Intensive Care Medicine
KEY POINTS
- Prehospital emergency anaesthesia (PHEA) is a high-risk intervention that can have a significant positive impact on patient outcome.
- Careful patient selection is of paramount importance. Suitable indications include patients with airway compromise, ventilatory failure, those requiring specific neuroprotection, and patients whose predicted clinical course suggests the need for emergency induction of anaesthesia either prior to transportation to hospital or shortly after arrival at hospital.
- Weather conditions, equipment availability, patient position, scene dynamics, and team competencies can all contribute to increased difficulties with the safe delivery of anaesthesia in the prehospital setting.
- Choice of drugs for induction and maintenance should be adapted according to the haemodynamic status and underlying condition of each patient.
- The use of C-spine immobilisation, cricoid pressure, and ketamine as an induction agent represent areas of controversy. However, an evolving evidence base informs practice in these areas.
INTRODUCTION
Prehospital emergency anaesthesia (PHEA) refers to the induction of anaesthesia and securing of the airway in the prehospital environment. It is a modified form of rapid sequence induction (RSI) and intubation. PHEA is inherently high risk because of both patient factors and the prehospital environment. Many factors need to be considered and addressed in order to minimise risks. Prehospital anaesthesia has been described as a ‘‘desirable intervention in relatively few patients that can result in unnecessary morbidity and mortality if performed poorly.’’1 The 2007 National Confidential Enquiry into Patient Outcome and Death (NCEPOD) report ‘‘Trauma: Who Cares?’’ looked at areas that potentially contribute to preventable death in major trauma. This report identified that an inadequate airway was secured in 42 of 438 cases and that 72.9% of those with severe head injury and a Glasgow Coma Scale (GCS) score less than 9 did not undergo PHEA.2
WHY? FOR WHOM?
The risks associated with performing PHEA need to be balanced against the proposed benefits on an individual patient basis. There are regional and international variations in practice regarding performing prehospital interventions. The 2 extremes of this variation have been referred to as ‘‘stay and play’’ versus rapid transfer ‘‘scoop and run.’’ There is little evidence of one system having advantages over the other.2 Multiple factors need to be considered for each case in which PHEA is considered. These include geographical considerations, mode of conveyance, and clinical competence of responding team and injury/illness distributions. These factors are important determinants in the selection of patients in whom the benefits of PHEA outweigh its risks.
Patient Factors to be Considered in Selecting Patients
- The need for airway protection in patients with actual or impending airway compromise.
- The need for respiratory support. Ventilatory failure can sometimes be improved most effectively by intubation and institution of mechanical ventilation.
- The need for neuroprotection to prevent secondary brain injury.
- Predicted clinical course (eg, a patient with reduced GCS who is combative and who is anticipated to require anaesthesia on admission to hospital to facilitate imaging or treatment. NCEPOD reported in the document ‘‘Trauma: Who Cares?’’ that 31.7% of severely injured patients with an Injury Severity Score >16 required intubation within 30 minutes of arrival. It was concluded that this led to worse clinical outcomes.1 Therefore, in cases in which the predicted clinical course is deterioration to the point at which anaesthesia is likely to be required immediately on arrival at secondary care, then PHEA should ordinarily be performed on scene.
- For humane reasons (eg, in the presence of very severe injuries such as fractures requiring splinting or significant burns).
- Mode of transport, team for transport, and time required for patient transfer to definitive care should also be considered when balancing the benefits of PHEA. In environments with short transfer times (such as British urban environments), the benefit of rapid transfer to a hospital environment may trump the benefit of prehospital interventions.3 The position of the patient and of different team members within the transfer vehicle should also be anticipated as access to the patient during transfer is often limited. For example, a chest injury that may require thoracostomy en route needs to be carefully considered if the injured side is immediately next to the wall of the ambulance or aircraft and therefore not immediately accessible.
INCREASED RISKS AND THEIR MITIGATION
The risks of performing PHEA can be split into environmental factors, operator/human factors, and patient factors. These factors are often interlinked.
Environmental Factors
A variety of environmental factors influence the risks of PHEA.
1. Environmental conditions. Compared with working in the usually controlled, warm, and light hospital environment, attempting PHEA has additional stressors. Distracting noises, an excess or lack of light, wind, rain, members of the public, moving vehicles, steep ground, fuel spills, and so forth will all add to the cognitive load of the operator. This can result in a reduced technical ability to complete the task and a loss of situational awareness, including reduced ability to recognise when errors have occurred.
Environmental conditions will also have an impact on the patients’ temperature as they may be exposed to the elements and become immobile due to injury or illness and on occasion physically trapped. Any reduction in core temperature will be exacerbated following anaesthesia. A reduced core temperature will contribute to coagulopathy and poor outcomes in trauma.4 Steps to actively maintain body temperature by reducing heat loss, attempting active warming, and reducing on-scene time are imperative in this population. A choice of location can sometimes mitigate some of these issues.
Alterations in natural light can also lead to problems. Bright sunlight will cause the intubator’s pupil to constrict, thereby reducing visualisation of the vocal cords in the relative dark of the oropharynx. Positioning the patient with their head facing away from direction of sunlight and creative adaptions to the environment can create shade.
2. Patient access. Patients who require intubation in the prehospital setting are rarely found in convenient locations. Examples include cellars, small bedrooms, inside vehicles, steep banks, rocky hillsides, and narrow alleyways. Several risks are inherent in attempting anaesthesia in locations with restricted patient access. Where possible, the patient should be moved to a location where ‘‘360-degree access’’ can be gained before PHEA is attempted. To normalise the intubation attempt as much as possible and thereby reduce the risk of intubation failure, the patient is best placed at a height at which the intubator can kneel or stand. This may be on a trolley or gurney, which can be adapted to the appropriate height.
3. Accessibility of kit. In an organised hospital theatre environment, equipment and medications are readily available and quickly accessible. In the prehospital setting, all equipment required has to be carried to the scene. Standardisation of kit bags and frequent training drills to familiarise team members with the content and layout of the ‘kit dump’ are essential; this will allow any member of the prehospital team to set up. The kit dump should include airway devices and adjuncts, intubating bougie, suction, oxygen, breathing/ventilating system, monitoring, and drugs (either preprepared or drawn up into labelled syringes; see Table 2). Quantitative waveform capnography is advocated in the United Kingdom and should be considered a
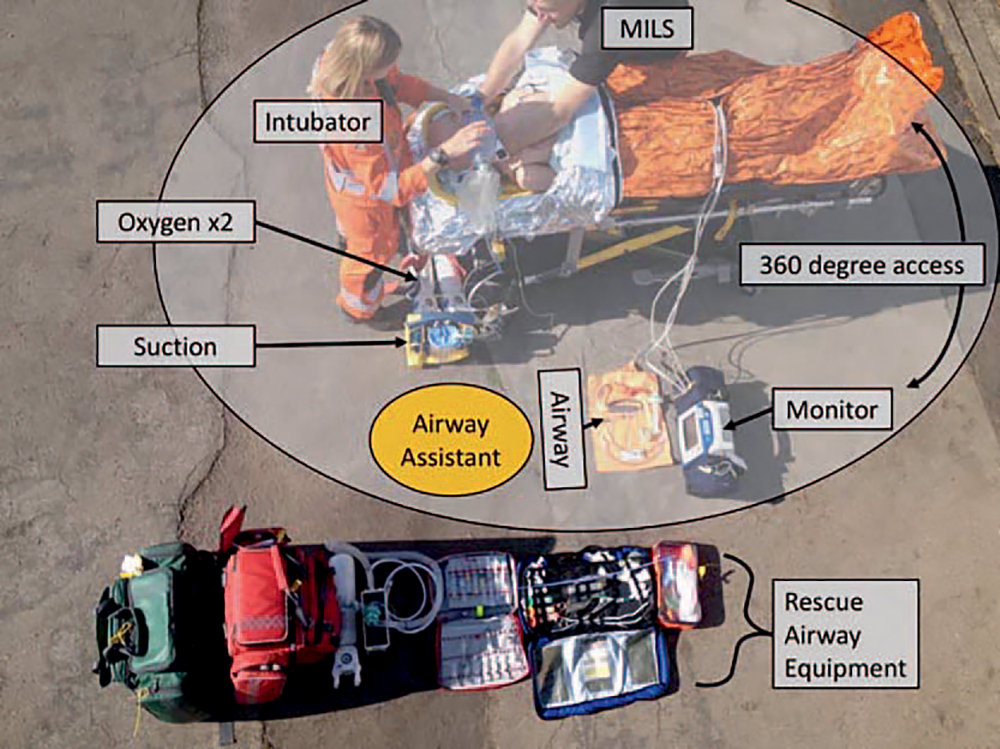
Figure. Kit dump with overlay showing location of equipment and personnel. Position of airway assistant marked in orange. Manual in-line stabilization (MILS) should be used when there is risk of c-spine injury to prevent excessive movement during intubation.
mandatory requirement before commencing a PHEA. In a study by Li et al,5 as many as 3% of emergency intubations resulted in oesophageal intubation. In a US-based study, the use of an end-tidal CO2 trace reduced the rate of unrecognised misplaced tracheal tubes from 9% to 0%.6 Other factors that can aid in detection of oesophageal intubation is the use of video laryngoscopy (as this allows the tube to be observed passing through the cords), auscultation of the chest with a stethoscope, and familiarity with ‘how it should feel’ when hand ventilating a patient via a correctly placed endotracheal tube (Figure).7
Operator/Human Factors
- Comfort and safety. As discussed above, the comfort and safety of the intubator and the rest of the team are important for risk reduction. Personal protective equipment, including appropriate clothing for the weather and temperature, is important, as is appropriate location and positioning of the patient.
- Skill set of the team. Prehospital anaesthesia is a high-risk intervention that should not be attempted by those who have insufficient training or experience. It is paramount that there is a rigorous training programme, that skills are maintained, and that there is regular review of practice.1 All those involved in PHEA should work to a set of standard operating procedures (SOPs) and should be well drilled, such that the whole team knows both what their role is and the standardised way that procedures are done within their organisation.
- Cognitive overload. The prehospital setting often has many rescuers on scene, including health care professionals, other emergency professionals, and the public. Frequently, there is concurrent activity, and there is sometimes more than one casualty. Error reduction is achieved by use of a verbal challenge-response preinduction checklist. SOPs and checklists simplify processes and limit choice to further reduce cognitive load.8 Cognitive load is reduced by confirming availability of equipment, drugs (including dose calculations), and emergency action plans for failed intubation and other potential problems.1 Using checklists can also ensure that those performing PHEA remain appropriately task focused. An example of a checklist is provided in Table 1.
Patient Factors
Patients requiring PHEA will not have undergone standard preoperative assessment. In contrast to elective surgical patients, they will not have been optimised for anaesthesia, and prior airway assessment information will be unavailable. They are a high-risk group, frequently with significant physiological derangement, such as hypovolemia, hypoxia, hypothermia, and metabolic acidosis. Mitigating these factors can be extremely difficult and is not always achievable.
1. Hypovolemia. Induction of anaesthesia in hypovolaemic patients is hazardous; PHEA in underresuscitated hypovolaemic trauma patients is associated with an increase in mortality. These patients should ideally undergo resuscitation with balanced blood products prior to induction of anaesthesia. Damage control resuscitation emphasises the importance of
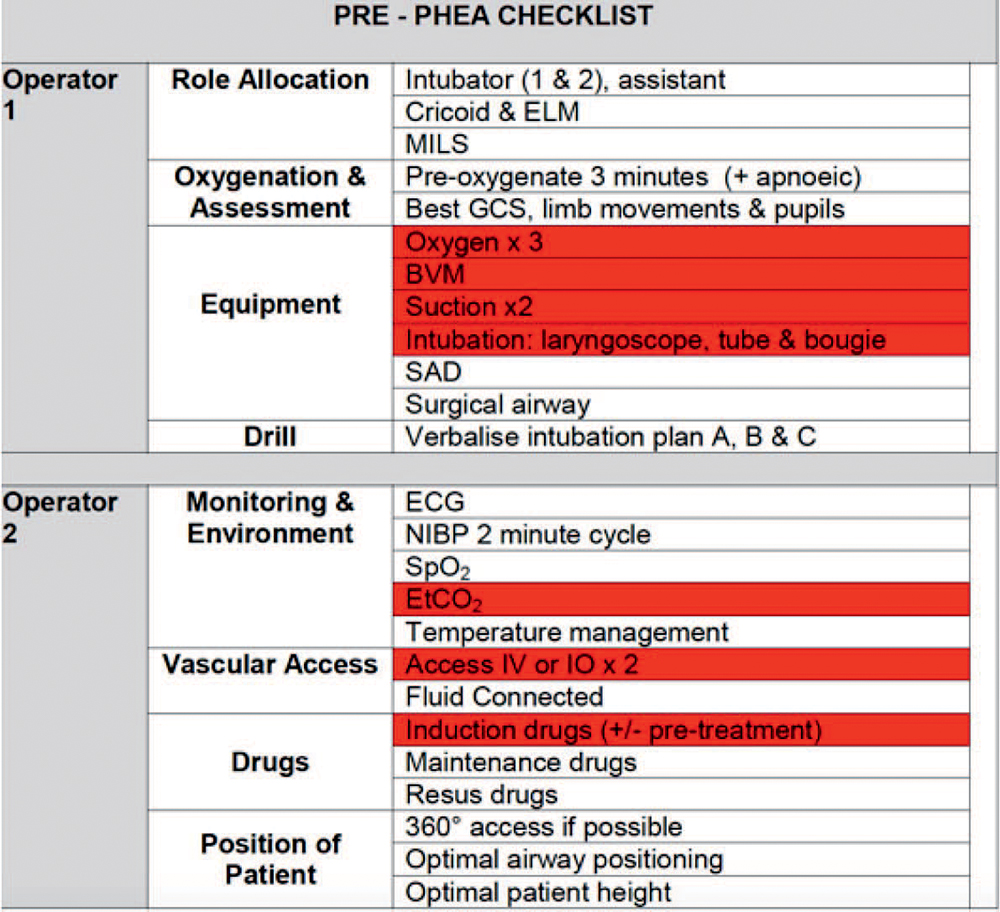
Table 1. Example PHEA Checklist With Core Elements for ‘‘Immediate Induction’’ Highlighted in Red. ELM, external laryngeal manipulation, MILS, manual inline stabilisation, SAD, supraglottic airway device. Taken from South Western Ambulance Service NHS Foundation Trust, Trust Clinical Guideline ID CCG02, ‘‘Pre-hospital Emergency Anaesthesia (PHEA),’’ issued September 1, 2015
appropriate resuscitation with balanced blood products to decrease the detrimental effects of major bleeding, including acidaemia and coagulopathy, within this patient group.9
Prior to achieving definitive haemorrhage control, suitable physiological values to target include a mean arterial pressure of 50mmHg, systolic blood pressure of more than 80 mmHg, or return of a palpable peripheral pulse.10 Acidosis, tracked by point-ofcare estimation of base excess, may be corrected by good resuscitation.
Anaesthetic drugs may further worsen the patient’s haemodynamic profile via drug-induced vasodilation, myocardial depression, and loss of compensatory sympathetic drive. In addition, positive-pressure ventilation in this setting will further reduce preload.
Adequate intravenous access is vital. It is advised to ideally have two sites of reliable, wide-bore venous access and fluid of some type attached for all anaesthesia inductions. This will allow both rapid administration of a 250-mL bolus of fluid if required and easy flushing of drugs that have been administered. The need for adapted doses of induction agents should be considered. As discussed later, vasopressors should be avoided in hypovolaemia, if possible.
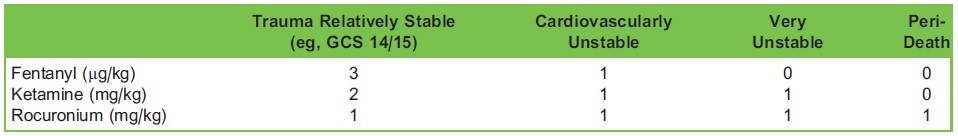
Table 2. Doses of Anaesthetic Agents Adjusted for Patient Condition (Adapted From Ref. 14)
2. Hypoxia. Efforts should be taken to maximise the effectiveness of preoxygenation. Effective preoxygenation in the prehospital setting can be difficult but is best achieved by combining high-flow nasal oxygen and a Water’s circuit. The former can be continued in the apnoeic phase, and this may increase safe apnoeic time by up to 10 minutes.11 For those in whom preoxygenation is difficult because of agitation, judicious sedation can be used to enable effective preoxygenation before attempting PHEA. Ketamine 0.5 to 1 mg/kg intravenously (or 4-5 mg/kg intramuscularly) is the most commonly used agent for this purpose. Whilst midazolam can also be effective, it is used less commonly in this scenario because of concerns about loss of airway patency.
Although, classically, an RSI would not include hand ventilation, in the critically unwell patient, assisted ventilation is commonly used during and following induction of anaesthesia. The risk of gastric inflation and consequential aspiration can be mitigated by keeping inspiratory pressure less than 25 cmH2O.12
3. Hypothermia. Patients should be kept warm with appropriate protection from the weather. In many cases, active warming to ensure maintenance of temperature will also be required.
4. Airway. All prehospital airways should be assumed to be difficult. Many UK critical care teams routinely use a videolaryngoscope and bougie in all intubations. This not only reduces cognitive load for the team by having a standard approach but it also removes a tier of process if the airway is difficult, thereby allowing rapid progression through a difficult airway algorithm.
For trauma patients with a suspicion of cervical spine injury, equipment used for immobilisation, such as cervical collars and blocks, will significantly decrease the best achievable laryngoscopy grade and should be exchanged for manual in-line stabilisation prior to induction of anaesthesia.2
DRUGS FOR INDUCTION
The aim should always be to deliver safe and balanced anaesthesia, tailored to the patient and the skill set of the operator. Many different formulae have been suggested as offering the optimal combination and doses of drugs.13–15 Some are discussed below. It is widely accepted that neuromuscular blockade should be used. A study of paramedic intubations showed an overall success rate of 67.5%, which was increased to 81% by using a sedative and 96.7% by using a neuromuscular blocking drug.1 Adequate neuromuscular blockade has also been demonstrated to significantly increase the probability of success of front-of-neck procedures in ‘can’t intubate can’t oxygenate’ situations.1 This is particularly important as it would be very rare for a patient to be suitable to be woken up in this scenario if PHEA was indicated.
‘3,2,1’ Formula
The 3,2,1 formula, referring to the doses of fentanyl, ketamine, and rocuronium, respectively, has been suggested as the basis for prehospital anaesthesia in trauma.12 This should be further adapted to suit different situations. A 1:1:1 regime has been suggested for cadiovascularly unstable patients. Removal of the fentanyl for very unstable patients has also been suggested, as has administration of just rocuronium in the comatose periarrest patient (Table 2).
A formula of fentanyl, ketamine, and rocuronium was shown to produce superior intubating conditions with improved haemodynamic stability when compared with etomidate and suxamethonium.16 In addition, there is evidence to suggest adrenal suppression can occur even after a single dose of etomidate.16 In a trial of etomidate verses ketamine, 232 patients who were randomised had adrenal insufficiency assessed. Adrenal insufficiency was more likely in the etomidate group, with an odds ratio of 6.7 (95% confidence interval, 3.5-12.7).17
Concerns have been raised regarding the long duration of rocuronium when compared with suxamethonium used in traditional RSIs. However, in most severely injured trauma patients, waking the patient up in the event of failed intubation is not a safe or viable option. Also, a difficult airway is known to become considerably more challenging in a partially anaesthetised patient in whom suxamethonium has worn off.12
Ketamine has a wide margin of error and maintains some sympathetic tone. This makes it a very useful drug in trauma, but caution should be exercised in the elderly as underlying cardiovascular comorbidities may mean the sympathetic drive provided by ketamine is poorly tolerated.18 In addition, in profoundly hypovolemic patients who are catecholamine depleted, ketamine administration can result in hypotension despite its sympathomimetic effects.19
Cardiac Arrest
In patients with return of spontaneous circulation following cardiac arrest, it is important to maintain cardiovascular stability. In this scenario, some authors have suggested use of midazolam 0.1 mg/kg, fentanyl 2 mcg/kg, and rocuronium 1 mg/kg13 for induction, as this may avoid tachycardia and thus improve myocardial perfusion, as well as reduce the hypertensive effects of intubation by preventing an increase in afterload.
Isolated Head Injury
In patients with severe head injury, maintenance of systolic blood pressure of more than 90 mmHg has been shown to reduce mortality.16 To prevent secondary brain injury, a balanced anaesthetic is required. This can be achieved with fentanyl, propofol, and rocuronium, although ketamine augmented with fentanyl is also suitable (see the section ‘‘Current Controversies’’).14 Commonly, a vasopressor infusion or repeated boluses will be required to maintain adequate systolic blood pressure following induction.
DRUGS FOR MAINTENANCE
Practitioners should be aware that induction is merely the start of the anaesthetic. In the immediate post PHEA period, it is essential to reassess the patient, optimise their condition, and prepare for onward transportation. The latter includes the planning and delivery of maintenance anaesthesia. It is very easy to lose momentum once intubation has occurred. The National Institute for Health and Care Excellence (NICE) guidance for PHEA recommends that the time from the call to emergency services to induction of PHEA should be less than 45 minutes. The same guidance also suggests that the time from PHEA to the time of leaving the scene should also be less than 15 minutes. To achieve this, ‘post tube inertia’ must be avoided!20
Several combinations of drugs can be used for maintenance of anaesthesia, including boluses of ketamine, midazolam, and opiate boluses or propofol ± opiate infusions. The final choice of maintenance drugs should be based on the individual patient and experience of the operator. Extra care is required to ensure that maintenance infusions are not obstructed (eg, by a bandage or a frequently cycling noninvasive blood pressure cuff). Repeat doses of a long-acting nondepolarising muscle relaxant should be used.
CURRENT CONTROVERSIES
C-Spine Immobilisation
Cervical spine immobilisation has been a controversial issue for several years, and NICE have issued multiple recommendations on the subject as new evidence has emerged.14 C-spine immobilisation is based on the principle that following trauma, there may be damage to the cervical spine, with the potential for increased damage should the c-spine be moved. Some authors have argued that the significant initial force applied to the spine causes spinal injury and cord damage, not subsequent low-force movements.21 Furthermore, they acknowledge that hard collars may increase intracerebral pressure by reducing venous flow. As many trauma victims at risk of cervical spine injury are also likely to have concurrent head injuries, this is a significant factor to consider.19 In the context of PHEA, c-spine immobilisation with a collar often causes a significant deterioration in best laryngoscopy grade achieved. The most recent NICE guidance suggests that at all stages of the assessment, manual in-line spinal immobilisation should be used, particularly during any airway intervention.20 Patients who are uncooperative or agitated, as well as children, should be allowed to find a comfortable position. In these groups, collars are not recommended, and instead, manual in-line stabilisation should be employed where possible. Collars are contraindicated in patients with compromised airways and spinal deformities such as ankylosing spondylitis.22 In conclusion, airway management should always take priority over c-spine immobilisation.
Routine Use of Cricoid Pressure
In 1961, Sellick23 first described applying backward pressure to the cricoid cartilage to occlude the upper oesophagus, thereby preventing regurgitation of gastric contents into the pharynx. Since then, the value of cricoid pressure has come under scrutiny because of the lack of reliable evidence of benefit and some evidence of potential harm. Evidence against its routine use has included case reports of fatal aspiration despite cricoid pressure,24,25 negative impact on airway patency and ventilation,26 worsening laryngeal view, and trauma to the airway.27 In a recent propensity-based analysis of 1195 patients, Caruana et al27 found no significant relationship between cricoid pressure for prehospital intubation and difficult laryngoscopy. However, the same authors described a statistically significant increased incidence of airway trauma related to laryngoscopy with cricoid pressure applied. Ellis and many others have therefore suggested that practitioners retain both an awareness of the potential problems associated with application of cricoid pressure and a low threshold to remove or reduce the pressure during PHEA.30,31
Ketamine in Head Injury
Ketamine is frequently used in trauma patients because of its known effect in preserving sympathetic tone. It was historically suggested that its use is associated with increased cerebral blood flow, in turn leading to increased intracerebral pressure, with the latter clearly being detrimental in acute head injuries. However, a more recent investigation into the use of ketamine in head injury has refuted this, suggesting instead that its use leads to reduced cerebral oxygen consumption,30 that it does not increase intracerebral pressure in the context of controlled ventilation, and that it may in fact may improve cerebral perfusion. It should therefore be considered safe and potentially beneficial to use in patients with head injuries.31
SUMMARY
PHEA is a high-risk intervention that can have a significant positive impact on patient outcome if conducted appropriately. This tutorial provides an overview of factors to consider for PHEA, including patient selection, environmental conditions, team competencies, and choice of drugs for induction and maintenance of anaesthesia. Suggested further reading includes patient transfer and transport (ATOTW 319 and 330) and the use of ketamine (ATOTW 381).
REFERENCES
- Association of Anaesthetists of Great Britain and Ireland. AAGBI: Safer prehospital anaesthesia 2017. Anaesthesia. 2017;72:379-390. https://www.aagbi.org/sites/default/files/Safer%20pre_hospital%20anaesthesia2017_0.pdf. Accessed May 20, 2018.
- National Enquiry Into Patient Outcome and Death. Trauma: who cares? http://www.ncepod.org.uk/2007report2/Downloads/SIP_summary.pdf. Published 2007. Accessed May 20, 2018.
- Smith RM, Conn AK. Prehospital care—scoop and run or stay and play? Injury. 2009;40(suppl 4):S23-S26.
- Kauver DS, Wade CE. The epidemiology and modern management of traumatic hemorrhage: US and international perspectives. Crit Care. 2009;5:S1.
- Royal College of Anesthetists and Difficult Airway Society. 4th National Audit Project (NAP4): major complications of airway management in the United Kingdom report and findings. https://www.rcoa.ac.uk/node/4211. Published March 2011. Accessed May 5, 2018.
- Silvestri S, Ralls GA, Krauss B, et al. The effectiveness of out-of-hospital use of continuous end-tidal carbon dioxide monitoring on the rate of unrecognized misplaced intubation within a regional emergency medical services system. Ann Emerg Med. 2005;45;497-503.
- Li J, Murphy-Lavoie H, Bugas C, et al. Complications of emergency intubation with and without paralysis. Am J Emerg Med. 1999;17:141-143.
- Lockey DJ, Crewdson K, Lossius HM. Pre-hospital anaesthesia: the same but different. Br J Anaesth. 2014;113(2):211-219. https://doi.org/10.1093/bja/aeu205. Accessed May 20, 2018.
- Cantle PM, Cotton BA. Balanced resuscitation in trauma management. Surg Clin North Am 2017;97:999-1014.
- Gerhardt RT, Strandenes G, Cap AP, et al. Remote damage control resuscitation and the Solstrand Conference: defining the need, the language, and a way forward. Transfusion. 2013;53:9S-16S.
- Chrimes N, Fritz P. The vortex approach. Safe Apnoea time website. http://vortexapproach.org/safeapnoeatime/#apox. Published 2016. Accessed May 20, 2018.
- Awes EG, Campbell I, Mercer D. Inflation pressure, gastric insufflation and rapid sequence induction. Br J Anaesth.1987;59:315-318.
- Lyon RM, Perkins AB, Chatterjee D, et al. Significant modification of traditional rapid sequence induction improves safety and effectiveness of pre-hospital trauma anaesthesia. Crit Care. 2015;19:134.
- Miller M, Groombridge CJ, Lyon R. Haemodynamic changes to a midazolam–fentanyl–rocuronium protocol for prehospital anaesthesia following return of spontaneous circulation after cardiac arrest. Anaesthesia. 2017;72:585-591.
- Hossfeld B, Bein B, Boettiger BW, et al. Recommended practice for out-of-hospital emergency anaesthesia in adults: statement from the Out-of-Hospital Emergency Anaesthesia Working Group of the Emergency Medicine Research
Group of the German Society of Anaesthesiology and Intensive Care. Eur J Anaesthesiol. 2016;33(12):881-897. - Oglesby A. Should etomidate be the induction agent of choice for rapid sequence intubation in the emergency department? Emerg Med J. 2004;21:655-659.
- Jabre P, Combes X, Lapostolle F, et al. Etomidate versus ketamine for rapid sequence intubation in acutely ill patients: a multicentre randomised controlled trial. Lancet. 374:9686:293-300.
- Joint Formulary Committee, ed. BNF (British National Formulary) 74. Chapter 15 ‘‘Anaesthesia’’, London, UK: Pharmaceutical Press; 2017-2018:1234.
- Miller M, Kruit N, Heldreich C, et al. Response after rapid sequence induction with ketamine in out-of-hospital patients at risk of shock as defined by the shock index. Ann Emerg Med. 2016;68(2):181-188.e2.
- NICE guidance [NG39]. Major trauma: assessment and initial management. https://www.nice.org.uk/guidance/ng39/chapter/Recommendations. Published February 2016. Accessed August 16, 2018.
- Benger J, Blackham J. Why do we put cervical collars on conscious trauma patients? Scand J Trauma Resusc Emerg Med. 2009;17:44
- NICE guideline [NG41]. Spinal injury: assessment and initial management. https://www.nice.org.uk/guidance/ng41/chapter/Recommendations. Published February 2016. Accessed May 20, 2018.
- Sellick BA. Cricoid pressure to control regurgitation of stomach contents during induction of anaesthesia. Lancet. 1961;2:404-406.
- Robinson JS, Thompson JM. Fatal aspiration (Mendelson’s) syndrome despite antacids and cricoid pressure. Lancet. 1979;2:228-230.
- Williamson R. Cricoid pressure. Can J Anaesth. 1989;36:601.
- Hartsilver EL, Vanner RG. Airway obstruction with cricoid pressure. Anaesthesia. 2000;55:208-211.
- Caruana E, Chevret S, Pirracchio R. Effect of cricoid pressure on laryngeal view during prehospital tracheal intubation: a propensity-based analysis. Emerg Med J. 2017;34:132-137.
- Ellis DY, Harris T, Zideman D. Cricoid pressure in emergency department rapid sequence tracheal intubations: a risk-benefit analysis. Ann Emerg Med. 2009;50(6):653-665.
- Harris T, Ellis, D, Foster L, et al. Cricoid pressure and laryngeal manipulation in 402 pre-hospital emergency anaesthetics: essential safety measure or a hindrance to rapid safe intubation? Resuscitation. 2010;81(7):810-816.
- Morris C, Perris A, Klein J, et al. Anaesthesia in haemodynamically compromised emergency patients: does ketamine represent the best choice of induction agent? Anaesthesia. 2009;64:532-539.
- Himmelseher S, Durieux ME. Revising a dogma: ketamine for patients with neurological injury? Anesth Analg. 2005;101:524-534.



