Intensive Care Medicine
SELF-ASSESSMENT QUESTIONS
Please attempt the following questions before reading the tutorial.
- Which of the following statements is correct?
- Rhabdomyolysis is caused by the breakdown of haemoglobin
- The diagnosis is confirmed by measuring urinary myoglobin levels
- Dark discolouration of the urine results from hypovolaemia
- Status epilepticus is a cause of rhabdomyolysis
- Which of the following condition is NOT a recognised cause of rhabdomyolyis?
- Paracetamol toxicity
- Tetanus
- Neuroleptic malignant syndrome
- Dermatomyositis
- Regarding the management of rhabdomyolysis, which statements is/are correct?
- After crush injury, treatment should be started in hospital when the patient is fully monitored
- Normal saline 0.9% is an acceptable crystalloid to use
- There is no requirement for arterial blood gas analysis in an asymptomatic patient
- A urine output of 1ml/kg/hr is adequate
INTRODUCTION
Rhabdomyolysis is the breakdown of striated muscle. There are many causes that all ultimately progress to myocyte necrosis and release of intracellular contents into the circulation. This can produce life-threatening complications including hyperkalaemia and acute kidney injury (AKI).
EPIDEMIOLOGY
In the ICU setting, the most common causes of rhabdomyolysis are muscular trauma and vascular obstruction.1 Rhabdomyolysis occurs in up to 85% of patients with traumatic injuries.2 Alcohol has been implicated in the development of rhabdomyolysis in up to 20% of cases.3 About a third of all patients with rhabdomyolysis will develop AKI and it is suggested that 5-25% of all AKI results from rhabdomyolysis.4 Patients with severe injuries that develop rhabdomyolysis-induced renal failure have a mortality of approximately 20% but is higher if multiple organ dysfunction is present.5
PATHOPHYSIOLOGY
Muscle necrosis is the end-point of rhabdomyolysis. It results from either direct injury of the sarcolemma (the skeletal muscle cell membrane) or from hypoxia causing ATP depletion and sodium-potassium pump failure. This leads to sodium influx and accumulation of free cytosolic ionized calcium as the cell attempts to restore electrochemical neutrality via the sodium-calcium exchange mechanism. High intracellular calcium activates calcium-dependent proteases and phospholipases causing toxic metabolite production and cell death. Potassium, phosphate, myoglobin, creatine kinase (CK), creatinine and nucleosides (which are metabolized to urate) leak into the circulation. The subsequent inflammation and oedema leads to fluid accumulation in affected muscles and intravascular volume depletion.6
CAUSES
Causes of rhabdomyolysis can be classified into traumatic and non-traumatic (table 1). The most common cause is direct trauma to the muscle, either from being crushed or from direct pressure e.g, patient lying on the floor for long periods of time and unable to get up.
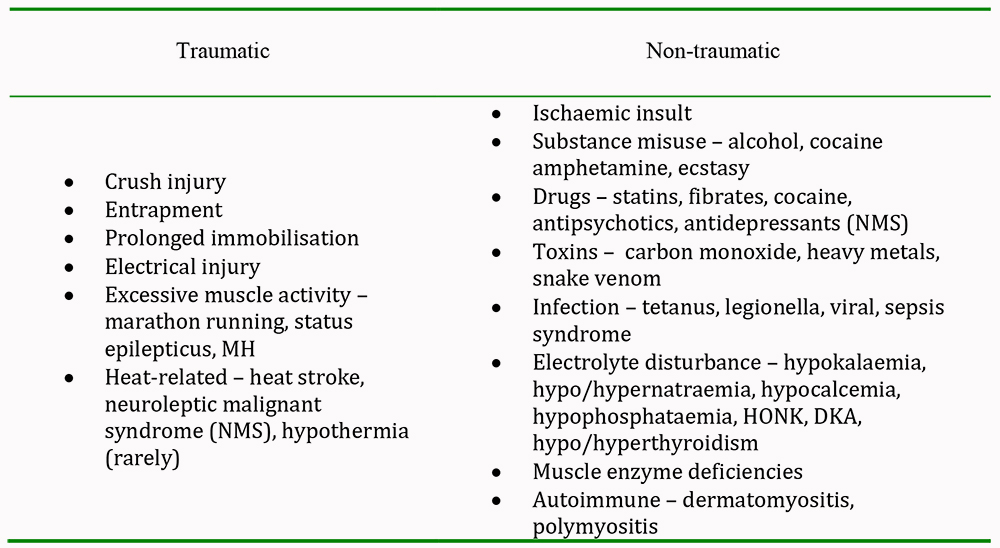
Table 1: Causes of rhabdomyolysis
PRESENTATION
Clinical Manifestations
The clinical presentation of rhabdomyolysis varies depending on the aetiology and severity. It may range from an asymptomatic rise in serum CK to hypovolaemic shock with life-threatening arrhythmias. Muscle pains and weakness are common and often associated with general malaise, nausea, tachycardia and confusion. Dark coloured urine may be the first indication of muscle damage. The ‘classic’ triad of symptoms includes muscle pains, weakness and dark urine but is seen in less than 10% of patients.5
Laboratory features
Biochemical markers confirm the diagnosis and can be used to predict prognosis. Serum CK levels are the most sensitive indicator of muscle damage, rising within the first twelve hours of injury, peaking at one to three days and declining at three to five days.5 A serum CK level over 5000u.litre-1 is related to renal failure and is associated with an incidence of AKI of over 50%.5 Levels are directly proportional to the extent of muscle injury. Compartment syndrome compounding the injury may further increase serum CK.7 Compartment syndrome occurs when increased pressure within a confined cavity within the body (commonly between fascial layers in the limbs) compromised the function of tissues, nerves and blood vessels.
Myoglobin is one of the significant compounds released after muscle disintegration. High circulating levels produce dark-brown discolouration of the urine as myoglobin is filtered by the kidney. Haematuria and myoglobinuria often co-exist, particularly in the context of trauma. The absence of myoglobinuria does not exclude the diagnosis of rhabdomyolysis so the clinical use is questionable.
Many metabolic derangements occur due to the rapid influx of calcium into cells. These include hyperkalaemia, hyperuricaemia, hyperphosphataemia, hypermagnesaemia and initially hypocalcaemia as calcium concentrates in myocytes. Hyperkalaemia is an early feature; electrolytes should be measured as soon as the diagnosis is made. High anion gap metabolic acidosis may develop in severe rhabdomyolysis due to lactic acid production in ischaemic muscles.
COMPLICATIONS
Early
Severe hyperkalaemia may lead to arrhythmias and cardiac arrest, especially in association with profound hypovolaemia, hypocalcaemia and acidosis.
Early or late
Compartment syndrome may develop and is exacerbated by the presence of hypotension. Compartment pressures greater than 30 mmHg are likely to cause significant muscle ischaemia and subsequent secondary rhabdomyolysis. Hepatic dysfunction occurs in approximately 25 % of individuals.4
Late
Disseminated intravascular coagulation may occur up to seventy-two hours following initial insult. Acute kidney injury is the most serious complication.8 The mechanism is not completely understood, but it thought to be due to a combination of renal vasoconstriction, hypovolaemia, mechanical obstruction by intraluminal cast formation and direct cytotoxicity.
During the recovery phase, hypercalcaemia may result from accumulation in muscle and from iatrogenic administration of calcium supplementation during periods of hypocalcaemia.7
MANAGEMENT
Early recognition and initiation of treatment is key to the stabilisation of life-threatening electrolyte disturbance and metabolic acidosis. Prompt aggressive fluid resuscitation with crystalloid is paramount and is the single most important factor in reducing the incidence of AKI. Alkalinisation of the urine with crystalloid resuscitation is considered standard. The use of bicarbonate and mannitol therapy is recognised however observational data suggest that they provide no additional clinical benefit to volume expansion with crystalloid.
Initial resuscitation
As soon as the diagnosis is confirmed, intravenous access should be established and baseline measurements including electrolytes and an arterial blood gas sample taken. Acute hyperkalaemia should be treated with standard therapy including insulin, dextrose and bicarbonate. As much as ten litres of fluid may be sequestrated into injured muscle. Intravenous crystalloid therapy with sodium chloride 0.9% should be started immediately. Fluid should be titrated to achieve a urine output of 200-300ml/hr. There is no good evidence to show that alkaline diuresis is superior to sodium chloride 0.9%.9 The administration of both sodium chloride 0.9% and isotonic sodium bicarbonate (1.26%) is an acceptable approach that can be used to avoid a worsening hyperchloraemic metabolic acidosis. Resuscitation should ideally be guided by the use of invasive monitoring. Intravenous mannitol can also be considered as it promotes renal renal blood flow and diuresis, although there is no evidence that this therapy leads to beneficial outcomes.
Rationale for bicarbonate and mannitol therapy
Alkalinisation of the urine is achieved by using 1.26% sodium bicarbonate of up to 500ml/hr, aiming for a urinary pH of greater than 6.5. This potentially prevents precipitation and degradation of myoglobin in the urinary tubules. It is also useful in the management of hyperkalaemia and acidosis however neither therapy has been subject to randomised clinical trials. Observational data suggest that the addition of mannitol and bicarbonate have no effect on the development of acute kidney injury, need for dialysis or death. If sodium bicarbonate is used, serum bicarbonate, calcium and potassium should be closely monitored.10
Compartment syndrome
Irreversible muscle and nerve damage can occur if there is a delay in the recognition and management of compartment syndrome. Neurovascular compromise implicates the need for fasciotomy. Intra-compartmental pressures consistently greater than 30mmHg despite reductive measures indicate a clear requirement for fasciotomy.
Renal replacement therapy
Established acute kidney injury or the presence of refractory hyperkalaemia and acidosis may necessitate renal replacement therapy (RRT). It is unusual for fluid overload to be an indication for RRT in rhabdomyolysis. Haemodialysis corrects metabolic and electrolyte disturbances rapidly and efficiently. The prognosis of renal failure secondary to rhabdomyolysis is good with renal function usually returning to normal within 3 months.10
SUMMARY
Rhabdomyolysis is often encountered in the intensive care setting. Patients may have few symptoms so a high level of suspicion should be maintained. Serum CK is the most sensitive indicator of muscle injury.
- Initiate fluid resuscitation immediately
- Treat acute hyperkalaemia
- Monitor for complications including compartment syndrome
- Serial CK measurement
- Renal replacement therapy may be required
ANSWERS TO QUESTIONS
- FFFT – a: rhabdomyolysis is due to striated muscle breakdown and myoglobin release; b: diagnosis is made on serum creatinine kinase levels; c: urine is discoloured by myoglobin; d: excessive muscle activity during seizures can cause muscle breakdown
- TFFF – a: paracetamol is not known to cause rhabdomyolysis however the rest are non-traumatic causes of muscle injury
- FTFF – a: fluid resuscitation should begin on scene if the patient is trapped to minimise the extent of acute kidney injury; b: saline is the fluid of choice however the patient should be monitored for the development of hyperchloraemic acidosis; c: arterial sampling establishes metabolic and electrolyte disturbance and often patients may have few symptoms; d: a target urine output of 300ml/hr should be achieved.
REFERENCES and FURTHER READING
- De Meijer AR, Fikkers BG, de Keijzer MH, van Engelen BG, Drenth JP. Serum creatine kinase as a predictor of clinical course in rhabdomyolysis: a 5-year intensive care survey. Intensive Care Med 2003; 29: 1121-5.
- Brown CV, Rhee P, Chan L, Evans K, Demetriades D, Velmahos GC. Preventing renal failure in patients with rhabdomyolysis. Do bicarbonate and mannitol make a difference? Journal of Trauma, injury, infection and critical care 2004; 56: 1191-6.
- Knochel JP. Mechanisms of rhabdomyolysis. Curr Opin Rheumatol 1993; 5: 725-31.
- Khan FY. Rhabdomyolysis: a review of the literature. The Netherlands Journal of Medicine 2009; 67(9): 272-83.
- Huerta-Alardin AL, Varon J, Marik PE. Bench-to-bedside review: Rhabdomyolysis – an overview for clinicians. Critical Care 2005; 9: 158-69.
- Bosch X., Poch E., Grau JM. Rhabdomyolysis and acute kidney injury. N Engl J Med 2009; 361(1): 62-72.
- Hunter JD, Gregg K, Damani Z. Rhabdomyolysis. Continuing Education in Anaesthesia, Critical Care and Pain 2006; 6(4): 141-3
- Ward M. Factors predictive of acute renal failure in rhabdomyolysis. Arch Intern Med 1988; 148: 1553-7.
- Hogg K. Rhabdomyolysis and the use of sodium bicarbonate and/or mannitol. Emerg Med J 2010; 27: 305-
- Holt SG, Moore KP. Pathogenesis and treatment of renal dysfunction in rhabdomyolysis. Intensive Care Med 2001; 27: 803-11.



