Paediatric Anaesthesia
QUESTIONS
Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation. Please answer True or False:
- Food consumption in healthy subjects undergoing elective surgery increases the risk of pulmonary aspiration by:
a. Increasing residual gastric volume
b. Decreasing gastric pH
c. Increasing gastric emptying
d. Decreasing oesophageal sphincter tone
e. In the presence of hiatus hernia - Advantages of reduced duration of fasting are:
a. No increase in residual gastric volume nor reduction in gastric pH
b. Safety and improved patient wellbeing
c. Prevention of hypoglycaemia
d. Improved patient compliance
e. Reduction in post-operative nausea and vomiting - Clear fluids include:
a. Water
b. Fruit juices without pulp
c. Clear tea and black coffee
d. Milk
e. Ice lollies
Key Points
- Preoperative fasting reduces the risk of pulmonary aspiration by allowing time for gastric emptying.
- Regurgitation after feeds in infants less than 6 months of age is very common due to the higher intragastric pressure and lower gastro-oesophageal sphincter tone.
- APAGBI Consensus guidelines currently recommend the ‘2-4-6 rule’ for children.
- A recent study shows that there is a low risk of aspiration in children who are allowed to consume clear liquids up to time of surgery,
INTRODUCTION
Pre-operative fasting, which is defined as the restriction of food and fluid intake for few hours before general anaesthesia or sedation, is one of the cornerstones of perioperative patient safety. Induction of anaesthesia or sedation results in a depression of the gag, cough and swallow reflexes that normally protect the airway, placing patients at risk of pulmonary aspiration, pneumonia and even death should regurgitation or vomiting of gastric contents occur1-3. The aspiration of breast milk or infant formula in particular may result in severe damage to the lungs2.
Subjects are fasted before surgery in order to allow gastric emptying, thus reducing the risk of pulmonary aspiration4. However, prolonged periods of fasting can cause distress, fatigue, irritability, dehydration and biochemical or metabolic imbalances. Recently it has been observed that a reduction in the duration of preoperative fasting is not only safe for the patient, but also improves patient compliance, cooperation and general wellbeing1.
The amount and type of food and fluid that children need preoperatively varies with age. A neonate (a baby less than one month old) needs to be fed often with milk (breast milk, non-human milk or formula) to prevent hunger, thirst and hypoglycaemia, while the physiological needs of the adolescent (child 12 to 18 years) are similar to those of an adult. Children are usually starved of both food and fluid before their surgery to reduce the risk of aspiration during anaesthesia2.
RISK FACTORS FOR PULMONARY ASPIRATION
The mechanisms by which consumption of food and fluids in healthy subjects undergoing elective surgery can increase the risk of pulmonary aspiration are:
- increase in the residual gastric volume
- decrease in gastric pH
- decrease in the tone of the oesophageal sphincter
Fasting aims to overcome these three aspects5. However, there is a lack of clarity on what should be the target gastric volume and pH. Arbitrary critical values have been defined as a pH greater than 2.5 and volume less than 0.4 ml/kg based on primate studies. These values are debated, with some researchers suggesting that gastric acidity is more relevant than volume2, while others still continue to use gastric emptying as the standard.
Gastric emptying of liquids is an exponential process, similar to drug elimination, so the stomach is never fully empty or full, and hence, gastric volume might not in fact be a key criterion for pulmonary aspiration5. Instead, it has been suggested that the three most important risk factors for aspiration are:
- emergency surgery
- light anaesthesia or unexpected response to stimulation
- upper or lower gastrointestinal pathology5
Infants less than 6 months of age have a higher intragastric pressure and lower gastro-oesophageal sphincter tone, so regurgitation is very common. The risk of regurgitation is further increased during inhalational induction because the protective airway reflexes are less active, putting the infant at a higher risk of pulmonary aspiration5. In older children however, the risk of regurgitation and incidence of aspiration pneumonia are low2.
ADVANTAGES OF REDUCED FASTING TIMES
Prolonged fasting in children, especially infants, can result in dehydration, hypoglycaemia, hypovolaemia, hypotension, and other metabolic complications4. Infants have limited energy reserve6, and children become irritable after prolonged fasting5. Given that patients are often starved for much longer periods than recommended, this has resulted in a lot of debate in the recent years about the usefulness of prolonged periods of fasting4. Ideally, children should not be starved for longer than absolutely necessary. Guidelines should prompt when they should be given something to eat or drink rather than the minimum starvation period. This is particularly important for fluids.
Based on current observations, children attending for elective surgery are usually allowed to consume clear fluids up to 2h before surgery, although some centres are allowing more liberal fasting times for clear fluids (see table 1) 5-7.
The Association of Paediatric Anaesthetists of Great Britain and Ireland (APAGBI) 2007 consensus guidelines on perioperative fluid management in children recommend the ‘2-4-6 rule’ for children, which represents fasting times of 2 hours for fluids, 4 hours for breast milk and 6 hours for formula milk/solids for children under 6 months of age. Sweets and lollipops are considered to be solid food, although ice-lollies made with clear juice or water can be considered as fluids5. Babies less than 6 months old may be offered shorter starvation times in some centres, depending on which guidelines are being followed.
The advantages of reducing the duration of fasting are multiple. With shorter fasting times, the residual gastric volume is not increased nor is the gastric pH reduced6. It has been shown to be safe, improves patient wellbeing, reduces postoperative nausea and vomiting1, reduces the risk of hypoglycaemia and hypovolemia8, and aids in smoother induction of anaesthesia6. Studies have shown that children who were permitted fluids up to 2 h before surgery were less thirsty and hungry, more cooperative, and more comfortable compared to those who were fasted for over 6 h8. Finally, this prevents the need for preoperative intravenous fluid and increases the cost effectiveness of patient care7.
The recommended fasting times for breast milk and formula are longer than for clear liquids- 4 hours for breast milk and 6 hours for formula8. Milk is a liquid emulsion, but behaves more like a solid after consumption as it forms curds in the stomach2. Infants who are being breast-fed every 2-3 hours need to fast for longer than this (>4 hours) as breast milk contains considerable amounts of fat which prolongs gastric emptying7. The gastric emptying time is even longer for formula or non–human milk8. The most serious concern is that aspiration of breast milk or formula results in significant lung injury7.
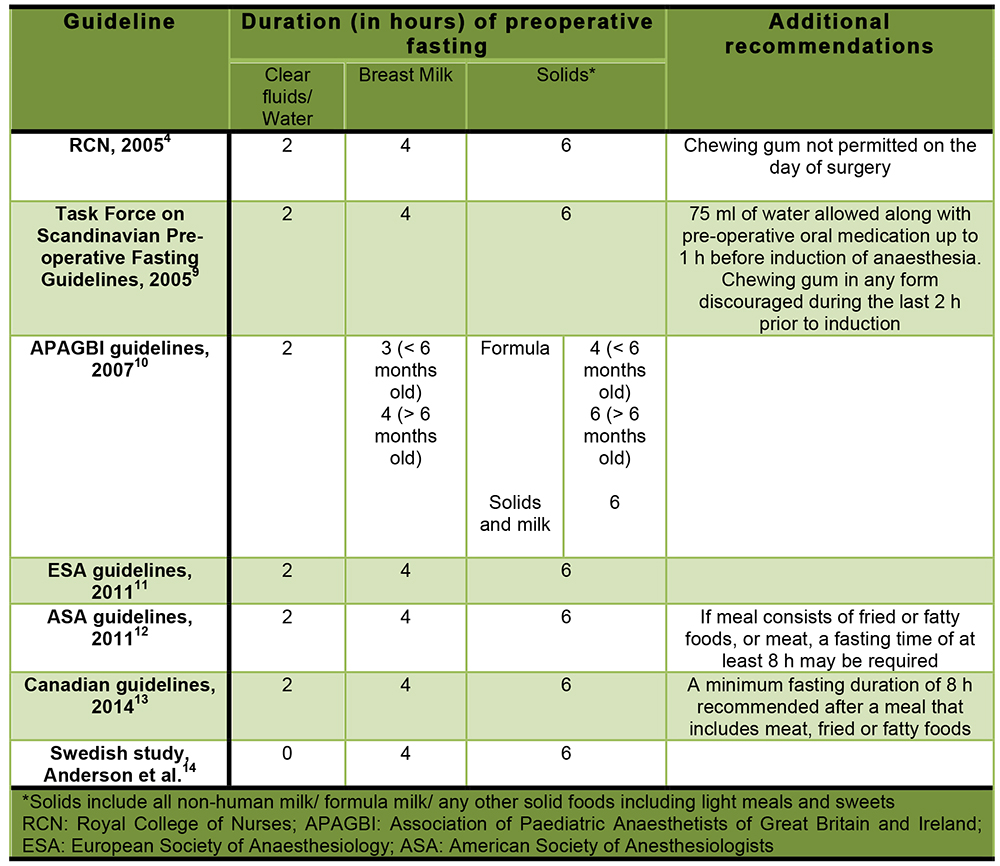
Table 1: Summary of recommendations on paediatric preoperative fasting
NEW EVIDENCE
In a recent Swedish study, Anderson et al. demonstrated that children could be allowed to consume fluids until taken to the operating area, and this practice did not increase the risk of pulmonary aspiration. Elective paediatric procedures from 2008-2013 were assessed retrospectively. In over 10,000 anaesthetic cases, only three patients had any evidence of pulmonary aspiration. Further, none of the cases required cancellation of the surgery, ventilator support or admission to intensive care. The authors recommend a 0-4-6 regimen instead of 2-4-6 regimen for preoperative fasting in the paediatric age group13. The authors suggested that the advantages of such a practice are14-15:
- A contented child no longer at risk of dehydration or hypoglycaemia
- Improved patient cooperation and compliance
- An eliminated need to precisely manage fasting durations due to a frequently changing operating schedule, which is overcome by allowing the child to consume fluids until time of surgery
INCONSISTENCIES IN CURRENT PRACTICE
Although various societies have published guidelines on preoperative fasting, clinical adoption is slow3. In a survey by Emerson, only about 75% of paediatric anaesthetists allowed children to drink clear fluids up to two hours preoperatively. While with respect to breast milk, formula and other solid feeds, the practice patterns were even more varied16. Sometimes, anaesthetists permitted consumption of milk closer to the time of surgery than the guideline recommendation17. These observations show a lack of uniformity regarding the preoperative fasting practices. In reality, children are frequently fasted far in excess of the recommendations.
SUMMARY
Challenges in practice can be overcome by developing local policies based on published evidence and consensus opinion of the local anaesthetists and ward nurses. An evidence-based and patient-centric approach is important, with periodic audits to highlight any inconsistencies. The 0-4-6 regimen could be a promising approach to preoperative fasting in routine paediatric anaesthetic practice, but requires local audit to ensure that there are no unexpected consequences of introducing a more liberal approach to starvation.
ANSWERS TO QUESTIONS
- Food consumption in healthy subjects undergoing elective surgery increases the risk of pulmonary aspiration by:
a. True
b. True
c. False: Increase in gastric emptying decreases the gastric volume and reduces the risk of pulmonary aspiration
d. True
e. True - Advantages of reduced duration of fasting are:
a. True
b. True
c. True
d. True
e. True - Clear fluids include:
a. True
b. True
c. True
d. False: Milk, an emulsion, behaves more like a solid after consumption, by forming curds in the stomach
e. True
REFERENCES AND FURTHER READING
- Hamid S. Pre-operative fasting- a patient centered approach.BMJ Qual Improv Report. 2014; 2.
- Brady MC, Kinn S, Ness V, O’Rourke K, Randhawa N, Stuart P. Preoperative fasting for preventing perioperative complications in children. Cochrane Database of Systematic Reviews 2009, Issue 4. Art. No.: CD005285. DOI: 10.1002/14651858.CD005285.pub2.
- Arun BG, Korula G. Preoperative fasting in children: An audit and its implications in a tertiary care hospital. J Anaesthesiol Clin Pharmacol. 2013;29:88-91.
- Perioperative fasting in adults and children. An RCN guideline for the multidisciplinary team. 2005.
- Andersson H, Zaren B, Frykholm P. Low incidence of pulmonary aspiration in children allowed intake of clear fluids until called to operating suite. Pediatric Anesthesia . 2015;25(8): 770-777.
- Levy DM. Pre-operative fasting—60 years on from Mendelson. Contin Educ Anaesth Crit Care Pain. 2006;6(6):215-218.
- Meurling S. Paediatric aspects: no fasting in children? Scand J Nutr. 2004;48(2):83.
- Crowley M. Preoperative fasting guidelines. 2015. Available at: http://www.uptodate.com/contents/preoperativefasting- guidelines. Accessed on October 28, 2015.
- Søreide E, Eriksson LI, Hirlekar G, Eriksson H, Henneberg SW, Sandin R, Raeder J; (Task Force on Scandinavian Pre-operative Fasting Guidelines, Clinical Practice Committee Scandinavian Society of Anaesthesiology and Intensive Care Medicine). Pre-operative fasting guidelines: an update. Acta Anaesthesiol Scand. 2005 Sep;49(8):1041-7.
- APA consensus guideline on perioperative fluid management in children: V 1.1 September 2007.
- Smith I, Kranke P, Murat I, Smith A, O’Sullivan G, Søreide E, Spies C, in’t Veld B; European Society of Anaesthesiology. Perioperative fasting in adults and children: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol. 2011 Aug;28(8):556-69.
- An Updated Report by the American Society of Anesthesiologists Committee on Standards and Practice Parameters: Practice Guidelines for Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration: Application to Healthy Patients Undergoing Elective Procedures. Anesthesiology. 2011;114(3):495-511.
- Merchant R, Chartrand D, Dain S, et al. Guidelines to the Practice of Anesthesia–Revised Edition 2014. Can J Anaesth 2014; 61:46-71.
- Anderson H, Zaren B, Frykholm P. low incidence of pulmonary aspiration in children allowed intake of clear fluids until called to the operating suite. Paediatr Anaesth. 2015 Aug;25(8):770-7.
- Ragg P. Let them drink! Paediatr aanesth. 2015 Aug;25(8):762-3.doi: 1111/pan.12710
- Emerson BM, Wrigley SR, Newton M. Pre-operative fasting for paediatric anaesthesia. A survey of current practice. Anaesthesia 1998;53(4):326-30.
- Hofer C, Tucci M, van Gessel E, Alon E, Zollinger A. Is traditional preoperative fasting policy changing? Results of a Swiss survey on current practice. European Society of Anaesthetists Proceedings. 2001:8-9 (A30).



