea, gastroesophageal reflux disorder and quality of life, with variations amongst regions and operations. Similar outcomes have been reported by the UK National Bariatric Surgery Register. The perioperative care of a bariatric surgery patient is provided by a multidisciplinary team including surgeons, anaesthetists, specialist nurses, dieticians, psychologists, nutritionists and physiotherapists.
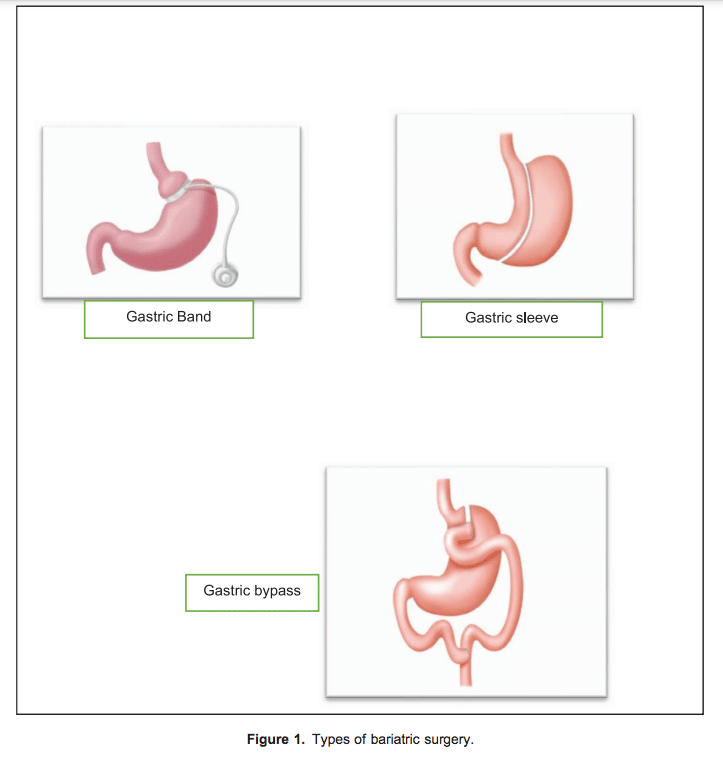
There are 2 main categories of operation (Figure 1)7 :
- Restrictive: the inflatable gastric band is placed around a small pouch of the stomach to reduce the size of the stomach.
- Malabsorptive:
- Roux-en-Y gastric bypass, considered the gold standard of weight loss surgery;
- Laparoscopic sleeve gastrectomy, performed by removing approximately 80% of the stomach;
- Biliopancreatic diversion with duodenal switch (BPD/DS), a procedure with 2 components: a smaller, tubular stomach pouch with a large portion of the small intestine bypassed.
The 3 most commonly performed operations are laparoscopic adjustable gastric banding (band), laparoscopic gastric bypass (bypass) and laparoscopic sleeve gastrectomy (sleeve). All lead to weight loss, but they are associated with different problems. In addition, there is currently no evidence/recommendation for a preferred technique.
The By-Band-Sleeve study,8 a UK-based multicentre randomised trial, is currently under way. Its aim is to compare the effectiveness, cost-effectiveness and acceptability of the 3 techniques, 3 years after randomisation, on weight loss and a wide range of symptoms and aspects of quality of life. The investigators will also study patient-reported outcomes, nutritional outcomes, short- and long-term surgical complications and value for money.
PREOPERATIVE ASSESSMENT AND OPTIMISATION
As obesity is associated with several serious comorbidities, preoperative assessment should look to identify, assess and optimise treatment for hypertension, diabetes, heart failure, OSA, pulmonary hypertension and ischaemic heart disease. In addition a thorough history should be obtained and a thorough examination conducted.
A focused airway assessment should be performed and pharmacologic prophylaxis against aspiration should be considered with proton pump inhibitors and/or ranitidine. Weight and routine observations such as heart rate, blood pressure, temperature, respiratory rate and peripheral oxygen saturation (SpO2) on air should be recorded. Investigations should include but not be limited to baseline 12-lead electrocardiogram (ECG), full blood count, fasting blood glucose and kidney and liver function tests. Patients should also be screened for micronutrient deficiency and long-term metabolic problems, particularly vitamin D and iron deficiencies, with input from a bariatric nutritionist or physician.
This cohort of patients possess significant risk factors for cardiovascular disease; however, traditional noninvasive cardiac imaging modalities, such as echocardiography, cardiac computed tomography and cardiac magnetic resonance can all be challenging, and there are currently no recommendations or guidelines to assess cardiovascular disease in the obese population. Myocardial perfusion scan and exercise stress testing should be considered in selected patients.
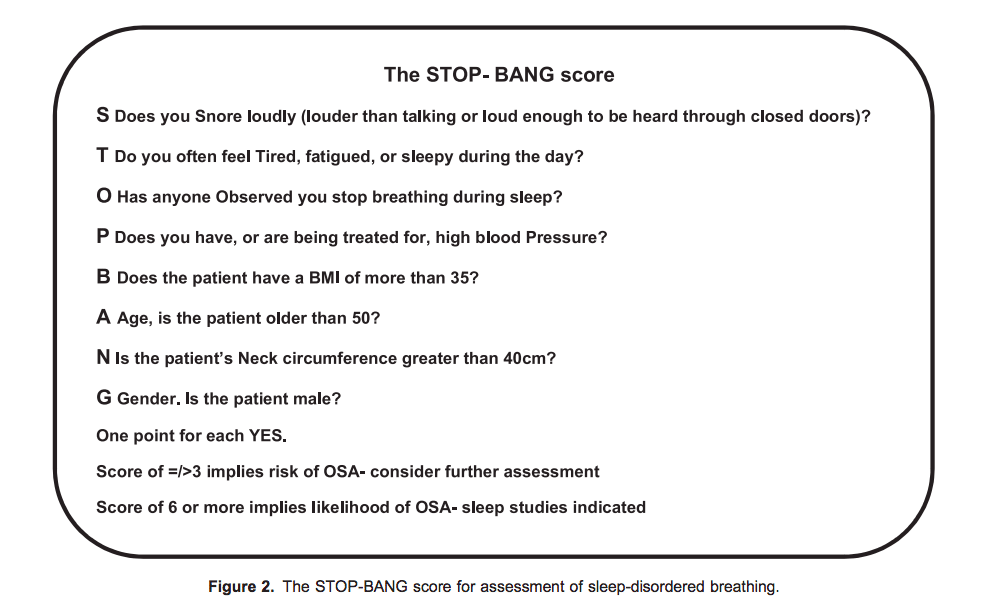
The STOP-BANG questionnaire (Figure 2) is a validated tool to screen for OSA/sleep-disordered breathing, and sleep studies should be organised if indicated. (Please see Tutorial 360 on perioperative management of adults with known or suspected sleep apnoea for elective and emergency surgery). Preoperative use of continuous positive airway pressure (CPAP) ventilation at home is shown to improve right heart dysfunction, increase patient quality of life and reduce postoperative complications.9
A dietetic, psychologist and physiotherapy review, with the dual purpose of assessment and patient education regarding longterm diet and lifestyle changes following bariatric surgery, form an essential part of multidisciplinary preparation. Patients are required to stop smoking with active support. They are offered group education sessions with specialist bariatric dietitians and physiotherapists with input from a bariatric physician and/or nutritionists. The aim is to provide holistic patient-centred care and educate patients about managing their obesity as a lifelong chronic condition with a special focus on healthy eating, portion control, reduction of alcohol and sugary drink consumption and increasing physical activity with multidisciplinary long-term follow-up care.
The Liver Shrinkage Diet
Obesity is commonly associated with an enlarged and fatty liver, restricting and complicating surgical access to the gastroesophageal junction behind the left lobe and increasing the risk for laceration of the liver. A low-calorie, low-carbohydrate diet leads to increased glycogen utilization in the liver with a dual benefit of liver size shrinkage and some overall weight loss. As part of optimisation, patients are advised to follow this diet for 2 to 6 weeks immediately prior to surgery. The liver shrinkage diet often consists of a low-fat, 1000-kcal/day diet with detailed written instructions, in consultation with our bariatric physicians and dietitians tailored to the patient’s preference.
Patients are instructed to completely avoid high-carbohydrate, high-fat food items such as sweets, potato crisps and chocolates, sugary drinks and alcohol. Water intake is encouraged with supplementation of multivitamins and fibre.
Preoperative Risk Stratification
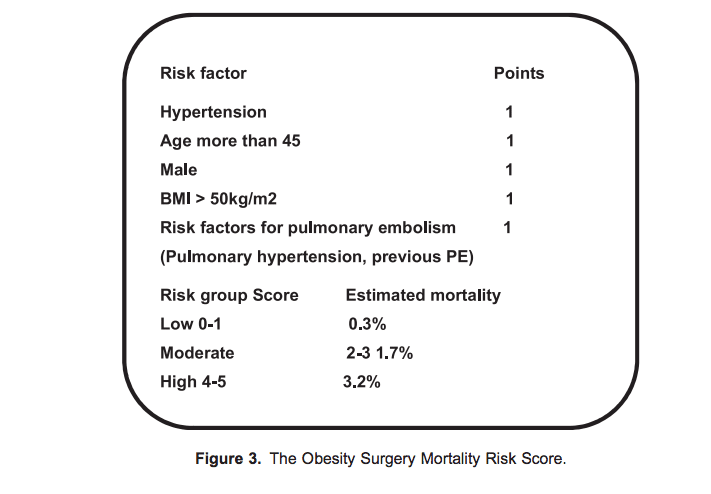
The Obesity Surgery Mortality Risk Score10 (Figure 3) is a validated tool that can be used to stratify risk and plan care for the bariatric surgical population. Class C patients are likely to require closer postoperative monitoring, and postoperative intensive care/high-dependency unit admission can be considered. The Obesity Surgery Mortality Risk Score, although validated only for bariatric surgical patients, can be applied to obese patients undergoing nonbariatric operations and guide perioperative management.
INTRAOPERATIVE CARE
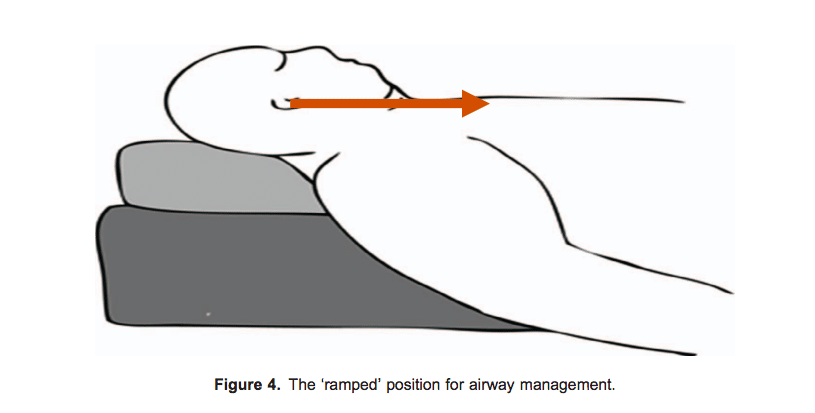
The key element of care is meticulous attention to patient positioning, incorporating ‘ramping’ for airway management, steep reverse Trendelenburg position for optimal surgical access and measures to prevent slipping, safe transfers and careful protection of pressure areas to prevent nerve and skin damage.
Airway Management
Obesity is associated with increased chance of difficult/failed intubation and complications of airway management.11,12 Routinely ‘ramping’ obese patients in the 20o to 30o head-up position (ie, elevating the head and upper body until the external auditory meatus and the sternal notch are in the same horizontal plane) facilitates optimal preoxygenation and ease of intubation (Figure 4). High-flow nasal oxygen should also be considered during intubation.11,12
The anaesthetist should have immediate access to equipment for difficult airway management available in their centre and use a laryngoscopy technique most familiar to them. Induction of general anaesthesia on the operating room table and use of an inflatable hover mattress increase ease and safety of patient transfer. A large-bore orogastric tube is inserted for some operations, this needs some intraoperative manipulation and removal prior to extubation.
Monitoring
Monitoring13 should include ECG, noninvasive blood pressure, peripheral oxygen saturations, end-tidal CO2, temperature and peripheral nerve stimulator for neuromuscular block. Some points specific to bariatric surgery include the following:
- A range of large blood pressure cuffs should be available. The blood pressure cuff may need to be placed on the forearm when the upper arms are conical in shape.
- The temperature probe should not be inserted in the oesophagus to avoid accidental stapling of the probe to the gastric sleeve. Instead, aural or pharyngeal temperature could be recorded.
- Occasionally, central venous access and invasive arterial monitoring may be needed.
- Ultrasound can be extremely helpful for challenging intravenous and intra-arterial access.
- Depth of anaesthesia monitoring is highly recommended with intravenous technique and is also useful to titrate inhalational anaesthetic agent.
- Intraoperatively, the goal is to maintain an adequate cerebral perfusion pressure, whilst hypertension may need to be treated with titrated doses of intravenous beta-blockers such as labetalol/metoprolol. Adjustments for cerebral perfusion pressure must take steep head-up positioning into account.
Intraoperative Ventilation Strategies
Laparoscopy insufflation pressures used in bariatric surgery are commonly higher (15-20 mm Hg) than usual (10-15 mm Hg). Pressure-controlled ventilation with titrated positive end-expiratory pressure to maximise tidal volumes for a given pressure and minimise intra- and postoperative atelectasis with monitored neuromuscular block is a good practical strategy. In practice, the steep reverse Trendelenburg position used for bariatric surgery mitigates the effect of pneumoperitoneum on ventilation to a certain degree.
Perioperative Drug Dosing
Obesity can affect the distribution, binding and elimination of the drugs with a tendency to accumulate lipophilic drugs, especially if given as infusions due to increased volume of distribution. However, there is limited information on the effect of obesity on the pharmacology of commonly used anaesthetic drugs. Much of the excess weight is fat, which is usually poorly perfused but can act as a reservoir for highly lipophilic drugs. Principles of perioperative anaesthesia drug use are as follows:
- Use short-acting drugs where possible;
- Use caution with long-acting opioids;
- Titrate drugs to effect;
- Base drug dosing on ideal body weight or adjusted body weight to avoid overdosing.
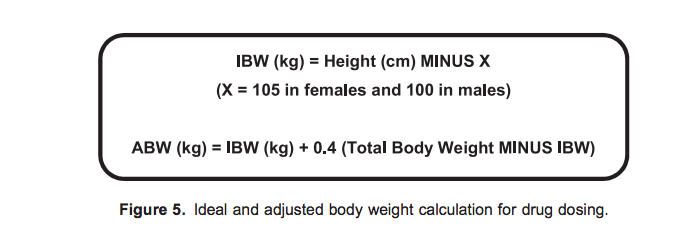
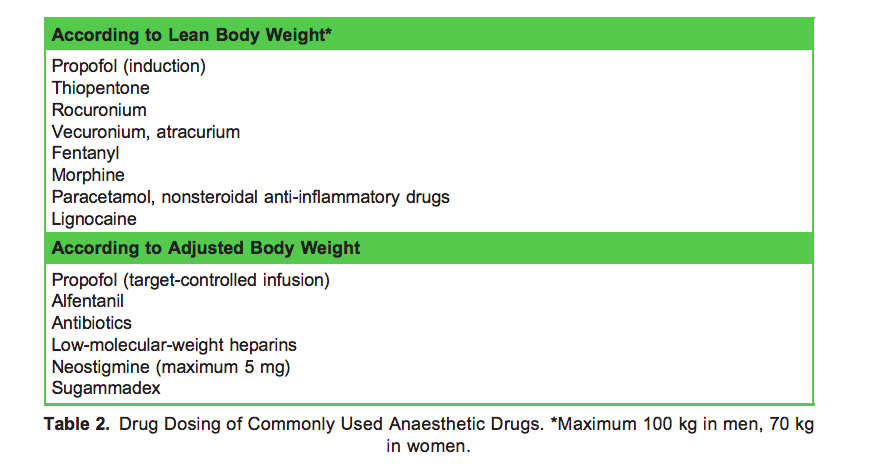
Lean body weight (LBW) is the patient’s weight excluding fat. LBW rarely exceeds 100 kg in men and 70 kg in women. Adjusted body weight (Figure 5) considers the fact that obese individuals have increased lean body mass and an increased volume of distribution for drugs. As a general rule, we recommend ideal body weight and adjusted body weight as guides to drug dosing13 (Table 2), with exception for some drugs (eg, suxamethonium).
Practical points for clinical practice are as follows:
- Induction: A more rapid redistribution of induction agents into the larger fat mass means that patients wake up more quickly than nonobese patients after a single bolus dose. A dose based on total body weight is likely to result in significant hypotension.
- Muscle relaxants: Hydrophilic drugs such as neuromuscular blockers should be administered according to ideal body weight, as their volume of distribution remains relatively consistent. Total body weight can be used for suxamethonium due to increased plasma cholinesterase activity. Doses of neostigmine and sugammadex are related to the timing and total dose of neuromuscular blocking drugs to be reversed and should be titrated to effect.
- Intraoperative opioids: These drugs should be dosed using lean body weight to begin with and titrated to effect once the patient is awake.
- Target controlled infusions: The Marsh and Schneider formulae for target-controlled infusions of propofol become unreliable for patients weighing more than 140 kg. None of the commercially available pumps allow input of weights greater than 150 kg using the Marsh model or a BMI >35 kg/m2 (female) and 42 kg/m2 (male) using the Schneider model.
- Desflurane and remifentanil: These drugs lend themselves well to the obese population because of the minimal accumulation in fatty tissues, with some evidence for use of desflurane as the agent of choice.
Postoperative Analgesia
Multimodal, opioid-sparing analgesia with titrated doses of long-acting opioids are the guiding principles. We recommend regular paracetamol supplemented by nonsteroidal analgesics if appropriate with carefully titrated opioids. Regional analgesia can be useful but challenging, and a rectus sheath block can be done by the surgeon under direct vision at the end of the operation. Local anaesthetic infiltration of surgical incisions should be routine, with ideal body weight used as a guide for dosing.
Prevention of Nausea and Vomiting
Prevention of postoperative nausea and vomiting (PONV) is an important component of care not only to avoid distress to the patients but also from a surgical point of view to allow the anastomosis to heal. This cohort of patients are at high risk of PONV.14 We recommend prophylaxis with 2 antiemetics such as ondansetron and dexamethasone if possible, with continuation of ondansetron, prochlorperazine and/or cyclizine postoperatively.
Extubation and Transfer to the Postanaesthesia Care Unit
Patients should be extubated awake in the sitting position following complete reversal of neuromuscular blockade and return of airway reflexes. An inflatable hover mattress is a very useful for transfers. Monitoring should be continued in the recovery area and opioid analgesics carefully titrated. All obese patients and particularly those with OSA should be monitored for a period whilst unstimulated to rule out airway obstruction and respiratory depression.
Opioid-Free Anaesthesia
The opioid-free anaesthesia (OFA) technique has been recently reported in the literature15 for the bariatric surgery population and is popular in certain parts of Europe, demonstrating good outcomes. OFA involves avoidance of opioids by all routes, including by intravenous and neuraxial routes, in the intraoperative period and has the benefits of reduced PONV and reduction of postoperative respiratory depression, particularly in patients with obstructive sleep apnoea. This typically involves sympatholysis and amnesia with dexmedetomidine and anaesthesia maintenance with desflurane monitored and titrated with bispectral index monitoring; co-analgesia with ketamine, magnesium and intravenous lignocaine infusion; and deep neuromuscular blockade maintained until the end of the operation. Intravenous nonsteroidal anti-inflammatory drugs, highdose paracetamol, dexamethasone and gabapentin may be added with routine use of local anaesthetic infiltration. The OFA technique has not been adopted widely because of the lack of robust evidence.
POSTOPERATIVE CARE
Most patients can be safely managed on bariatric surgical wards. The Obesity Surgery-Mortality Risk Score can also be used to plan postoperative care, with high-risk patients admitted to high-dependency unit/intensive/critical care for monitoring. As a high-volume centre with an experienced perioperative team, we admit very few of our patients to critical care.
The important components of postoperative care include the following:
- Avoidance of intravenous infusions, intravenous patient-controlled analgesia or urinary catheters to encourage early mobilisation;
- Routine administration of prophylactic low-molecular-weight heparin, with mechanical devices to prevent thromboembolism;
- Early resumption of deep-breathing exercises with physiotherapy input and CPAP if already in place;
- Careful review of blood glucose levels, as requirement for diabetes medications may decrease significantly in the first 48 hours;
- Multimodal, opioid-sparing analgesia and routine plus as-required antiemetics with avoidance of intramuscular medication; all oral medicines need to be prescribed in a crushed/liquid form or sublingually for a few days to weeks after bariatric surgery, until patients can resume taking tablets;
- Use of proton-pump inhibitors routinely considered for the first few weeks;
- Wound care and avoidance of infection;
- Early discharge with written instructions arrangements for long-term follow-up care.
FUTURE DIRECTION
Currently, 2 clinical trials are under way related specifically to perioperative anaesthetic practices in bariatric surgery:
- The Prospective Opioid-Free Anaesthesia (POFA) trial is a prospective, randomised, parallel, single-blind, multicentre study16 of 400 obese patients undergoing elective intermediate or major noncardiac surgery, comparing a standard anaesthesia protocol or an OFA. The primary outcome measure is the occurrence of a severe postoperative opioid-related adverse event within the first 48 hours after extubation, defined as postoperative hypoxaemia or postoperative ileus or postoperative cognitive dysfunction.
- The High Flow Nasal Oxygen After Bariatric Surgery (OXYBAR) study is a prospective, unblinded, single-centre, randomised, controlled pilot study17 comparing the use of high-flow nasal oxygen versus standard oxygen therapy for patients undergoing laparoscopic bariatric surgery. The primary outcome measure is the change in end-expiratory lung impedance, and secondary outcome measures include change in tidal volume, partial arterial pressure of oxygen/fraction of inspired oxygen (PaO2/FiO2) ratio, incidence of postoperative pulmonary complications, hospital length of stay and measures of patient comfort.
SUMMARY
Obesity is a complex, chronic condition that is now common across the world and is difficult to manage. As bariatric surgery becomes more common, anaesthetists should be familiar with the perioperative care for bariatric surgery. As the march of the obesity pandemic continues, many of the skills as a ‘bariatric’ anaesthetist are transferable and are likely to become an essential component of the skillset belonging to a ‘generalist’ anaesthetist.
REFERENCES
1. World Health Organisation. Health Topics: Obesity. https://www.who.int/topics/obesity/en/. Accessed September 25, 2019.
2. Rubino F, Nathan D, Eckel R, et al. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by International Diabetes Organizations. Diabetes Care 2016;39(6):861-877.
3. Sjo¨ stro¨ m L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683-2693.
4. Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724-1737.
5. Schiavon CA, Bersch-Ferreira AC, Santucci EV, et al. Effects of bariatric surgery in obese patients with hypertension: the GATEWAY randomized trial (gastric bypass to treat obese patients with steady hypertension) Circulation. 2018;137(11):1132-1142. doi:10.1161/CIRCULATIONAHA.117.032130
6. International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO). 5th annual report. https://www.ifso.com/ifso-registry/. Accessed September 20, 2019.
7. UK National Health Service. Weight loss surgery. https://www.nhs.uk/conditions/weight-loss-surgery/types/. Accessed October 2, 2019.
8. Rogers CA, et al. Adaptation of the By-Band randomized clinical trial to By-Band-Sleeve to include a new intervention and maintain relevance of the study to practice. Br J Surg. 2017;104(9):1207-1214. doi:10.1002/bjs.10562
9. Recommendations for screening and management of sleep disordered breathing (SDB) in patients undergoing bariatric surgery. Society of Obesity and Bariatric Anaesthesia, UK. 2016. https://www.dropbox.com/s/7njcdrrjfqgcyp1/SOBA%
20OSA%20Guideline%202016.pdf?dl=0 Accessed November 13, 2019.
10. Efthimiou E, Court O, Sampalis J, et al. Validation of Obesity Surgery Mortality Risk Score in patients undergoing gastric bypass in a Canadian center. Surg Obes Relat Dis. 2009;5:643-647.
11. Collins JS, Lemmens HJM, Brodsky JB, Brock-Utne JG, Levitan RM. Laryngoscopy and morbid obesity: a comparison of the ‘‘sniff’’ and ‘‘ramped’’ positions. Obes Surg. 2004;14:1171-1175.
12. Cook TM, Woodall N, Frerk C; on behalf of the Fourth National Audit Project. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Br J Anaesth. 2011;106(5):617-631.
13. Association of Anaesthetists of Great Britain and Ireland Society for Obesity and Bariatric Anaesthesia. Peri-operative management of the obese surgical patient 2015. Anaesthesia. 2015;70(7):859-876.
14. Apfel CC, Korttila K, Abdalla M et al. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. N Engl J Med. 2004;350(24):2441-2451.



