General Topics
KEY POINTS
- Perioperative myocardial ischaemia may increase 30-day mortality when it results in myocardial infarction.
- Optimise at-risk patients preoperatively where time allows.
- Aim to match myocardial supply and demand intraoperatively and monitor for evidence of ischaemia during the perioperative period.
INTRODUCTION
Myocardial ischaemia can proceed to myocardial infarction (MI), this is important as perioperative MI is associated with a significant increase in 30-day mortality.1 This article will discuss preoperative, intraoperative, and postoperative strategies for prevention and management of perioperative myocardial ischaemia.
PREOPERATIVE CONSIDERATIONS
Risk-Evaluation Scoring Systems
Multiple scoring systems are available that predict the risk of major adverse cardiac events.2 They tend to focus on a patient’s past medical history and surgical risk factors. Lee’s Revised Cardiac Risk Index is a simple, validated, and widely used scoring system that predicts major cardiac complications in major elective non-cardiac surgery2. The 6 independent factors are listed in Table 1.
Predicted cardiac event rate increases with increasing number of risk factors present, ranging from 0.4%-11%: 0 points- 0.4%; 1 point- 0.9%; 2 points- 6.6%; ≥ 3 points – 11%.2
Lee’s cardiac risk index is only validated for elective surgery and does not encompass all risk factors for major adverse cardiac events. Of note, the outcome is a composite endpoint, not specific to myocardial ischaemia or infarction. Other important risk factors include recent MI, recent insertion of coronary stents, elevated preoperative high-sensitivity troponin-I, valvular heart disease, decompensated heart failure, and arrhythmias. This article will discuss some of these risk factors in greater detail.
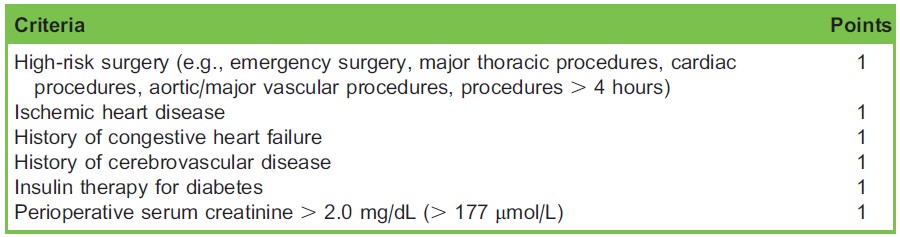
Table 1. The Lee Revised Cardiac Risk Index
Recent Percutaneous Coronary Intervention (PCI)
Subsequent to PCI, there is a known risk of in-stent thrombosis, which decreases with time after the procedure. In-stent thrombosis may result in myocardial ischaemia and is associated with a high mortality. In order to reduce this risk, patients are commenced on dual antiplatelet agents for the highest-risk period; the duration of therapy is specific to the type of stent placed.
Dual antiplatelet therapy increases the susceptibility to bleeding perioperatively. The risk of bleeding must be balanced against the risk of in-stent thrombosis relative to early cessation of antiplatelet agents. Because of these factors the 2014 American Heart Association/American College of Cardiology (AHA/ACC) guideline recommends that elective surgery be delayed (Table 2) and that urgent or emergency surgery have a multidisciplinary discussion regarding the risk and benefit of continuing or ceasing antiplatelet agents perioperatively.3 Aspirin should be continued where possible.
Recent MI
A recent MI increases the risk of perioperative MI and mortality.4 As time since the MI occurred increases, the risk of reinfarction decreases. A retrospective study showed that the risk of reinfarction decreased from 32.8% when surgery occurred within 0-30 days of MI compared with 5.9% when surgery occurred 91-180 days post-MI.4 The likelihood of reinfarction and mortality clearly fall with increasing time from MI, but it is not currently possible to give an accurate estimate of risk at a given time point following infarction. American guidelines recommend delaying elective surgery for at least 60 days post-MI where possible to mitigate this risk.3
Optimisation
Non-invasive Cardiac Stress Testing
The 2014 European Society of Cardiology/European Society of Anaesthesia (ESC/ESA) and the AHA/ACC guidelines propose preoperative stress testing if all the following criteria are met:
- Surgery is elective.
- Patient has poor functional capacity limited by angina or shortness of breath (< 4 Metabolic equivalents (METs), or with unknown functional capacity).
- Patient has an elevated perioperative risk of major adverse coronary events.
- Testing will impact decision making for perioperative care.3,5
Patients with excellent functional capacity (> 10 METs) need not have exercise stress testing. Guidance is less clear regarding those patients with elevated cardiac risk and moderate to good functional capacity (4-10 METs), for whom ‘‘. . .it may be reasonable to forgo further exercise testing. . .and proceed to surgery.’’3
Coronary Revascularisation
Indications for preoperative coronary artery revascularisation in patients at risk of myocardial ischaemia are similar to the indications outside of the perioperative setting.3,5 In particular, no benefit has been shown for preoperative prophylactic revascularisation in patients with stable or asymptomatic coronary artery disease.6 Revascularisation with either PCI or surgery has not been shown to improve outcomes with the caveat that studies invariably excluded patients with a strong indication for cardiac surgery, such as left main stem disease or its equivalent.
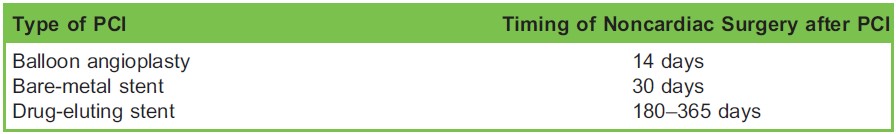
Table 2. Recommended Timing of Elective Noncardiac Surgery Following Percutaneous Coronary Intervention (PCI)3
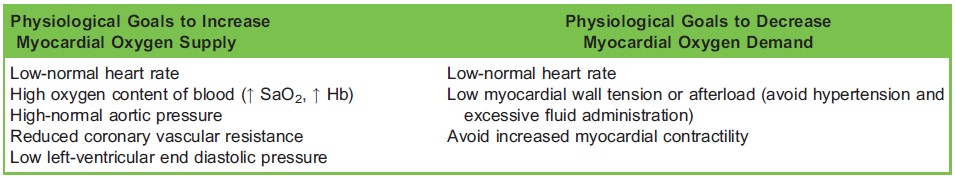
Table 3. Determinants of Myocardial Oxygen Demand and Supply
Medication Considerations
Beta-Blockers
Existing literature on perioperative use of beta-blockers has been muddied by fraudulent research. Guidelines suggest continuing beta-blockers for those already taking them, and uncertainty exists about starting patients who are at risk of perioperative myocardial ischaemia on beta-blockers de novo.3,5 Careful titration to heart rate in high-risk patients may be beneficial and physiologically attractive. However, in adopting a one size fits all approach, whilst reducing MI, starting patients on beta-blocker could lead to increased mortality and stroke risk, likely due to drug-induced hypotension.
Aspirin
Continuing aspirin perioperatively is contentious subsequent to a recent large randomised controlled trial (RCT) that showed an increased rate of significant bleeding without improved mortality or reduced nonfatal MI.7 Current consensus guidelines recommend that for patients that are on aspirin the decision to continue aspirin should be based on individual risk of perioperative bleeding relative to risk of thrombotic complications.3,5 Separate guidelines exist for those who have had recent acute coronary syndrome (ACS) or PCI.
Angiotensin-converting enzyme inhibitors (ACEis) and angiotensin-receptor blockers (ARBs)
Controversy exists regarding use of ARBs and ACEis perioperatively. American guidelines suggest it is reasonable to continue their use,3 whereas European guidelines suggest discontinuing therapy if the indication is for hypertension.5
Statins
Statins may reduce the incidence of perioperative MI. Statins should be continued if patients are already on them and could be initiated in patients undergoing vascular surgery at least 2 weeks preoperatively,5 although there are no large-scale prospective trials to confirm this approach.
Clonidine
There is no evidence of benefit from prophylactic use of preoperative clonidine.
Emergency Surgery
Elective surgery allows time for a thorough workup and optimisation of high-risk patients. This benefit is sometimes outweighed by the consequences of delaying emergency surgery. In these circumstances, the AHA/ACC guidelines recommend proceeding using ‘‘appropriate monitoring and management strategies based on the clinical assessment.’’3
INTRAOPERATIVE CONSIDERATIONS
Physiological Goals
Two main mechanisms are postulated to cause perioperative myocardial ischaemia—acute coronary artery plaque rupture or instability and myocardial oxygen supply-demand imbalances (often in the presence of stable coronary artery disease). The proportional contribution of each mechanism is contentious. Contributing factors include increasing myocardial oxygen demand from sympathetic response to pain, trauma, and inflammation, and reduction in myocardial oxygen supply from anaemia, hypoxia, hypotension, and arterial thrombosis from perioperative hypercoagulability.
It is the myocardial supply-demand imbalance that can be modified intraoperatively to prevent myocardial ischaemia. Myocardial oxygen supply is governed by the oxygen content of blood and coronary blood flow. Blood oxygen content is mainly determined by haemoglobin concentration and SaO2 and coronary blood flow is increased by increasing diastolic time (inversely proportional to heart rate), mean arterial blood pressure and calibre of coronary arteries. The calibre of the coronary arteries is largely controlled by metabolic autoregulation to meet the demands of the myocardium and by the myocardial wall tension. In pathological states, the calibre can be decreased by atherosclerosis.
Myocardial oxygen demand is increased with increasing heart rate, afterload, myocardial wall tension, and myocardial contractility.
Although techniques to match myocardial oxygen supply and demand would seem prudent in the patient with ischaemic heart disease, not all have supporting evidence for improved outcomes.
Oxygen
Emerging evidence from the non-perioperative setting suggests that hyperoxia can increase infarct size in acute ST-elevation MI.8 In the perioperative setting, a non–statistically significant association between high FiO2 and acute coronary syndrome has been demonstrated.9 Although further evidence is required, a pragmatic approach would be to maintain normal oxygen saturations, using the lowest possible FiO2.
Heart Rate
Large doses of prophylactic heart rate–reducing agents given preoperatively have not proved to be beneficial.10 However, avoiding tachycardia with careful titration of analgesia and beta-blockers makes theoretical sense and has not been sufficiently studied to discredit.
Transfusion Thresholds
Weak evidence suggests a higher transfusion threshold (such as Hb > 100 g/dL) might result in better outcome for patients with acute coronary syndrome11; however, no survival benefit has been demonstrated in higher transfusion thresholds for those at risk of cardiovascular disease perioperatively.12 The National Institute for Health and Care Excellence (NICE) guidelines recommend a restrictive transfusion threshold of 70 g/L unless the patient has acute coronary syndrome, in which case the more liberal threshold of 80 g/L is recommended. Further research is needed to clarify the appropriate transfusion threshold for patients with stable coronary artery disease; however, patients with signs of ischaemia or who are particularly high risk may theoretically warrant a transfusion threshold of 90 or 100 g/L.
Temperature Control
Some studies suggest mild hypothermia is associated with increased perioperative myocardial ischaemia and cardiac events when compared with normothermia. The mechanism for this is not clearly understood.
Anaesthetic Technique
There is no strong evidence to support a specific anaesthetic technique in preventing myocardial ischaemia.
General Anaesthesia vs Regional/Neuraxial
Although some controversy exists, the majority of the evidence would suggest there is no statistically significant difference between general, neuraxial, or regional anaesthetic technique.13–15 Whether this is because the studies are underpowered or represent a true finding is unclear. A confounding issue is that high-risk patients, such as those who have had a recent MI or PCI, are more likely to be on antiplatelet therapy, which may preclude neuraxial and regional techniques, thus resulting in overrepresentation of high-risk patients in the general anaesthesia groups.
Nitrous Oxide
The addition of nitrous oxide to a general anaesthetic does not appear to increase mortality at 1 year or cardiovascular complications at 30 days in patients at risk of cardiovascular complications.16
Volatile compared with Total Intravenous Anaesthesia (TIVA)
There is insufficient evidence to recommend TIVA or volatile as a preferred option in the prevention of myocardial ischaemia in noncardiac surgery.
Cyclooxygenase-2 (COX-2) Inhibitors
There is a view that selective COX-2 enzyme inhibitors result in a prothrombotic state which increases the risk of MI. Two large meta-analyses17 have supported this view with increased risk of MI for those taking COX-2 inhibitors compared with a placebo.
Intraoperative Monitoring
Each patient will have a given baseline risk of perioperative myocardial ischaemia (as discussed earlier) and monitoring should initially be dictated by this. Specific monitoring options include the following:
Electrocardiogram (ECG)
ECG monitoring is a standard of care according to the Association of Anaesthetists of Great Britain and Ireland (AAGBI) Recommendations for Standards of Monitoring During Anaesthesia and Recovery. ECG is a cheap, easy, and noninvasive means of monitoring for myocardial ischaemia. The addition of precordial leads to the standard 3-lead ECG for patients at risk of myocardial ischaemia increases its sensitivity. A small intraoperative study indicated that in isolation, leads V5 and V4 were most sensitive (75% and 61+% respectively). Combining leads increases sensitivity, with V4 and V5 having a 90% sensitivity, leads II and V5 having 80% sensitivity, and leads II, V4, and V5 having a sensitivity of 96%.18 A more recent study showed that 2 or more precordial leads are required to achieve a sensitivity for MI or ischaemia of 95% or more.19 Automated ST-segment analysis, while not as good at detecting ischaemia, can alert the anaesthetist to ECG changes.
Blood Pressure Measurement
Intraoperative hypotension has an association with adverse cardiac events.20 Mean arterial blood pressure is also one of the determinants of myocardial oxygen supply. It would follow that accurate measurement and timely treatment of hypotension (and hypertension) is important in those at risk of myocardial ischaemia. Arterial line placement gives accurate real-time blood pressure measurement to aid these objectives. The potential for adverse consequences of hypotension means that invasive blood pressure monitoring should be considered in high-risk patients.
Transoesophageal Echocardiography (TOE)
TOE detects myocardial ischaemia by identifying regional wall motion abnormalities. TOE has associated risks and costs, and it requires an experienced operator. For these reasons routine TOE monitoring for those at risk of myocardial ischaemia is not recommended except for in response to persistent intraoperative haemodynamic instability.3
Pulmonary Artery Catheter
Routine use of pulmonary artery catheters in high-risk patients is not recommended.3,5
Diagnosis of Ischaemia and Infarction
Acute Myocardial Ischaemia (or Acute Coronary Syndrome)
Myocardial ischaemia is identified by a patient’s symptoms and signs or from ECG abnormalities. Symptoms of ischaemia (such as pain in the chest, mandible, or upper extremity) may be absent in the perioperative setting where anaesthesia or strong analgesia has been administered.21 Other signs of ischaemia include tachycardia, haemodynamic instability, and evidence of pulmonary congestion (such as reduced oxygen saturations, lung compliance, or wheeze).
ECG criteria to diagnose acute myocardial ischaemia require at least 2 anatomically contiguous lead with the following22:
- ST elevation at the J point of at least 1mm (depending on location) or
- ST depression of at least 0.5 mm, and/or T wave inversion of at least 1 mm.
Acute MI
MI is defined as myocardial cell death due to prolonged myocardial ischaemia. It is diagnosed by22 a rise of cardiac biomarker value above the 99th percentile limit with at least 1 of the following:
- Symptoms of ischaemia,
- New ST-segment T wave changes or new left bundle branch block,
- New pathological Q waves,
- Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality
- Identification of an intracoronary thrombus by angiography or autopsy OR: Cardiac death with symptoms suggestive of myocardial ischaemia.
It is important to note that the above diagnostic criteria have not been created for the perioperative setting. An elevated troponin after noncardiac surgery, even without other features of ischaemia independently increases the risk of 30-day mortality.21 With this in mind, a new perioperative diagnosis has been created—myocardial injury after noncardiac surgery (MINS). MINS is diagnosed by a postoperative peak troponin T of 0.03 ng/mL or greater due to myocardial ischaemia.21 Although a diagnosis of MINS has prognostic significance, the clinical utility remains uncertain.
Management of Myocardial Ischaemia
Once myocardial ischaemia is suspected, management strategies are as follows:
Confirm Diagnosis
- Obtain 12-lead ECG.
- Consider transoesophageal or transthoracic echocardiogram if haemodynamic instability is detected.
- Obtain baseline and 4-hour troponin levels.
Optimise Myocardial Oxygen Supply-and-Demand Balance
- Pause surgery if appropriate while the situation is stabilized
- Achieve physiologic goals as mentioned earlier: low/normal heart rate, normal blood pressure, normal oxygen saturations with the least FiO2 possible, avoid hypothermia, avoid excessive fluid.
- Administer medications: beta-blockers to achieve low or normal heart rate provided no hypotension, consider giving aspirin (via nasogastric tube if under general anaesthesia), and a glyceryl trinitrate (GTN) infusion.
- Consider use of intra-aortic balloon pump, as guided by cardiologists.
Consider Abandoning Surgery
This will be situation-specific and involve a multidisciplinary discussion. Considerations include the following:
- How unstable is the patient?
- How urgent is the surgery?
- Can the surgery stop rapidly if the patient deteriorates?
If the surgery is continued, having an experienced surgeon to ensure shortest surgical time might be of benefit to the patient.
Consult Cardiologist
If evidence of ST-elevation MI is present on ECG, or there is haemodynamic instability, emergent cardiology opinion is recommended to consider need for PCI. Thrombolysis is usually contraindicated if surgical incision has been made.
POSTOPERATIVE CONSIDERATIONS
Postoperative management will be patient-specific but considerations include the following:
- Postoperative placement: consider more intensive monitoring as appropriate, including need for telemetry.
- Consider need for serial ECGs or troponins depending on index of suspicion of MI.
- Ensure cardiology follow-up or in-patient review if infarct is suspected.
- Ensure good analgesia, euvolaemia, and the addition of beta-blockers (blood pressure allowing) to minimise tachycardia.
- Maintain normal oxygen saturations with judicious oxygen therapy.
- Commence aspirin and consider PGY12 inhibitor as guided by cardiology opinion.
SUMMARY
- Perioperative myocardial ischaemia is an important entity with prognostic implications.
- Preoperatively, patients should have their perioperative risk clarified, and be optimised where time permits.
- Intraoperative management consists of appropriate monitoring and anaesthetic technique, preventing myocardial oxygen supply-demand imbalances and identifying and treating intraoperative myocardial ischaemia.
- Postoperative considerations will depend on intraoperative events and the risk category of the patient, but may involve intensive monitoring and cardiology review.
REFERENCES AND FURTHER READING
- Devereaux P, Xavier D, Pogue J, et al. Characteristics and short-term prognosis of perioperative myocardial infarction in patients undergoing noncardiac surgery: a cohort study. Ann Intern Med. 2011;154(8):523-528.
- Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100(10):1043-1049.
- Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(22):e77-e137.
- Livhits M, Ko CY, Leonardi MJ, Zingmond DS, Gibbons MM, de Virgilio C. Risk of surgery following recent myocardial infarction. Ann Surg. 2011;253(5):857-864.
- Kristensen SD, Knuuti J, Saraste A, et al. 2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assessment and management. Eur Heart J. 2014:ehu282.
- McFalls EO, Ward HB, Moritz TE, et al. Coronary-artery revascularization before elective major vascular surgery. N Engl J Med. 2004;351(27):2795-2804.
- Devereaux P, Mrkobrada M, Sessler DI, et al. Aspirin in patients undergoing noncardiac surgery. N Engl J Med. 2014;370(16):1494-1503.
- Stub D, Smith K, Bernard S, et al. Air versus oxygen in ST-segment elevation myocardial infarction. Circulation. 2015;131(24):2143-2150.
- Fonnes S, Go¨ genur I, Søndergaard ES, et al. Perioperative hyperoxia—long-term impact on cardiovascular complications after abdominal surgery, a post hoc analysis of the PROXI trial. Int J Cardiol. 2016;215:238-243.
- Group PS. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008;371(9627):1839-1847.
- Carson JL, Brooks MM, Abbott JD, et al. Liberal versus restrictive transfusion thresholds for patients with symptomatic coronary artery disease. Am Heart J. 2013;165(6):964-971. e961.
- Carson JL, Sieber F, Cook DR, et al. Liberal versus restrictive blood transfusion strategy: 3-year survival and cause of death results from the FOCUS randomised controlled trial. Lancet. 2015;385(9974):1183-1189.
- Guay J, Parker MJ, Gajendragadkar PR, Kopp S. Anaesthesia for hip fracture surgery in adults. Cochrane Library. 2016. Feb 22;2:CD000521.
- Group GTC. General anaesthesia versus local anaesthesia for carotid surgery (GALA): a multicentre, randomised controlled trial. Lancet. 2009;372(9656):2132-2142.
- Chu C-C, Weng S-F, Chen K-T, et al. Propensity score–matched comparison of postoperative adverse outcomes between geriatric patients given a general or a neuraxial anesthetic for hip surgery: a population-based study. Anesthesiology. 2015;123(1):136-147.
- Myles PS, Leslie K, Chan MT, et al. The safety of addition of nitrous oxide to general anaesthesia in at-risk patients having major non-cardiac surgery (ENIGMA-II): a randomised, single-blind trial. Lancet. 2014;384(9952):1446-1454.
- Chen LC, Ashcroft DM. Risk of myocardial infarction associated with selective COX-2 inhibitors: meta-analysis of randomised controlled trials. Pharmacoepidemiol Drug Saf. 2007;16(7):762-772.
- London MJ, Hollenberg M, Wong MG, et al. Intraoperative myocardial ischemia: localization by continuous 12-lead electrocardiography. Anesthesiology. 1988;69(2):232-241.
- Landesberg G, Mosseri M, Wolf Y, Vesselov Y, Weissman C. Perioperative myocardial ischemia and infarction identification by continuous 12-lead electrocardiogram with online ST-segment monitoring. Anesthesiology. 2002;96(2):264-270.
- Walsh M, Devereaux PJ, Garg AX, et al. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery toward an empirical definition of hypotension. Anesthesiology. 2013;119(3):507-515.
- Botto F, Alonso-Coello P, Chan M, et al. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology. 2014; 120(3):564-578.
- Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD. Third universal definition of myocardial infarction. Circulation. 2012;126(16):2020-2035.



