Basic Sciences
Part 1: Basic pharmacology of inhalational anaesthetic drugs
Before reading this tutorial think about the following questions;
- What are the ideal properties of an inhalational drug?
- What are the benefits and disadvantages of the currently available inhalational anaesthetics.
- Why does sevoflurane act faster than halothane and also wear off quicker?
The Ideal Inhalational Anaesthetic Drug
Sadly the perfect inhalational drug has not yet been produced and as a result of the quest to develop one, several different inhalational compounds have become available. Some are no longer used while others are in regular use. Of the latter, each one has advantages and disadvantages. Probably the easiest way to remember about the different inhalational drugs is to compare each to the properties of the ideal anaesthetic. These properties can be divided into :
- physical,
- pharmacodynamic (what the drug does to the patient)
- pharmacokinetic (what the patient does to the drug).
Physical properties
- Stable over a range of temperatures
- Not be degraded by light
- Does not require the presence of a preservative
- Non-explosive and does not support combustion
- Odourless or has a pleasant smell
- Environmentally safe
- Does not react with other compounds (e.g. Soda lime)
- Has a boiling point well above room temperature
Pharmacodynamic properties
- Predictable dose-related CNS depression
- Analgesic, anti-emetic and muscle relaxation properties
- Minimal respiratory depression, does not cause coughing or bronchospasm
- Minimal cardiovascular effects.
- No increase in cerebral blood flow (and therefore intracranial pressure).
- Not epileptogenic
- Does not impair renal or hepatic function
- No effect on uterine smooth muscle
- Does not trigger of malignant hyperpyrexia
Pharmacokinetic properties
- (a) Low blood: gas solubility co-efficient
- (b) Low oil: gas solubility co-efficient
- (c) Not metabolised or no active metabolites
- (d) Is excreted completely by the respiratory system
Physical properties
Because anaesthetics are given in a wide range of environments, the compound should be stable particularly when used in a warm environment and to allow storage over prolonged periods, it must not degrade on exposure to light. Even if these can be achieved by the addition of some form of preservative, this is less than ideal as its presence may impair the function of a vaporiser (for example the presence of thymol in halothane). Compounds that are explosive could be ignited either by the surgical diathermy of sparks from static electricity. Despite this a compound called cyclopropane was used until the early 1980s! It is important to remember that although not widely used, ethyl ether still falls into this category.
To allow the inhalational drug to be used during a gaseous induction its odour should not be unpleasant. As the majority of the drug will be excreted unchanged in exhaled air and will contribute to atmospheric gases, it should be environmentally safe. Some inhalational drugs can undergo chemical reactions within the circuit and produce compounds that are potentially toxic to the human body, or cause the circuit itself to perish and are best avoided. The compounds that are produced by chemical reactions can be potentially toxic to the human body, or cause the circuit itself to perish. An example would be carbon monoxide being produced when isoflurane is passed over a dry warm absorber.
Why should the boiling point of an inhalational drug be well above room temperature?
If you look at a graph of the saturated vapour pressure (SVP) of water against temperature, you can see that it is an exponential curve (Fig 1). As the boiling point is approached, there is a greater change in SVP per degree change in temperature. At the boiling point the SVP equals atmospheric pressure (this is true for any liquid). If you were to plot a graph of SVP against temperature for an inhalational drug, it would have a similar shape, although the vapour pressure for a given temperature and boiling point would be different. For example halothane boils at 50.2°C at which its SVP would be 760mmHg.
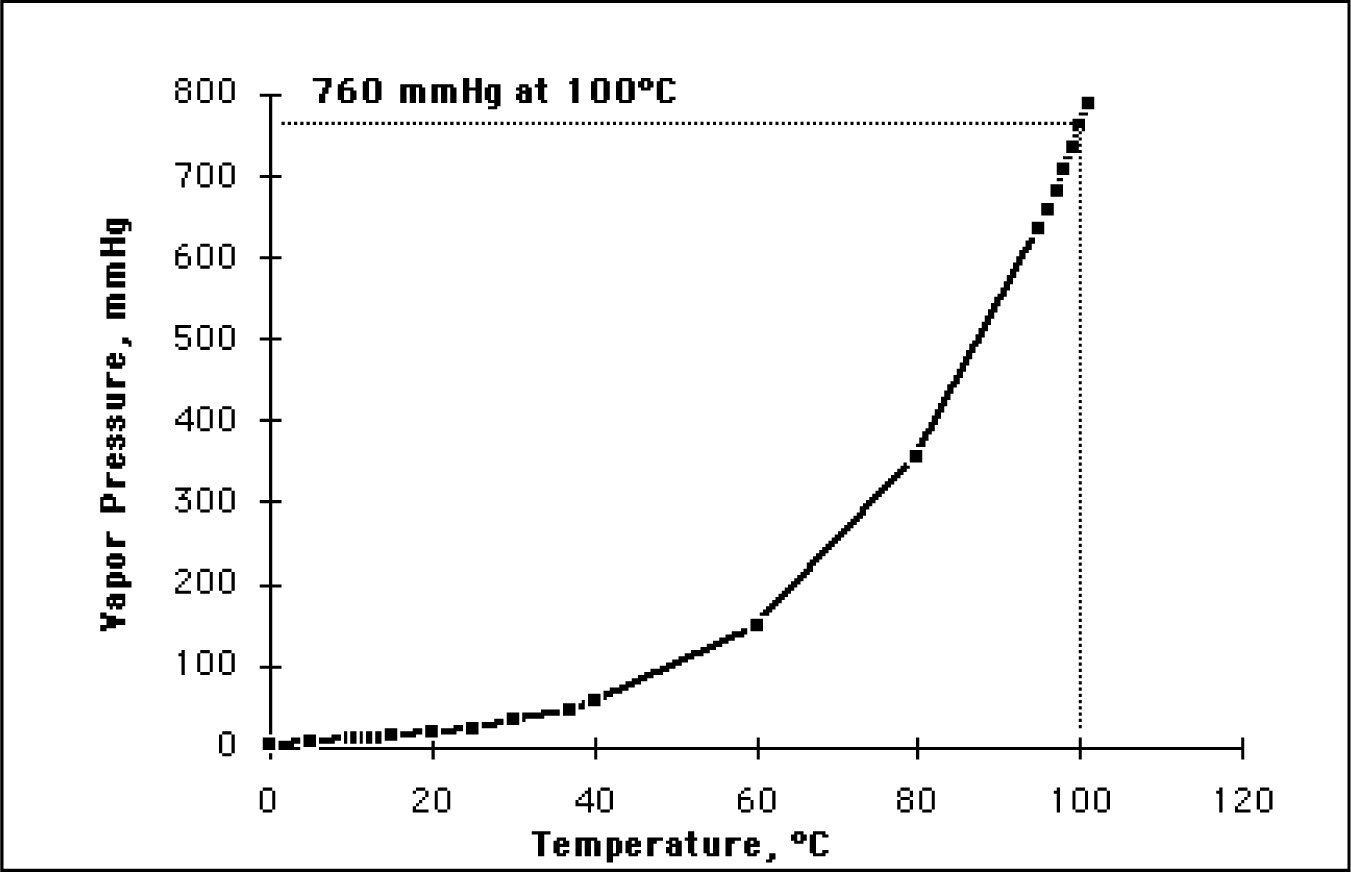
Figure 1. Relationship between temperature and saturated vapour pressure
Vaporiser accuracy depends on the temperature within the vaporiser remaining stable. This stable temperature produces a fixed vapour pressure and therefore a predictable dose of drug. Despite all the temperature compensation measures within a vaporiser, there are still small fluctuations in temperature. Therefore if the compound is close to its boiling point at room temperature, its vapour pressure curve will be at the steepest point. A small fluctuation in temperature may produce a change in the concentration of drug produced by the vaporiser, rendering it inaccurate with the potential for both over and under dosing of the patient.
Pharmacodynamic properties
The ideal drug should be able to produce a smooth induction. For this to be possible it would have to be pleasant to breathe, cause no coughing, airway irritation, or secretions. In addition, inhalation should not cause laryngospasm, bronchoconstriction or respiratory depression. As well as a hypnotic effect, the ideal drug would also have analgesic, anti-emetic, and some muscle relaxation properties, which would prevent the need for further drugs. Currently, of all the inhalational drugs, only ether has any analgesic properties, and none have any anti-emetic properties. The degree of muscle relaxation is generally dose dependant.
In addition our ideal drug would be safe to give to all patients, despite any illnesses that the patient had. This would require no adverse effects on coronary, renal or hepatic blood flow. Furthermore it would not cause cardiovascular depression or arrhythmias, or post operative seizures.
No increase in cerebral blood flow or intracranial pressure would be desirable when anaesthetising patients for intracranial neurosurgical procedures. Many neurosurgical patients already have raised intracranial pressure and an increase in cerebral blood flow will cause this to rise still further. This increase in pressure could make it difficult to operate on the brain and could lead to brain cell death.
No effect on uterine smooth muscle would be of benefit when providing a general anaesthetic for caesarean section. A relaxed uterus, post delivery will increase blood loss and will increase the chance of a blood transfusion along with its associated risks.
A small percentage of the population, when exposed to any of the currently available inhalational drugs will develop a condition called malignant hyperthermia (MH). This is a rare genetic condition which following exposure to a triggering inhalational drug will result in prolonged muscle contraction, the breakdown of muscle cells and a hyper metabolic state. If this condition is not recognised and treated it can be fatal.
Pharmacokinetic properties
The ideal inhalational drug would undergo no metabolism and be completely excreted via the respiratory system. This is because other forms of metabolism involve the renal and hepatic system and consequently are affected by their function. If a patient’s kidney or liver function were abnormal, the drug would take longer to be removed from the body and have a prolonged effect. Metabolism can also produce compounds which are toxic to the human body or have active metabolites, which again could have a prolonged effect on the patient.
The most desirable anaesthetic property is that the drug has a rapid onset and offset of action. This is primarily determined by the drug’s relative solubility in blood and fat. Metabolism plays only a very minor role.
Blood:Gas Solubility Co-efficient
This term refers to how soluble an inhalational drug is in blood compared to its vapour state. Fig 2 shows a diagrammatic representation of the situation in an alveolus when a patient breathes a mixture of inhalational drug and oxygen to induce anaesthesia.
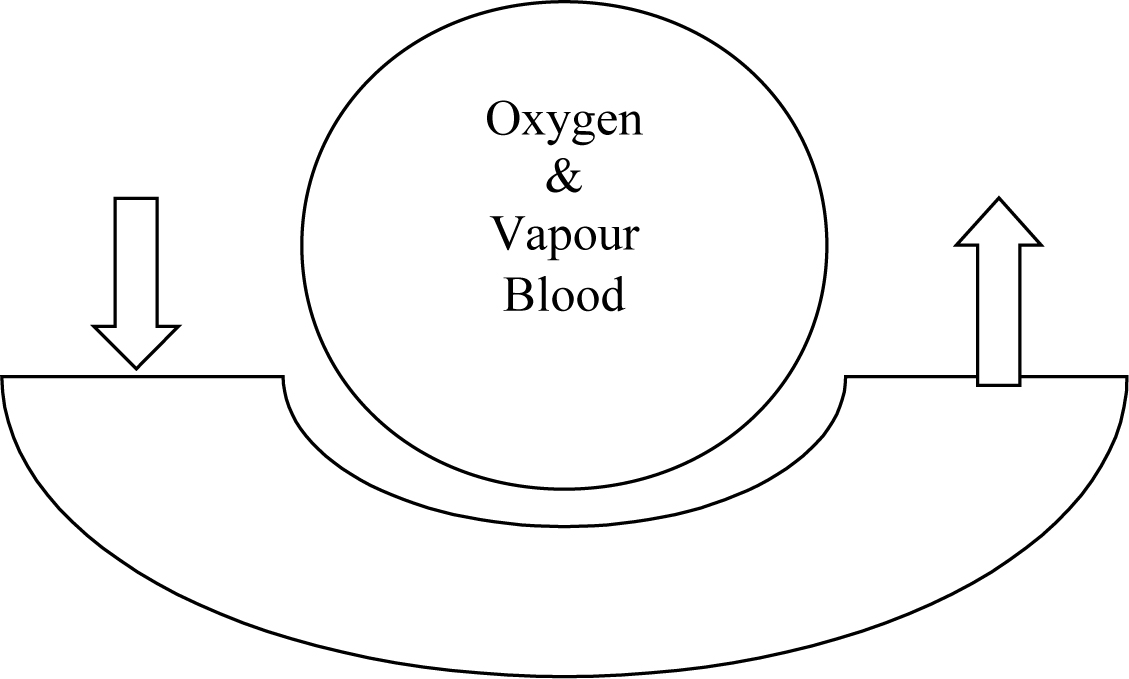
Figure_2
Some of the vapour will dissolve in the blood and eventually an equilibrium is reached between blood and vapour (i.e. the number of molecules of anaesthetic entering and leaving the blood in a given time period are equal). The more soluble the drug, the more molecules will dissolve in blood and the longer it will take for the equilibrium to be reached between vapour in the alveoli and blood. The converse is true for insoluble drugs. The anaesthetic effect is only achieved when the concentration in the blood is the same as that in the gas in the alveoli. The result of this is that the more insoluble a drug in blood, the faster its onset of action and change in depth of anaesthesia as equilibrium is achieved more rapidly. This solubility is expressed using the blood: gas solubility coefficient. The lower the solubility coefficient, the less soluble the vapour, and the faster its onset of action or change in depth of anaesthesia.
Oil: Gas Solubility Coefficient
Although the blood:gas solubility coefficient is a factor in the time it takes for the offset of an inhalational drug, it is not the most important, this is how lipid soluble an inhalational drug is, and expressed as the oil:gas solubility coefficient.
All lipid soluble drugs behave in a similar way. If you take the human body you can divide it into three theoretical compartments; the blood, the tissues that have a rich vascular supply and little fat (e.g. brain, heart) and tissues that have lots of fat and a poor vascular supply (e.g. adipose tissue). These three compartments are interlinked as shown in fig 3.
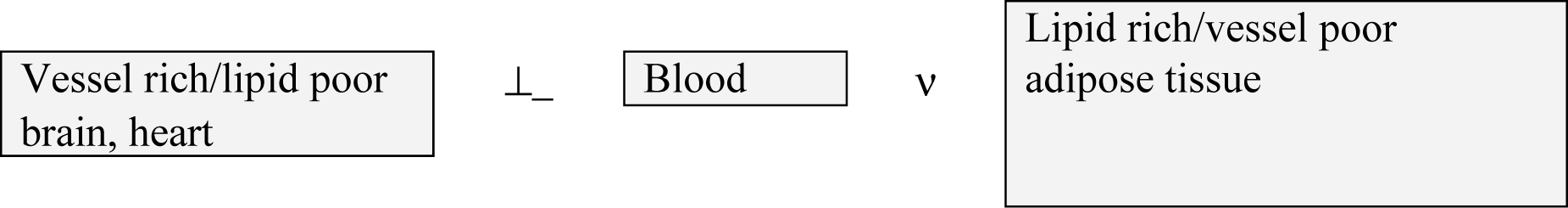
Figure 3: The three key compartments
When you give an inhalational anaesthetic drug, you are in effect infusing a drug. Initially the blood compartment becomes saturated or full, followed shortly afterwards by the vessel rich/lipid poor compartment. If you stopped the drug now, the patient would wake quite rapidly as the drug concentration in the blood would fall. This would lead to redistribution from the vessel rich compartment into both the blood from where it will be excreted and a small amount will redistribute to the vessel poor/lipid rich compartment. If however you continued to give the inhalational drug, the adipose tissue would slowly absorb more and more of the drug; the longer the inhalational drug is given, the larger the dose of drug that is stored in adipose tissue. Once the anaesthetic is stopped, the drug then slowly redistributed into the blood before being excreted and some will be distributed to the vessel rich group, thereby delaying recovery.
Therefore if an inhalational drug is not very soluble in lipid, very little will be stored in the adipose tissue and therefore it will not take long to be excreted from the body.
Again, the lower the oil:gas solubility coefficient, the less lipid soluble the drug and the faster it’s offset.
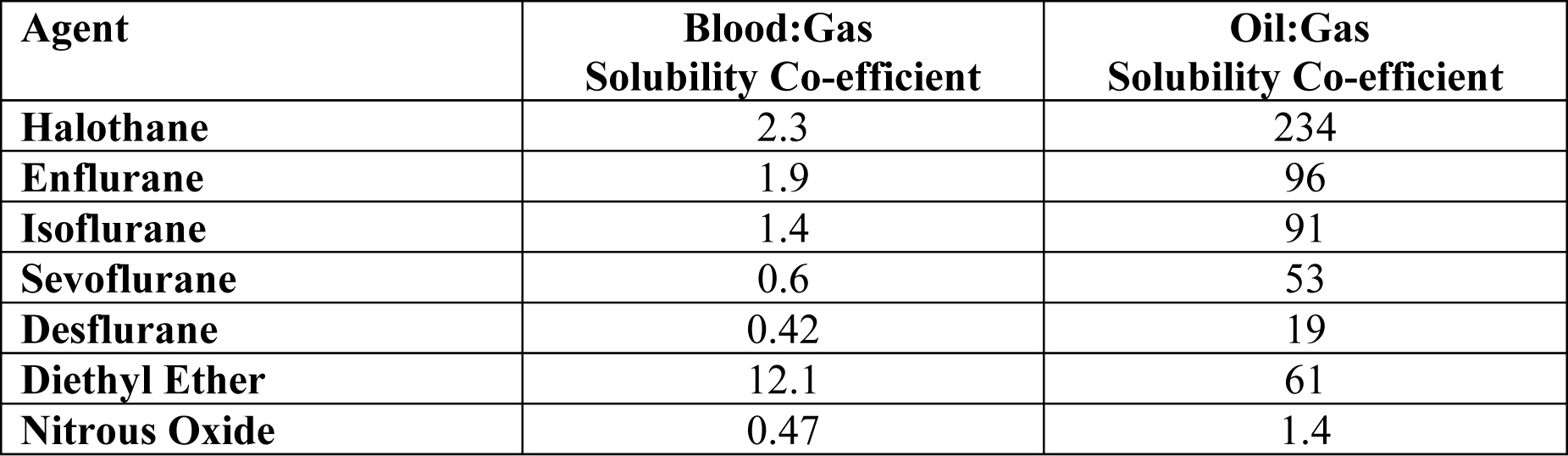
Table 1; Comparison of blood:gas & oil:gas solubility co-efficients of different inhalational drugs.
References
- http://www.baxter.com/products/anesthesia/anesthetic_pharmaceuticals/downloads/su prane.pdf
- http://www.rxabbott.com/pdf/ultanepi.pdf
- Sasada M, Smith S. Drugs in Anaesthesia & intensive Care. 3rd Edition. Oxford University Press 2003.
- Bovill J.G, Howie M.B. Clinical Pharmacology for Anaesthetists. 1st Edition. W.B.Saunders 1999.
- Pinnock C et al. Fundamentals of Anaesthesia. 2nd Edition. Greenwich Medical Media 2002.



