Basic Sciences
QUESTIONS
Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation.
- Lung measurements:
- Fowlers method measures physiological dead space
- TLC can be measured using a spirometer
- the FRC in an average adult is 2.2litre
- vital capacity is the volume of air expired from full inspiration to full expiration
- helium dilution over estimates FRC in patients’ with bullous lung disease
- The functional residual capacity:
- is increased in the obese
- is the residual volume plus the inspiratory reserve volume
- falls with general anaesthesia
- is not affected by posture
- falls with increasing age
- Surfactant:
- is a mucopolypeptide
- causes a decrease in surface tension
- keeps alveoli dry
- causes an increase in compliance
- production is reduced after a prolonged reduction in pulmonary blood flow
- A pressure-volume curve can be used for measuring:
- the work of breathing
- functional residual capacity
- anatomical dead space
- compliance
- respiratory quotient
FUNCTIONAL ANATOMY
To maintain gas exchange function, the anatomy of the respiratory system is designed in such a way to make the process as efficient as possible.
The nose, mouth and pharynx conduct air to the larynx, humidify and filter the air gases. The larynx aids phonation and conducts the gas into the trachea which in an adult is about 18mm in diameter and 11 cm in length. It is lined with columnar ciliated epithelium and divides into the left and right major bronchi at the carina (T4). The bronchi divide 23 times in total (23 generations) in order to increase the surface area available for gas exchange.
The first 16 generations are termed the conducting zone, no bronchi in his region take part in gas exchange and this forms the anatomical dead space. In an average adult the volume of this space is about 150ml.
From generation 17 onwards, small alveoli bud off the bronchi, these are where gas exchange takes place. Generation 17 -23 is the respiratory zone where gas exchange occurs. The volume of this zone is about 2-3 litres and there are about 300 million alveoli present within an average lung.
Cells types and functions in the lung
Type 1 alveolar cells
- These cells are derived from type II alveolar cells and provide a thin layer of cytoplasm which covers about 80% of the gas exchange zone
Type II alveolar cells
- These cells allow the formation of surfactant and other enzymes
Type III alveolar cells
- These cells are the main lung defence system – they are the alveolar macrophages
Surfactant
Surfactant is stored in the lamellar bodies of type II alveolar cells and made up of a mixture of phospholipids, plasma proteins and carbohydrate. It is an amphipathic molecule – with a charged hydrophilic head and hydrophobic tail. Functions of surfactant are:
- Surfactant reduces surface tension within the alveoli which helps to increase the compliance of the lung
- It improves alveolar stability
- It keeps alveoli dry by opposing water movement from the pulmonary interstitium
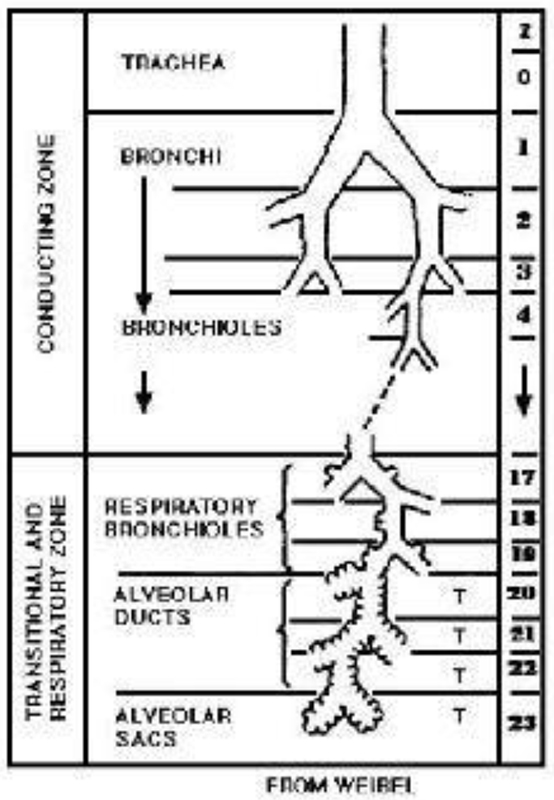
Figure 1: Weibels classification of the airways – Generations 1 – 23
LUNG VOLUMES
There are many lung volumes which can be measured and used to give information about diagnosis and progression of disease processes as well as a guide to patients’ respiratory reserve.
Most volumes are measured using basic spirometry at B,T,P,S (Body Temperature and Standard Pressure) using a Wright’s Respirometer.
Key points
- The conducting zone begins at the mouth and continues until the 16th generation. This zone transports gas but plays no part in gas exchange.
- The respiratory zone continues from the 17th until the 23rd generation and is the region where gas exchange occurs.
Clinical Points
- The ETT in an adult should lie 1-2cm superior to the carina
- On an X-ray the carina is the point at which the trachea can be seen dividing into the right and left bronchi – around T4
- The right major bronchus divides from the trachea at a much less acute angle than the left making it more prone to endobronchial intubation
- The right upper lobe bronchus arises only a few centimeters from the carina therefore for one lung ventilation a left sided double lumen tube is favoured to avoid the risks of right upper lobe collapse with a right sided double lumen tube
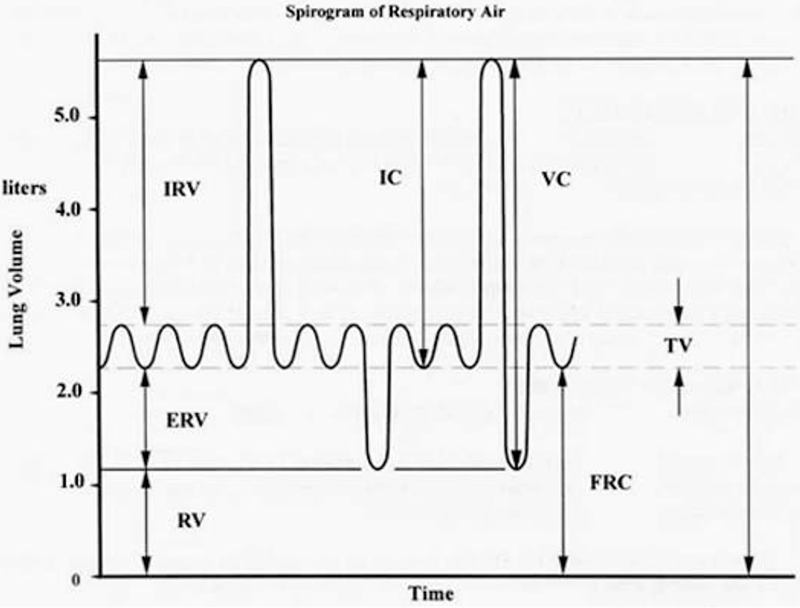
Figure 2: Basic spirometry trace of lung volumes and capacities
Lung volumes vary with age, sex, height and weight, and are formulated into nomograms.
- Residual volume RV – Volume of gas remaining in lungs after a forced expiration (15-20ml/kg)
- Expiratory reserve volume ERV – Volume of gas forcefully expired after normal tidal expiration (15ml/kg)
- Tidal volume TV – Volume of gas inspired and expired during normal breathing (6ml/kg)
- Inspiratory reserve volume IRV – Volume of gas inspired over normal tidal inspiration (45ml/kg)
Any 2 or more volumes added together = a capacity
- Total lung capacity – volume of gas in lungs at the end of maximal inspiration (80ml/kg)
- Vital Capacity – sum of IRV, TV and ERV (60-70ml/kg)
- Functional residual capacity – Sum of ERV and RV (30ml/kg)
Functional Residual capacity
FRC = ERV + RV
The FRC is the balance between the tendency of the chest wall to spring outwards and the tendency of the lung to collapse. FRC is not the same volume all the time; it can be disrupted by many factors
Factors decreasing FRC
- Age
- Posture – supine position
- Anaesthesia – muscle relaxants
- Surgery – Laparoscopic
- Pulmonary fibrosis
- Pulmonary oedema
- Obesity
- Abdominal Swelling
- Reduced muscle tone – Reduced diaphragm tone will reduce pull away from the lungs
- Pregnancy – Increased abdominal pressure
Factors increasing FRC
- Increasing height of patient
- Erect position – diaphragm and abdominal organs less able to encroach upon bases of the lungs
- Emphysema – decreased elastic recoil of lung therefore less tendency of lung to collapse
- Asthma – air trapping
Measurement of FRC
A spirometer is unable to measure TLC, FRC and RV.
There are 2 methods are used to measure FRC:
1. Helium dilution
The patient is connected to a spirometer containing a known volume of gas (V1) with a known concentration of helium (C1)
Helium is not metabolised by the body.
The patient begins to breathe normally. The helium concentration will change as the helium gets diluted in a larger volume of gas due to the patient’s lung volume. (V1 + FRC)
The final helium concentration is measured.
The value for FRC can then be derived since 3 of the 4 values are known.
C1 X V1 = C2 x (V1 +V2)
V2 = V1 (C1-C2)/C2
This method measures the volume of gas in the lungs which is participating in gas exchange. It will underestimate the FRC if there are significant areas of gas trapping.
2. Body Plethysmography
FRC is measured by placing the patient in a closed chamber and measuring the pressure and volume changes occurring when the subject makes an inspiratory effort against a closed airway. Boyle’s gas law (P1V1=P2V2) is applied as ventilation takes place to derive the FRC.
This technique also takes into account any gas trapped behind closed airways e.g. in the case of patients with emphysematous bullae. Helium dilution techniques do not calculate this.
Closing capacity (CC)
This is the volume at which the small airways close during expiration. Under normal circumstances the FRC is always greater than the CC however if the FRC was to decrease then this would no longer be the case and the small airways may close at the end of normal tidal expiration. This leads to hypoxaemia, atelectasis and worsening gas exchange due to increasing V/Q mismatch.
Closing capacity increases with age. Typically closing capacity is equal to FRC at the age of 66 in the erect position or 44 in the supine position.
Preoxygenation
The major oxygen store within the body is the Functional Residual Capacity. A typical volume for FRC is about 2.2 litres in an average adult and normally contains 21% oxygen. Since total body oxygen consumption is about 250mls per minute this normal store of oxygen will only last just over 1 minute with apnoea. Preoxygenation is defined as breathing 100% oxygen from a close fitting mask for 3-5 minutes. Breathing 100% oxygen for this time will denitrogenate the lungs and increases the oxygen store to in excess of 1800mls thus increasing the time to desaturation to about 7-8 minutes assuming an oxygen consumption of 250mls/min.
Key points
- Spirometry can be used to provide values for all basic lung volumes except TLC, RV and FRC
- FRC is determined by the balance between lung collapse and chest wall springing outward
- FRC affects oxygenation
- FRC is the main oxygen store in the body and can be easily and quickly enriched with oxygen
- FRC will change due to a large number of factors
Clinical points
- The FRC is reduced by anaesthesia and therefore hypoxia is common in a patient with a decrease in FRC. The application of PEEP enables the FRC to remain greater then CC and improves oxygenation
- PEEP maintains the lungs on the steep part of the compliance curve which lessens collapse at the bases of the lungs.
- Preoxygenation should take place for 3-5 minutes or 4 vital capacity breaths
- Preoxygenation is essential in patients likely to have a decreased FRC e.g. pregnant, obese
- Adequacy of preoxygenation can be assessed by monitoring end tidal oxygen – aim for ETO2 > 90%
VENTILATION
Total ventilation (MV) = VT x RR
With each tidal volume about a third the total amount of gas flowing into the airway and lung does not participate in gas exchange. This is the physiological dead space.
What is dead space?
Dead space can be defined as a volume of gas which does not take part in gas exchange.
Dead space can be classified into 3 types
- Anatomical dead space
- This includes any breathing system or airway plus mouth, trachea and the airways up until the start of the respiratory zone. The typical volume in an adult is about 150mls (See section 1)
- Alveolar dead space
- This occurs when areas of the lung are being ventilated but not being perfused and this leads to what is known as V/Q mismatch.
- Large increases in alveolar dead space commonly occur in the following conditions: pneumonia, pulmonary oedema, pulmonary embolism
- Physiological dead space
- This is a combination of alveolar and anatomical dead space added together.
Dead space is usually 30% of VT
Measurement of dead space
Fowlers method
This is used to measure anatomical dead space.
A patient takes a breath of 100% oxygen to rid the conducting zone gases of nitrogen and then exhales through a mouthpiece capable of analysing nitrogen concentration at the lips.
Initially the exhaled gases contain no nitrogen as this is dead space gas; the nitrogen concentration will increase as the alveolar gases are exhaled. Nitrogen which is measured following the breath of 100% oxygen must then have come only from gas exchanging areas of the lung and not dead space.
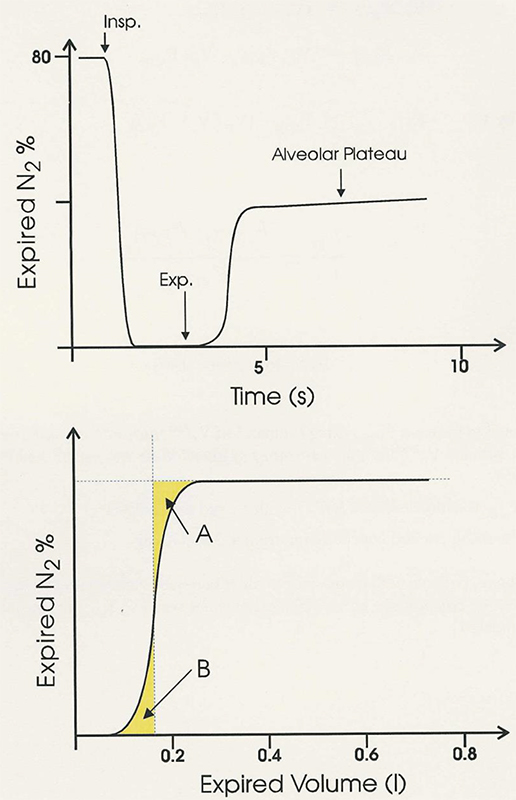
Figure 3: Fowlers method. Initially expired nitrogen concentration is plotted against time as seen intop graph. To calculate the anatomical dead space expired nitrogen is plotted against volume. The upstroke of the curve is equally divided in half to give areas A and B. The anatomical dead space equals volume 0 up to and including area B.
The Bohr Equation
This measures physiological dead space. It is a complicated equation is based upon the fact that all CO2 comes from alveolar gas and the exhalation of CO2 can therefore be used to measure gas exchange or lack of gas exchange if there is alveolar dead space (no perfusion of these alveoli).
For each tidal volume there will be a proportion of dead space (anatomical) but the amount of gas that is left over should take part in gas exchange. In order to derive the equation:
- FACO2- Alveolar CO2
- FeCO2-CO2 from mixed expired gases
- VT- Tidal volume
- VD- Dead space volume (Physiological)
In an adult with normal lungs the value for VD/VT is between 0.20 and 0.35
The expiration of CO2 is calculated by either
VTCO2 = VA x FACO2
or
VTCO2 = VT x FeCO2
As we said above though with each breath there will be a component of dead space, therefore:
VA = VT – VD
Therefore:
(VT – VD) x FACO2 = VT x FeCO2
This can be expressed as:
VD/VT = (FACO2 – FeCO2)/FACO2
There is not really a truly ideal value for FACO2 that can be used in the equation and therefore arterial pCO2 is used. This is substituted into the equation giving:
VD/VT = (PaCO2 – PeCO2)/PaCO2
Key points
- Approximately 1/3 of VT is dead space
- There are 3 types of dead space: Anatomical, Physiological and Alveolar
- Physiological dead space is a combination of alveolar and anatomical dead space
- Anatomical dead space is about 150mls in an average adult and is measured by fowlers method
- Physiological dead space is measured using the Bohr equation
Clinical points
- Minimise dead space by using the correct sized equipment e.g HME, breathing circuits Consider the application of PEEP to prevent atelectasis and V/Q mismatch
RESPIRATORY MECHANICS
Respiratory muscles
Inspiratory muscles
- Diaphragm – very powerful, has the ability to contact 10cm in forced inspiration
- External intercostals – pull the ribs up and forwards
- Accessory inspiratory muscles – scalene muscles (elevate first 2 ribs) and sternomastoids (raise the sternum)
- Muscles of neck and head (seen in small babies in respiratory distress)
Expiratory muscles
Expiration is usually passive and relies on the elastic recoil of the lungs and the chest wall. Under anaesthesia or extreme exercise expiration may become active due to the activation of abdominal muscles. Muscles have their use in forced expiration.
- Abdominal wall muscles – rectus abdominus, internal and external oblique
- Internal intercostal muscles – pull ribs down and inwards
Compliance
Compliance is defined as the volume change per unit pressure change and is usually expressed in mls/cmH2O
Compliance = ∆V/∆P
It is classified into chest wall, lung or total lung compliance. (Distensibility)
Compliance can be measured by inserting an oesophageal probe into a co-operative patient, the patient inhales and exhales to a set volume. At each volume the intrapleural pressure is estimated using the oesophageal probe. A pressure volume curve can then be plotted.
If during the measurement process no gas flow occurs at each set volume then this is static compliance. (Gas flow ceases and equilibration occurs) If gas flow continues throughout measurement then this is dynamic compliance.
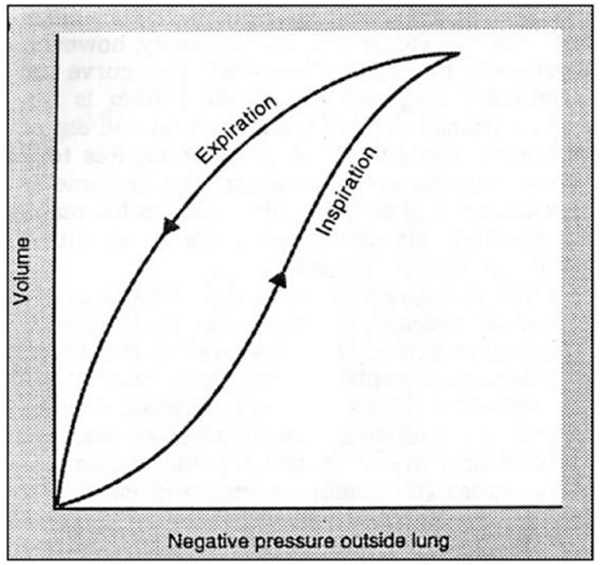
Figure 4: This graph illustrates lung compliance.
Using a spirometer certain fixed volumes can easily be measured e.g. TLC, RV and FRC.
The pressure along the x axis is often plotted as the transpulmonary pressure (Alveolar pressure – Intrapleural pressure)
Initially as can be seen from the above curve at lower lung volumes the compliance of the lung is poor and greater pressure change is required to cause a change in volume. This occurs if the lungs become collapsed for a period of time.
At FRC compliance is optimal since the elastic recoil of the lung towards collapse is balanced by the tendency of the chest wall to spring outwards.
At higher lung volumes the compliance of the lung again becomes less as the lung becomes stiffer.
Expiration is deemed a passive process due to the elastic recoil of the lung; because of this the inspiratory curve is not identical to the expiratory curve on a correctly drawn compliance curve. This is known as hysteresis.
Compliance increases in old age and emphysema as elastic lung tissue is destroyed. It is decreased in pulmonary fibrosis, pulmonary oedema, atelectasis and in the extremes of lung volume.
Work of breathing
The energy required for the work of breathing is mainly used in the process of inspiration as energy is required to overcome airway resistance, the elastic recoil of the tissues and the chest wall and tissue resistance.
The energy stored within the elastic tissues is used to provide for expiration.
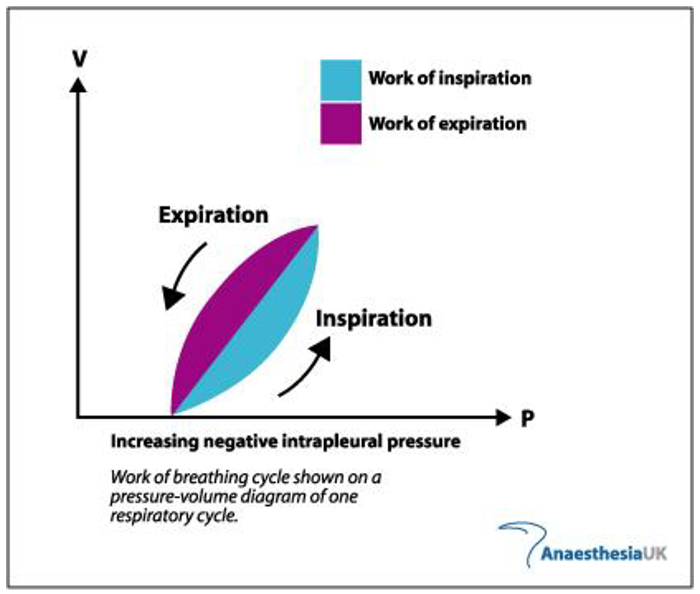
Figure 5: The work of breathing
Key Points
- Expiration is normally a passive process
- Compliance is the change in volume per unit change in pressure
- Compliance can be dynamic or static depending on whether the gas flow is continuing or allowed to equilibriate during pressure measurements
- A spirometer cannot measure TLC, FRC or RV
- Compliance of the lungs is poor at very low or very high lung volumes
- Compliance is optimal at or just above FRC
Clinical points
- Patients using their accessory muscles may indicate increased work of breathing
- PEEP can help to maintain the lungs at FRC
- If used correctly CPAP can reduce the work of breathing by increasing FRC
ANSWERS TO MCQS
- FFTTF
Fowlers method uses expired nitrogen concentration to measure anatomical dead space. TLC, RV and FRC are measured using either helium dilution or body plethysmography techniques. FRC is about 2.2 litres in an average adult. Vital capacity is the combination of inspiratory reserve volume, tidal volume and expiratory volume. Helium dilution will underestimate the FRC in patients with bullous lung disease - FFTFT
The FRC decreases in the obese population and in the supine position. It is also affected by age and sex. It is the combination of the residual volume plus the expiratory reserve Volume. - FTTTT
Surfactant is an amphipathic molecule, with a charged hydrophilic head and hydrophobic tail. It is a mucopolysaccharide. - TFFTF
See explanation in answer 1 for stems a and b. The respiratory quotient is the amount of CO2 produced/O2 consumed and is measured by indirect calorimetry using a respirometer.
WEB LINKS
- www.frca.co.uk
REFERENCES
- West J B, Respiratory Physiology The essentials
- Brandis K, The Physiology Viva
- Yentis S, Hirsch N, Smith G B, Anaesthesia and Intensive Care A-Z



