Paediatric Anaesthesia
QUESTIONS
Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation.
- The aetiology of airway obstruction following cleft palate repair may include:
- Laryngospasm
- Newly repaired palate contacting the posterior pharyngeal wall
- Retained throat pack
- Bleeding and blood clots in the airway
- Respiratory depression due to opioid use
- In children undergoing CP repair:
- Airway obstruction is more common in children with micrognathia
- Syndromes that do not affect the airway do not increase the risk of postoperative airway obstruction
- Airway obstruction is most likely to occur in the immediate postoperative period
- There is good evidence that dexamethasone reduces the incidence of postoperative airway obstruction
- The tongue gag should be released every 90 minutes to reduce the risk of significant tongue swelling
- Nasopharyngeal airways (NPA) in children following CP repair:
- May be constructed from standard uncuffed endotracheal tubes
- Should not be inserted until airway obstruction becomes problematic
- Should be placed so the tip lies beyond the epiglottis
- Require higher levels of postoperative observation than children without NPAs
- Require regular suctioning to maintain patency
- In the postoperative period:
- If airway obstruction occurs positioning the child lateral or prone may be sufficient
- Oropharyngeal airways are contraindicated due to the risk of damaging the surgical repair
- If re-intubation is required it is unlikely to be more difficult than for the original procedure
- Oxygen therapy is mandatory for all children in the first 24 hours following surgery
- Appropriate observation includes an apnoea monitor if the child is less than 12 months old
INTRODUCTION
Cleft lip and palate (CLP) is one of the commonest congenital abnormalities, with an incidence of 1 in 700 – 800 live births. The abnormality causes feeding, speech and orthodontic problems and the psychosocial effects can be significant. Surgical repair is not without challenge but may be achieved successfully even in settings with limited resources. An overview of anaesthetic considerations pertinent to CLP repair has been described in ATOTW 72 [1]. Airway complications, including airway obstruction are the most significant postoperative concerns. This article will focus on the aetiology and risk factors for airway complications after cleft palate (CP) repair and address ways in which they may be prevented or managed.
AETIOLOGY OF AIRWAY COMPLICATIONS AFTER CLEFT PALATE REPAIR
Airway complications after CP repair range from episodes of mild stertor (noisy, snoring-like breathing resulting from obstruction in the naso- or oropharynx) to complete loss of the airway requiring re- intubation. Airway complications may occur in the immediate postoperative period, or on the ward postoperatively. It is useful to consider the aetiology of airway obstruction, although in reality, the cause may be multifactorial.
Congenital abnormalities associated with micrognathia:
Surgery for CP repair aims not only to close the defect but also to reconstruct the soft palate musculature to promote better speech development. Obstruction may occur postoperatively particularly in young infants who are obligate nasal breathers, as the tongue falls back and the newly repaired palate rests against the posterior pharyngeal wall. This is more likely to occur in children who have a small mandible (micrognathia), and limited space in the oral cavity to accommodate the tongue (see congenital syndromes below).
Anaesthetic or surgical complications:
- Retained throat pack
- Bleeding or blood clots in the airway
- Laryngospasm
- Reduction in pharyngeal tone due to the residual effects of volatile agents
- Respiratory depression due to opioid analgesia
- Laryngeal oedema secondary to difficult intubation
- Tongue oedema secondary to prolonged insertion of the mouth gag
RISK FACTORS FOR AIRWAY COMPLICATIONS AFTER CLEFT PALATE SURGERY
Syndromes and congenital abnormalities
The risk of postoperative airway obstruction after cleft palate repair is increased in the presence of a named syndrome or other congenital anomaly, even if these do not specifically affect the airway. The overall incidence of postoperative airway obstruction after CP repair is around 6% in all patients; the incidence rises to 25% in children who have a congenital abnormality of any type.
Airway difficulties at the time of CP repair are particularly common in children with micrognathia and are predicted by:
- Airway difficulties after birth, including respiratory problems, feeding difficulties, aspiration and apnoeas
- Airway intervention required in the first few weeks or months of life, including lateral or prone positioning, nasopharyngeal airway, tongue-lip adhesion, or in the most severe cases, tracheostomy.
This remains true even if the airway appears to be relatively normal at the time of surgery. These children may be compensating well for a minor degree of micrognathia, but airway compromise becomes apparent postoperatively after cleft repair.
Common syndromes and congenital abnormalities associated with airway problems.
Pierre Robin Sequence
Pierre Robin sequence (PRS) describes the clinical triad of micrognathia, retroglossoptosis and cleft palate. It is thought to be due to mandibular hypoplasia during early development; the tongue is pushed back high into the oral cavity and prevents closure of the palatal shelves, resulting in the typical, wide, U-shaped cleft palate seen in over 90% of patients. Micrognathia is seen in the majority of patients and is most noticeable in early infancy; catch up growth occurs so that by 5-6 years of age, most non- syndromic children have a normal mandibular size [2].
PRS may be an isolated anomaly (50% of patients) or found as part of another syndrome, such as velocardiofacial syndrome (7%), Stickler syndrome (20%) or Treacher Collins syndrome (5%).
Velocardiofacial syndrome
Velocardiofacial syndrome (VCF) is a genetic syndrome associated with a wide spectrum of clinical features. Cardiac anomalies are seen in 75% of cases (typically conotruncal abnormalities such as interrupted aortic arch, truncus arteriosus, tetralogy of Fallot), thymic abnormalities (impaired immune function) and parathyroid abnormalities (hypocalcaemia). 10% of cases with VCF have Di George syndrome (conotruncal abnormality, hypoarathyroidism, hypocalcaemia, immune deficiency). Patients have unique facial characteristics, mild developmental delay and psychiatric disorders. The palatal abnormality may be a submucous cleft associated with hypernasal speech, or overt cleft palate. 15-20% of patients with VCF have Pierre Robin sequence [3].
Stickler syndrome
Stickler syndrome is also known as hereditary arthro –opthalmopathy. It describes a group of collagen disorders associated typical facial features (flat face, small nose, flat nasal bridge), cleft palate and eye abnormalities (high myopia, glaucoma, retinal detachment, cataract), hearing or joint problems (hypermobility, arthritis).
Treacher Collins syndrome
This is an autosomal dominant syndrome with variable penetrance and clinical severity, associated with cleft palate and bilateral mandibular and maxillary hypoplasia, with typical beaked nose, ear abnormalities and eye abnormalities (anti mongoloid slant, colobomas of the lower lids, absent eyelashes)
CHARGE association
This is an autosomal dominant condition associated with cleft palate (30-50% of patients), dysmorphic features and a non-random association of Coloboma, Heart defect, Atresia choanae, Retarded growth and development, and/or CNS anomalies, Genital hypoplasia, and Ear anomalies and/or deafness. Other anomalies such as oesophageal atresia/tracheosophageal fistula may be present.
Timing Of Surgery
The timing of CP surgery is a compromise. Early repair aids speech development but may promote mid-face growth abnormalities, and the optimal age for surgery remains a topic of debate. The Eurocleft Study of 210 centres performing CLP repair found 194 different protocols for surgery! In our centre, children with cleft lip and palate undergo lip and anterior palate repair at 3 months of age, and palate repair at 6 months of age. However, in children with micrognathia and Pierre Robin sequence surgery may be deferred until the age of nine months or older as this allows the mandible to grow and reduces postoperative airway complications.
Timing of CP surgery in low-income settings is further complicated by environmental considerations. Postoperative airway problems are higher in infants, irrespective of the type of surgery undertaken, so a policy of deferred surgery in all children may be appropriate to minimise airway complications. However, for some children with CP with severe feeding difficulties early cleft surgery may have a survival benefit.
Preoperative condition of the patient
Perioperative respiratory complications are more common in children who have symptoms of an upper respiratory infection at the time of surgery and deferral of surgery should be considered. Deferral should also be considered in the presence of other intercurrent infections (including malaria in low- income settings) and in children with untreated congenital cardiac disease, as treatment of cardiac disease should take precedence over cleft palate surgery. Children with severe airway compromise, or those with CP in resource-poor settings may be severely malnourished prior to surgery. Preoperative feeding, including nasogastric feeding with vitamin supplementation should be considered before surgery. Preoperative condition of the patient Perioperative respiratory complications are more common in children who have symptoms of an upper respiratory infection at the time of surgery and deferral of surgery should be considered. Deferral should also be considered in the presence of other intercurrent infections (including malaria in low- income settings) and in children with untreated congenital cardiac disease, as treatment of cardiac disease should take precedence over cleft palate surgery. Children with severe airway compromise, or those with CP in resource-poor settings may be severely malnourished prior to surgery. Preoperative feeding, including nasogastric feeding with vitamin supplementation should be considered before surgery.
Surgical Technique
A detailed discussion of operations and their relative merits lies beyond the scope of this article, but the choice of surgical technique may influence the postoperative course. Multiple surgical approaches to CP repair have been described. Von Langenbeck’s approach involving bipedical mucoperiosteal flaps is the oldest and simplest operation in common use. This results in a relatively short palate with poorer speech outcomes but a lower incidence, severity and shorter duration of postoperative hypoxaemia than more extensive repairs. In our centre surgeons undertake the GOSta Sommerlad repair with radical muscle retropositioning, which minimises detrimental effects on maxillary growth, and maximises velopharyngeal function [4]. Patients with severe micrognathia may require a temporary nasopharyngeal airway postoperatively.
Traumatic Intubation
There is an increased incidence of difficult laryngoscopy in children undergoing CP repair, particularly in the presence of a bilateral cleft lip or micrognathia. Multiple attempts at laryngoscopy and a traumatic intubation may lead to airway oedema and contribute to postoperative airway complications. Detailed preoperative assessment including assessment of micrognathia is essential, as is careful planning of intubation technique which may include the use of aids such as bougies, laryngeal masks and possibly fibreoptic intubation. If initial attempts at intubation fail repeated use of the same technique is not acceptable and consideration should be given to waking the child up.
Application of the Surgical Gag
During surgery a tongue gag is necessary to provide adequate exposure of the palate. The pressure exerted by the gag may lead to massive swelling in the immediate postoperative period. The cause of the swelling may be venous stasis (exacerbated by the reverse Trendelenberg position adopted by some surgeons), haematoma formation, ischaemia and necrosis. The complication occurs rarely, with only nine cases reported in the literature, but it has been suggested that application of the gag for unusually long periods may be a significant factor. During surgery the gag should be released every 90-120 minutes to allow for tongue reperfusion.
PERIOPERATIVE STRATEGIES TO MINIMISE AIRWAY COMPLICATIONS AFTER PALATE SURGERY
Intraoperative strategies
Regional Anaesthetic Techniques
The use of opioids in infants and young children raises justifiable concerns about sedation and respiratory depression in the postoperative period. Regional techniques can reduce the need for their use. Infraorbital nerve blocks are effective for cleft lip repair and obviate the need for opioids but there is no comparable block in routine use for CP repair. Direct block of the greater and lesser palatine nerves and the naso-palatine nerve anteriorly may damage the vascularity of the palate flaps, but these nerves may be effectively blocked during infiltration of the area. Our practice is for surgeons to infiltrate the surgical field with a solution of lignocaine with adrenaline 1:200,000 to provide analgesia, improve the surgical field and reduce opioid requirements.
Dexamethasone
Dexamethasone 0.25mg/kg may be given perioperatively to reduce upper airway oedema and problems at extubation, although there is no evidence for its efficacy in a surgical setting. Most experience comes from trials in intensive care where the results are equivocal, although a benefit has been suggested in children at high-risk of post-extubation airway compromise. Our usual practice is to use dexamethasone when intubation has been difficult or we perceive an increased risk of postoperativeairway oedema.
Elective Nasopharyngeal Airway Insertion
A nasopharyngeal airway (NPA) may be inserted electively at the end of surgery to prevent problems with postoperative airway obstruction. NPAs are well tolerated and effective and are part of our routine management strategy in a child with predicted postoperative airway compromise:
- Children with Pierre Robin sequence
- Children with other syndromes affecting the airway
- Children who needed an NPA to maintain airway patency at any point prior to operation
- Children who develop airway obstruction with loss of pharyngeal tone following induction of anaesthesia. Our experience is that these children are more likely to experience problems with postoperative obstruction and may require an NPA postoperatively.
The NPA is placed at the end of surgery when the child is still anaesthetised. This ensures that the NPA can be inserted to the correct length under direct vision. The tip of the NPA should protrude from behind the soft palate, but be placed above the epiglottis to avoid laryngeal irritation when the child is awake. The NPA should be firmly secured in place. Whilst an NPA can also be inserted when the child is awake if the child develops unexpected airway obstruction, this may cause distress and risks
bleeding or damage to the surgical repair.
Our incidence of postoperative airway problems has fallen markedly since the use of NPAs became routine. In our experience the majority of children with an NPA inserted electively only require it for the first postoperative night and the NPA can usually be removed the day following surgery.
Purpose-made, preformed NPAs are available from Polamedco (Camcare Gels, UK) in sizes 3.0- 4.5mm. They are soft and flexible and have a flange to prevent inadvertent loss in the upper airway. Alternatively, NPAs can be fashioned from a tracheal tube cut to the appropriate length with flanges to allow it to be secured. Children with NPAs in situ following CP repair represent a high-risk group who require close postoperative observation. Detailed instructions for sizing and insertion, and guidelines on appropriate care of the child with an NPA may be found in the appendix to this article.
Tongue Suture
A tongue suture may be employed following cleft palate surgery to relieve airway obstruction in the postoperative period. A heavy nylon or prolene suture is inserted into the dorsal surface of the tongue in its posterior third at the end of surgery, tied in a large loose loop and the end taped to the child’s lower jaw. If airway obstruction develops, traction on the suture will lift the tongue from the posterior pharyngeal wall. The main benefit from a tongue suture comes in the first few hours after surgery and if not required it is easily removed. This technique does not form part of our routine practice but a recent US survey revealed around 40% of surgeons use a tongue suture all the time after cleft palate repair and around 40% never use the technique. There is no data on the effect of tongue sutures on outcomes.
Management of extubation
At the end of the procedure the pharynx should be inspected for blood clots and to check haemostasis. Particular care should be taken to remove throat packs and this should be included as part of the routine swab count included in the World Health Organisation Surgical Safety Checklist. Thereafter, instrumentation of the airway should be kept to a minimum to avoid disrupting the surgical repair and causing bleeding. Extubation should only occur once the child is fully awake and protective airway reflexes have returned.
Managing the child with airway obstruction after cleft surgery
Airway obstruction is most likely to occur in the immediate postoperative period, although airway problems may continue to present up to 48 hours post-surgery. Cases of massive tongue swelling usually present within 90 minutes of the end of the operation.
Simple Manoeuvres
For mild cases of stertor positioning the child lateral or prone position is often effective. Temporary application of continuous positive airway pressure until the child has fully recovered may suffice. For more severe cases, intervention will be required. Where possible, an oropharyngeal airway should be avoided as insertion risks damage to the surgical repair. However, they are readily available and anaesthetists are familiar with their use. In extremis the use of an oropharyngeal airway may be lifesaving.
Nasopharyngeal Airways
Even if not inserted electively at the end of surgery, NPAs can still be utilised if problems develop at any point in the postoperative period. One nostril is often larger than the other and it is useful if this information is recorded in the operation note or records in case an NPA is needed. Generally, because the flange on tubes faces to the left, the right nasal airway is preferred if it is of adequate size. Where possible the operating surgeon or team should be consulted before an NPA is used. Guidelines for insertion and subsequent care may be found in the appendix.
Re-intubation
Re-intubation may be required if simple manoeuvres cannot establish a safe airway. Difficult intubation should be anticipated as postoperative swelling and bleeding may distort the view at laryngoscopy. Particular attention should be paid to massive tongue swelling due to excessive pressure from the tongue gag and early re-intubation is advised if there are any concerns about such swelling after CP repair. The appropriate technique for re-intubation will be informed by experience at the initial intubation, the equipment available and the anaesthetist’s skill set. Wherever possible, care should be taken to avoid damage to the newly repaired palate. Re-intubation is most likely to be needed in the immediate postoperative period when the child is still within the theatre environment. However, if the child is on the ward when problems arise and there is time, they should be returned to theatre or other appropriate place where skilled assistance and equipment is readily available.
Postoperative Monitoring
All children should be monitored in the recovery area until they are fully awake, their pain is well controlled and there is no further bleeding. The use of continuous pulse oximetry is mandatory, and temperature, blood pressure, ECG and capnography should also be available.
On the ward, careful monitoring is required for at least 24 hours to allow early detection of airway problems. Appropriate observations include:
- Oxygen saturation
- Respiratory rate
- Heart rate
- Apnoea monitor if the child is less than 12 months
Where this monitoring is provided will depend upon the facilities available. Adequate supervision will usually require a location capable of providing higher-level care, such as a high dependency unit, and some institutions electively admit children at high risk of airway complications to intensive care on the first postoperative night. Oxygen should be available, particularly given the predilection of CP repair patients to postoperative hypoxaemia, but the use of oxygen should be reserved for those who need it (oxygen saturation below 94%). Unwarranted oxygen therapy in children with severe obstructive sleep apnoea has the potential to mask evolving airway obstruction as the hypoxic drive to ventilation is removed.
SUMMARY
- Airway obstruction is a potentially life-threatening complication following cleft palate repair
- Obstruction is more common in children with syndromes, particularly those associated with micrognathia
- Nasopharyngeal airways are a very effective way to prevent postoperative airway obstruction and should be inserted electively at the end of surgery if problems are expected
ANSWERS TO QUESTIONS
- All true. Airway obstruction is often multifactorial and may be due to factors that are not specific to CP repair.
- TFTFT.
- TFFTT. We recommend the elective use of NPAs in children at risk of postoperative obstruction, the aim being to prevent problems rather than wait until they develop. Children with NPAs in situ therefore represent a higher risk group who require more postoperative observation.
- TFFFT. Oropharyngeal airways should only be avoided if possible. If airway obstruction may be alleviated with the use of an oropharyngeal airway then it should be used and any damage to the surgical repair assessed once control of the airway has been established. Oxygen should be used only when needed (i.e. to maintain SpO2 above 94%) as excessive use may abolish hypoxic drive in children with obstructive sleep apnoea.
WEBLINKS
- Great Ormond Street guidelines on preparation and management of nasopharyngeal airways. Available at: http://www.gosh.nhs.uk/clinical_information/clinical_guidelines/cpg_guideline_00024 (accessed 7th June 2011)
- World Health Organisation Surgical Safety Checklist. Available at: http://whqlibdoc.who.int/publications/2009/9789241598590_eng_checklist.pdf (accessed 7th June 2011)
REFERENCES and FURTHER READING
- Rawlinson E. Anaesthesia for Cleft Lip and Palate. World Anaesthesia Society Tutorial available at http:/totw.anaesthesiologists.org accessed 28th May 2011.
- Lewfik TL, Trinh N, Teebi AS. Pierre Robin Syndrome. eMedicine available at http://emedicine.medscape.com/article/844143-overview#aw2aab6b2
- Horenstein MS, Forbes TJ, Ardinger R et al. Velocardiofacial Syndrome. eMedicine available at: http://emedicine.medscape.com/article/892655-overview accessed 18th December 2010
- Patel PK, Ramaswamy R, Grasseschi MF et al. Craniofacial: Cleft Palate Repair. eMedicine available at http://emedicine.medscape.com/article/1279283-overview accessed 30th October 2010. Further information about surgical techniques for repair of cleft palate.
APPENDIX: NASOPHARYNGEAL AIRWAYS
Nasopharyngeal Airway Size
Diameter
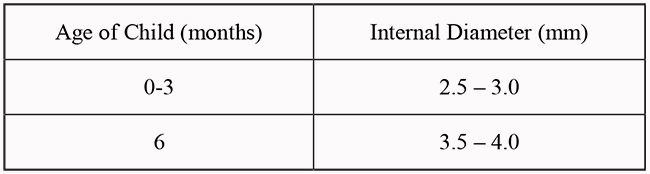
The correct internal diameter of the NPA may be estimated from the size of endotracheal tube used during surgery; the same size or one 0.5mm smaller will be appropriate. Alternatively, size may be determined from the following table:
Length
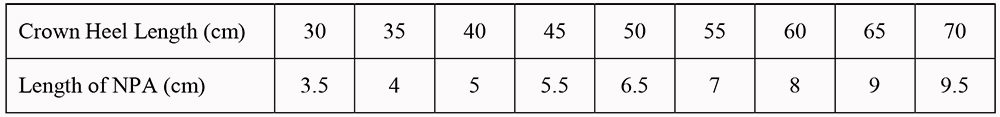
If the NPA is inserted in theatre the surgeon will determine the correct length under direct vision (with the tip beyond the tongue but above the epiglottis). Alternatively, the correct length may be determined from the following table:
Preparation of an NPA
Preformed NPAs are available that are soft and flexible. Their disadvantage is that they are of fixed length, and if the NPA is too long for the child it will tend to move and protrude from the nose. There are a variety of methods by which an NPA can be constructed from a standard endotracheal tube. Many staff at our institution prefer custom made NPAs as they can be sized more precisely and are easier to secure and manage. Details including photographs of our preferred construction technique may be found on the Great Ormond Street website (see weblinks above). A summary of the technique is as follows:
- Assemble an ETT of appropriate diameter (see above), a tracheal tube holder (0.5mm smaller than the ETT) and a non-absorbable suture
- Cut the ETT to the required length (see above)
- Trim the tracheal tube holder to reduce pressure points around the nose
- Fit the tube holder and ETT together
- Ensure blue line on ETT faces upwards
- Suture the two together with 3 to 4 sutures on either side
An alternative technique is to split a standard endotracheal tube longitudinally to the desired length. It is better to make 3 longitudinal cuts and then remove one of the resulting 3 flanges, leaving 2 flanges to attach the NPA to the child’s face. Simply making 2 cuts produces narrowing when the flanges are folded back to tape to the cheeks.
Insertion of a Nasopharyngeal Airway
In Theatre:
This is the preferred location for insertion, and should be done by the operating surgeon. The operation note should clearly record the size and length of the NPA as those caring for the child will need this information.
Preformed NPAs may be secured by means of long sutures inserted in both sides of the flange with the ends taped to the cheeks. NPAs constructed as above should be secured with tapes tied through the loops of the tracheal tube holder.
Postoperatively:
If an NPA is required postoperatively it should be inserted by those with appropriate training and experience, and after discussion with the surgical team. One nostril is often larger than the other and this information should be clearly available on the operation note.
The following instructions are taken from the ward-based protocol for NPAs at our institution:
- Adopt universal precautions
- Assemble equipment – NPA, lubricant and tapes to secure
- Ensure child is restrained and nostrils are clear
- Have oxygen and suction available
- Wash hands and apply non-sterile gloves
- Apply lubricant to NPA
- Insert NPA into largest nostril
- Always avoid excessive force
- If difficulty is experienced:
- Check that the correct size and enough lubricant is being used
- Attempt insertion via the other nostril
- Pass suction catheter through the nostril and insert the NPA using the suction catheter as an introducer, removing the catheter as soon as the NPA is in place
- Pass tapes through the loops of the tracheal tube holder and then onto the face
- Secure the NPA
- Perform suction of the NPA (see below)
- Clear away equipment and wash hands
Monitoring a Child with an NPA
Appropriately trained staff should nurse children with NPAs. The following should be monitored and recorded hourly:
- Oxygen saturation
- Respiratory rate
- Heart rate
- Amount of oxygen required (if applicable)
- Apnoea monitor – if the child is less than 12 months
Maintain oxygen saturations between 94% and 100%
Care of the NPA
The NPA should be maintained according to the following guidance:
- Suction will be required regularly using a suction catheter
- Catheters should not be advanced beyond the end of the NPA, so the length of the NPA must be known. This needs to include the extra length of the tracheal tube holder or other connector if used – otherwise the distal tube may remain blocked.
- Catheters should not exceed 50% of the internal diameter of the NPA as this allows the child to breathe whilst suctioning occurs.
- Appropriate catheter size may be estimated from twice the internal diameter of the NPA e.g. a size 4.0 NPA will require an 8Fr catheter
- Suction should be done routinely before and after feeds or 2-4 hourly if the child is on continuous feeds
- There is a risk that secretions or blood will occlude the NPA at any time. Suction should be performed as clinically indicated to clear the NPA.
- Small amounts of saline may be instilled occasionally to aid with clearing secretions from the NPA, but irrigants should not be used excessively.
- If the NPA becomes blocked or it falls out it should be replaced immediately
- A completely prepared spare airway of the correct size should be available at the child’s bedside and accompany the child at all times.
- A small amount of feed may come up the NPA before, during and after feeds. If this is excessive feeds should be stopped and the child assessed by their clinical team.



