Basic Sciences
The WFSA has been working on information about pulse oximery and the following tutorial is part of the material. Feedback would be very useful and should be sent to iain.wilson@rdeft.nhs.uk
The first part of this tutorial (last week) can be found at www.anaesthesiologists.org under educational resources.
PULSE OXIMETER QUIZ 3
The causes of hypoxia during anaesthesia can be attributed to problems in the Airway, Breathing, Circulation, Drugs and Equipment. By remembering to check the patient in this order, most of the problems causing hypoxia can be identified and treated.
Using the headings below, consider what could go wrong during anaesthesia to cause hypoxia. Compare your answers to the table on the next page.
Airway
Breathing
Circulation
Drugs
Equipment
What do you think is the most common cause of hypoxia in theatre or recovery?
CAUSES OF HYPOXIA DURING ANAESTHESIA
The causes of hypoxia during anaesthesia are summarised in table 1. Airway obstruction is the most common cause of hypoxia.
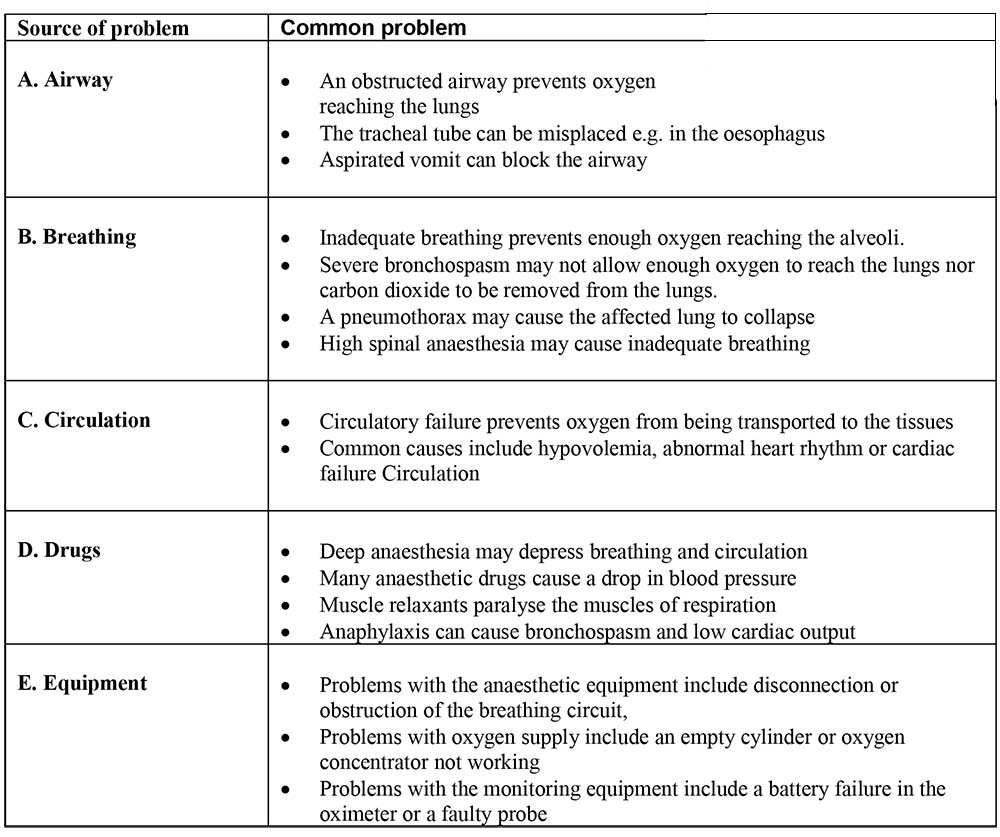
Table 1. Causes of hypoxia in theatre – ‘ABCDE’
Learning point: When hypoxia occurs, it is essential to decide whether the problem is with the patient or the equipment. After a quick check of the common patient problems, make sure the equipment is working.
What should be done when the saturation falls?
During anaesthesia, low oxygen saturations must be treated immediately and appropriately. The patient may become hypoxic at any time during induction, maintenance or emergence from anaesthesia. The appropriate response is to administer 100% oxygen, make sure that ventilation is adequate by using hand ventilation and then correct the factor that is causing the patient to become hypoxic. For example, if the patient has an obstructed airway and is unable to breathe oxygen into the lungs, the problem will only be cured when the airway is cleared.
Whenever the patient has low saturations, administer high flow oxygen and consider ‘ABCDE’:
- A – airway clear?
- B – breathing adequately?
- C – circulation working normally?
- D – drugs causing a problem?
- E – equipment working properly?
You must respond to hypoxia immediately by giving more oxygen, ensuring adequate ventilation by hand, calling for help, and running through the ‘ABCDE’ sequence. Treat each element of the sequence as you check it. After you have been through all the checks for the first time, go back and recheck them until you are satisfied that the patient’s condition has improved. WHO has put this into an algorithm or chart (below) to help you remember what to look for in a logical sequence. In an emergency, there may not be time to read what to do. You should ask a colleague to read through the chart for you to make sure that you have not forgotten anything.
Learning point: If SpO2 is 94% or below, give 100% oxygen, hand ventilate, consider ABCDE
ALGORITHM FOR SPO2 < 94%
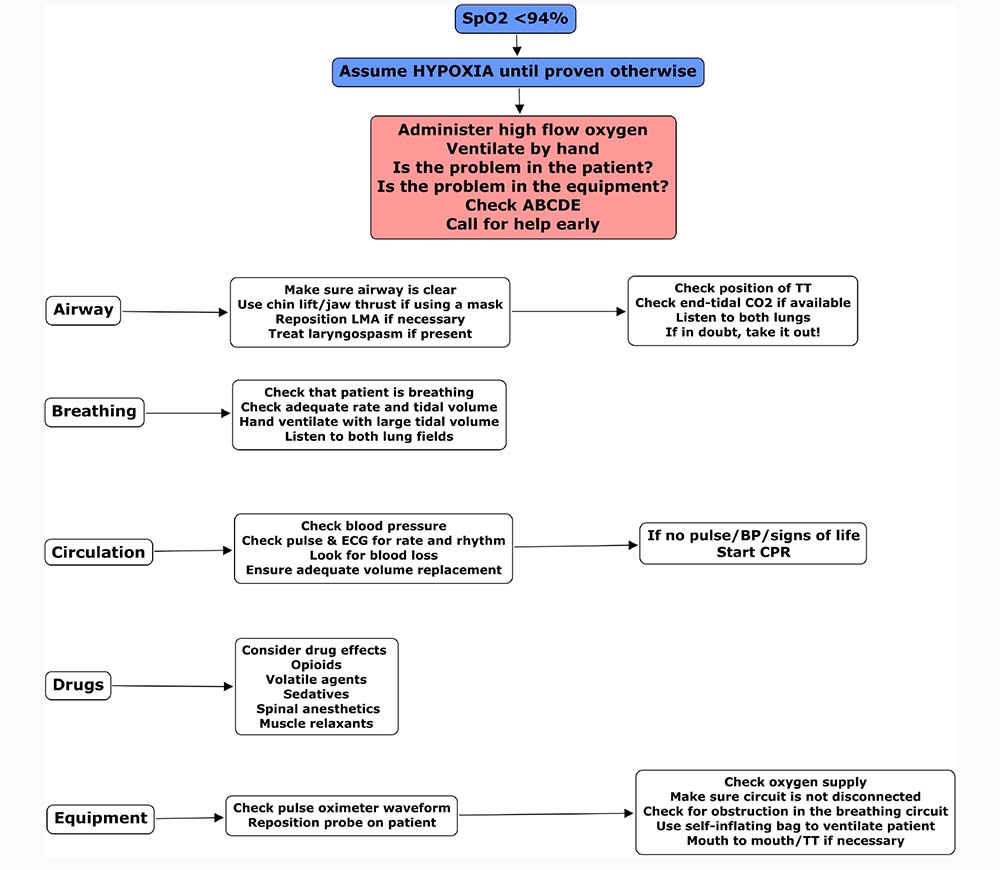
Actions To Take If The Oxygen Saturation Is 94% Or Below
If the oxygen saturation is 94% or below, you should administer 100% oxygen, ventilate by hand, consider whether the problem is with the patient or the equipment, then move through the algorithm ‘ABCDE’, assessing each factor and correcting it immediately as you go.
Oxygen
Administer high flow oxygen if SpO2 is ≤94%
A – Is the airway clear?
- Is the patient breathing quietly without signs of obstruction?
- Are there signs of laryngospasm? (mild laryngospasm – high pitched inspiratory noise; severe laryngospasm – silent, no gas passes between the vocal cords)
- Is there any vomit or blood in the airway?
- Is the tracheal tube in the right place?
Action
- Ensure that there is no obstruction.
- If breathing via a facemask – chin lift, jaw thrust
- Consider an oropharyngeal or nasopharyngeal airway
- Check for laryngospasm and treat if necessary
- Check the tracheal tube/LMA – if any doubt about the position, remove and use a facemask.
- If breathing via a facemask – chin lift, jaw thrust
- Suction the airway to clear secretions.
- Consider waking the patient up if you have difficulty maintaining the airway immediately after induction of anaesthesia.
- Consider intubation.
- If you ‘can’t intubate, can’t ventilate’, an emergency surgical airway is required.
Airway obstruction is the most common cause of hypoxia in theatre. Airway obstruction is a clinical diagnosis and must be acted upon swiftly. Unrecognised inadvertent oesophageal intubation is a major cause of anaesthesia morbidity and mortality. An intubated patient who has been previously well saturated may become hypoxic if the tracheal tube becomes displaced, kinked or obstructed by secretions. Check the endotracheal tube and – ‘If in doubt, take it out’
B – Is the patient breathing adequately?
Look, listen and feel:
- Are the chest movement and tidal volume adequate?
- Listen to both lungs – is there normal bilateral air entry? Are the breath sounds normal? Any wheeze or added sounds?
- Is the chest movement symmetrical?
- Is anaesthesia causing respiratory depression?
- Is a high spinal causing respiratory distress?
Bronchospasm, lung consolidation/collapse, lung trauma, pulmonary oedema or pneumothorax may prevent oxygen getting into the alveoli to combine with haemoglobin. Drugs such as opioids, poorly reversed neuromuscular blocking agents or deep volatile anaesthesia may depress breathing. A high spinal anaesthetic may paralyse the muscles of respiration. In an infant, stomach distension from facemask ventilation may splint the diaphragm and interfere with breathing. The treatment should deal with the specific problem.
Action
- Assist ventilation with good tidal volumes to expand both lungs until the problem is diagnosed and treated appropriately.
- If there is sufficient time, consider a chest X-ray to aid diagnosis.
The patient should be ventilated via a facemask, LMA or tracheal tube if the respiration is inadequate. This will rapidly reverse hypoventilation due to drugs or a high spinal and a collapsed lung will re-expand. The lower airway should be suctioned with suction catheters to remove any secretions. A nasogastric tube should be passed to relieve stomach distension.
A pneumothorax may occur following trauma, central line insertion or a supraclavicular brachial plexus block. It may be suspected if there is reduced air entry on the affected side. In thin patients a hollow note on percussion may also be detected. A chest X-ray is diagnostic. A chest drain should be inserted as the pneumothorax may worsen. When there is associated hypotension (tension pneumothorax), the pneumothorax should be treated by emergency needle decompression through the 2nd intercostal space in the mid-clavicular line without waiting for an X-ray. A definitive chest drain should be inserted later. Always maintain a high index of suspicion in trauma cases.
C – Is the circulation normal?
- Feel for a pulse and look for signs of life, including active bleeding from the surgical wound
- Check the blood pressure
- Check the peripheral perfusion and capillary refill time.
- Observe for signs of excessive blood loss in the suction bottles or wound swabs
- Is anaesthesia too deep? Is there a high spinal block?
- Is venous return impaired by compression of the vena cava (gravid uterus, surgical compression)
- Is the patient in septic or cardiac shock?
Normally an inadequate circulation is revealed by the pulse oximeter as a loss or reduction of pulsatile waveform or difficulty getting a pulse signal.
Action
- If the blood pressure is low, correct it
- Check for hypovolaemia
- Give IV fluids as appropriate (normal saline or blood as indicated)
- Consider head down or leg up position, or in the pregnant mother, left lateral displacement.
- Consider a vasoconstrictor such as ephedrine or phenylephrine
- If the patient has suffered a cardiac arrest, commence cardiopulmonary resuscitation (CPR) and consider reversible causes (4 H’s, 4T’s: Hypotension, Hypovolaemia, Hypoxia, Hypothermia; Tension pneumothorax, Tamponade (cardiac), Toxic effects (deep anaesthesia, sepsis, drugs), Thromboemboli (pulmonary embolism)
D – Drug effects
Check that all anaesthesia drugs are being given correctly.
- Excessive halothane (or other volatile agent) causes cardiac depression.
- Muscle relaxants will depress the ability to breathe if not reversed adequately at the end of surgery.
- Opioids and other sedatives may depress breathing.
- Anaphylaxis causes cardiovascular collapse, often with bronchospasm and skin flushing (rash). This may occur if the patient is given a drug, blood or artificial colloid solution that they are allergic to. Some patients are allergic to latex rubber.
Action
- Look for an adverse drug effect.
- In anaphylaxis, stop administering the causative agent, administer 100% oxygen, give intravenous saline starting with a bolus of 10ml/kg, administer adrenaline and consider giving steroids, bronchodilators and an antihistamine.
E – Is the equipment working properly?
- Is there a problem with the oxygen delivery system to the patient?
- Does the oximeter show an adequate pulse signal?
Action
- Check for obstruction or disconnection of the breathing circuit or tracheal tube.
- Check that the oxygen cylinder is not empty
- Check that the oxygen concentrator is working properly
- Check that the central hospital oxygen supply is working properly
- Change the probe to another site; check that it is working properly by trying it on your own finger.
If it is felt that the anaesthesia equipment is faulty, use a self-inflating bag to ventilate the patient with air while new equipment or oxygen supplies are obtained. If equipment is missing, mouth to tracheal tube, or mouth-to-mouth ventilation, may be lifesaving.
Clinical scenario workshop
Work through problems in each case, deciding why the SpO2 is low (ABCDE) and what the most appropriate action should be. The first three scenarios are explained in detail. The others should be discussed with your colleagues.
1. A 12-year-old child is scheduled for elective anaesthesia for foot surgery. The patient is ASA 1 and is induced with thiopentone then given halothane in air and oxygen via a face mask. During the induction the patient starts to cough and gets laryngospasm. The SpO2, which started at 98%, falls to 88% during coughing and then to 74% when laryngospasm occurs. Discuss why the saturation has fallen and what would be the most appropriate actions?
- Give 100% oxygen, assess ABCDE
- A – airway obstruction due to laryngospasm; apply positive pressure to the reservoir bag, deepen anaesthesia. If the situation does not resolve, a small dose of suxamethonium (0.5mg/kg) should be given.
- B – breathing improves after resolution of laryngospasm
- C – assess pulse rate – bradycardia may occur due to hypoxia or secondary to suxamethonium. Consider atropine after treating hypoxia.
- D – check the halothane has not run out
- E – check that the anaesthesia equipment is functioning and connected appropriately.
After treating the laryngospasm, the patient improved and the SpO2 returned to normal.
2. A 56-year-old obese patient is undergoing a laparotomy for bowel obstruction. Preoperatively he is reasonably fit and his SpO2 is 95%. After rapid sequence induction and intubation, the patient is ventilated and anaesthesia maintained using halothane in air with 30% oxygen. Over the next 10 minutes the patient’s SpO2 falls to 85%. What are the most likely causes and what action would you take?
- Give 100% oxygen, check ABCDE
- A – check the airway and position of the tracheal tube. Check there is equal air entry to both sides of the chest and that the tube is not kinked. Check that there is no vomit in the mouth to suggest that the patient may have aspirated.
- B – check that there are no added breath sounds to suggest aspiration, lung collapse or bronchospasm. Give large tidal volumes by hand and listed to the chest. Is ventilation easy?
- C – assess whether the circulation is normal
- D – assess whether the patient is fully relaxed. Check that there are no signs to suggest drug reaction (particularly wheeze + hypotension + rash)
- E – check that the anaesthesia equipment is functioning and connected appropriately
After ventilating the patient with some large tidal volumes and increasing the inspired oxygen the patient improved. The problem was lung collapse.
3. During a Caesarean section under spinal anaesthesia, a fit 23-year-old primigravida complains of tingling in the fingers and difficulty breathing. The SpO2 falls from 97% to 88%. What are the most likely causes and what action would you take?
- Give 100% oxygen. Check ABCDE
- A – check that the airway is clear
- B – assess breathing. A high spinal may paralyse the muscles of respiration. If breathing is inadequate, ventilate the patient and induce anaesthesia and intubate. Ventilate until the block wears off.
- C – check the blood pressure – hypotension is likely. Treat with left lateral tilt, IV fluids and vasopressors.
- D – check the height of the block. Look for signs of a very high block – difficulty breathing, whispering rather than talking, weak arms and numbness on the shoulders. All indicate the nerves to the diaphragm are becoming blocked. This will make it impossible for the patient to breathe. If the block is not this high, the patient can talk in a normal voice and move their arms normally, but breathing still feels difficult due to the intercostal paralysis, normally the patient can breathe safely using their diaphragm.
- E – always ensure that equipment is ready in case this complication occurs
After giving oxygen, the anaesthetist determined the block was not too high and the patient settled with reassurance. The SpO2 improved with oxygen. Any hypoxia in a pregnant patient is dangerous for the baby.
Discuss the following cases with your colleagues:
- In recovery, following a soft tissue knee operation under face-mask anaesthesia, a 43 year old patient is reported to have a SpO2 of 77%. What are the possible causes and what action would you take?
- In recovery, following a laparotomy under relaxant anaesthesia, a 43-year-old patient is reported to have a SpO2 of 77% and is making twitching, jerky movements. What are the most likely causes and what action would you take?
- Following a road traffic accident 3 days previously, a patient with 5 fractured ribs is found to have an SpO2 of 83%. He is not receiving oxygen, but is in a great deal of pain. What are the most likely causes and what action would you take?
- In a patient undergoing splenectomy following an accident, the pulse oximeter which was showing a pulse rate of 120 beats / min and an SpO2 of 94%, stops reading and alarms. What are the most likely causes and what action would you take?
- A 10-month-old child is having a halothane induction for a laparotomy for intussusception. The child was extremely unwell prior to anaesthesia. During induction the heart rate drops from 190 beats/min to 60 beats / minute. Over the next 30 seconds the heart rate continues to slow. The SpO2 is 98%. You then notice that there is no waveform or reading from the oximeter.
Discussion points which should have been considered:
1. ABCDE, oxygen, effects of anaesthesia drugs in recovery period, positioning, drugs, aspiration.
2. In addition to above – role of muscle relaxants and reversal.
3. Pain, ineffective breathing and coughing, lung contusion and collapse, analgesia.
4 & 5. Hypovolaemia, preoperative preparation, poor signal, cool peripheries, need for resuscitation, possible cardiac arrest due to hypovolaemia, halothane causing circulatory depression, signs of shock in children.



