General Topics
QUESTIONS
- What is the safe dose for bupivacaine?
- Which nerves supply nociception to the anterior abdominal wall and what is their course?
- What are the complications of rectus sheath catheter placement?
INTRODUCTION
The aim of modern surgical and anaesthetic practice is to facilitate the rapid recovery of patients with better anaesthesia, surgical techniques and analgesia, resulting in fewer complications and earlier return to normal activities. There are multiple techniques available for post-operative analgesia following laparotomy. These include patient controlled analgesia (PCA), epidural analgesia and intermittent injection of local anaesthetic agents via a rectus sheath catheter. All these modalities have risks and benefits that must be considered when planning post-operative pain management. In our institution we are using rectus sheath catheters placed by the operating surgeon with increasing frequency and have found this to be an efficient and safe technique.
BACKGROUND
The use of rectus sheath catheters for the administration of local anaesthetic is not new. In the 1950s several studies reported on the use of local anaesthetic catheters to reduce post operative pain post gynaecological and general surgical procedures 1-3. This technique has been further investigated with several papers demonstrating the benefit of either continuous or bolus administration of local anaesthetic 4-9, and others showing no difference10-13. The technique is based on the blockade of the anterior division of T6 – T11 thoraco-abdominal intercostal nerves. These nerves leave the spinal cord dividing into anterior and posterior divisions. The anterior divisions pass posteriorly to the costal cartilages and then between the transverses abdominis and internal oblique muscles, before passing medially to pierce and supply sensation to the rectus and overlying skin. Therefore a catheter placed anterior to the posterior sheath will block these nerves and achieve reduced pain fibre transmission from a midline laparotomy wound. (Fig 1)
METHOD
There have been several methods described for the placement of the rectus sheath catheters. The catheter can be inserted either under ultrasound guidance or as in this method where the operating surgeon places it under direct vision at the end of the procedure. This has the added advantage of being a simple technique that can be performed quickly and does not rely upon the immediate availability of ultrasound guidance.
We use epidural catheters which have multiple perforations at the end of the tubing (Smiths-medical 16G epidural mini-pack). Two catheters are place at the superior end of the laparotomy wound. The surgeon places one hand inside the abdomen and with the other hand inserts the introducer needle. The surgeon can feel when the atraumatic needle is in the interface between the peritoneum and muscle layer, and can also palpate and avoid the inferior epigastric artery. The stylet is then removed and the epidural catheter fed through until a 5cm length is in the peritoneum-muscle interface. The surgeon holds onto the catheter whilst the needle is removed. The catheter is secured at this point, as they can be accidentally pulled out. We use adhesive epidural catheter dressings (Smiths-medical ‘Lock-it plus); other centres secure them with silk or other suitable suture material. (Fig 2,3) Once secured, a bacterial filter is connected and the catheter is flushed as they can occlude if left during abdominal closure. The procedure is repeated on the controlateral side and 20mls of 0.25% plain levo-bupivicaine is injected into each side. This initial bolus will block the intercostal nerves and augment analgesia as the anaesthetic is ended and through the recovery period until the next bolus. On the ward nursing staff administer local anaesthetic every 6 hours in to each catheter, usually with around 20mls of 0.25% levo-bupivicaine (the safe dosage is 2mg/kg every 6 hours). The catheters must be inspected everyday for signs of infection or occlusion. They are usually weaned by day 4 but may be left in for up to a week. Although this technique is opioid-sparing, for large laparotomy wounds a PCA is commonly co-prescribed for the first 24hours.
CONCLUSION
We have found this technique to be safe and provide good additional pain relief in most patients. It has the benefit of being quick, safe and avoids the use of ultrasound which is not available in every hospital. It is also not associated with the risks / side effects of epidural anaesthesia including hypotension, epidural abscess or spinal cord injury.
REFERENCES
- Blades B, Ford WB. A method for control of postoperative pain. Surg Gynaecol Obstet 1950;91: 524-6
- Gerwig WH, Thompson CW, Blades B. Pain control following upper abdominal operations. Arch Surg 1951;62: 678-82
- Lewis DL, Thompson WAL. Reduction of post operative pain. Br Med J 1953;1: 973-4
- Patel JM, Lanzafame RJ, Williams JS, Mullen BV, Hinshaw JR. The effect of incisional infiltration of bupivacaine hydrochloride on pulmonary function, atelectasis and narcotic needs following elective cholecystectomy. Surg Gynecol Obstet 1983; 157: 338–40.
- Chester JF, Ravindranath K, White BD, Shanahan D, Taylor RS, Lloyd- WilliamsK. Wound perfusion with bupivacaine: objective evidence for efficacy in postoperative pain relief. Ann R Coll Surg Engl 1989; 71: 394–6.
- Levack ID, Holmes JD, Robertson GS. Abdominal wound perfusion for the relief of postoperative pain. Br J Anaesth 1986; 58: 615–9.
- Chen TF, Clarke N, Bowen R, Harper NJ, Payne SR. Intermuscular bupivacaine infusion for control of pain after renal surgery: a preliminary report. Br J Urol 1994; 74: 155–9.
- Cheong WK, Seow-Choen F, Eu KW, Tang C, Heah SM. Randomized clinical trial of local bupivacaine perfusion versus parenteral morphine infusion for pain relief after laparotomy. Br J Surg 2001; 88: 357–9.
- Mecklem DWJ, Humphrey MD, Hicks RW. Efficacy of bupivacaine delivered by wound catheter for post caesarean section analgesia. Aust NZ J Obstet Gynaecol 1995; 35: 416–21.
- Padmanabhan J, Rohatgi A, Niaz A, Chojnowska E, Baig K, Woods WGA. Does Rectus sheath of bupivicaine reduce postoperative opoid requirement? Ann R Coll Surg Engl 2007; 89: 229-232
- Gibbs P, Puroshotham A, Auld C, Cuschieri RJ. Continuous wound perfusion with bupivacaine for postoperative wound pain. Br J Surg 1988; 75: 923–4.
- Thomas DFM, Lambert WG, Lloyd-Williams K. The direct perfusion of surgical wounds with local anaesthetic solution: an approach to postoperative pain? Ann R Coll Surg Engl 1983; 65: 226–9.
- Russel WC, Ramsay AH, Fletcher DR. The effect of incisional infiltration of bupivacaine upon pain and respiratory function following open cholecystectomy. Aust NZ J Surg 1993; 63: 756–9.
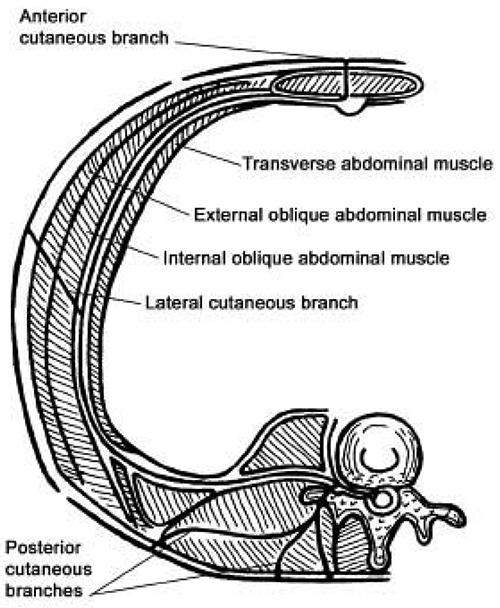
Figure 1: Axial cross-section of abdomen demonstrating anatomy of intercostal nerves.
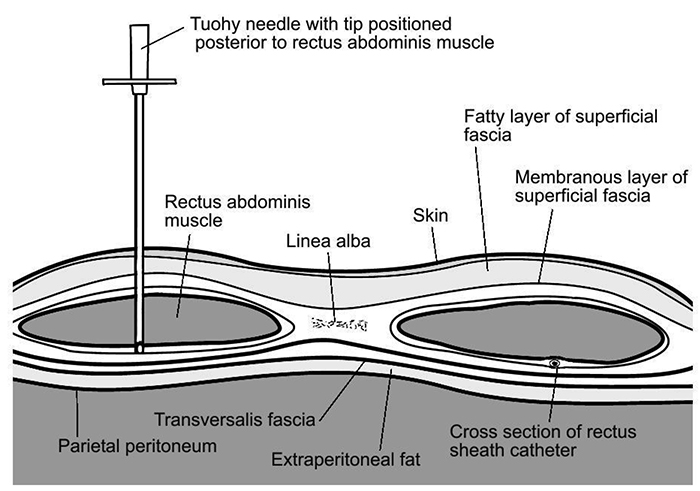
Figure 2: Cross section of abdominal wall illustrating rectus sheath catheter placement. (With permission of David Wilkinson and Katrina Webster)
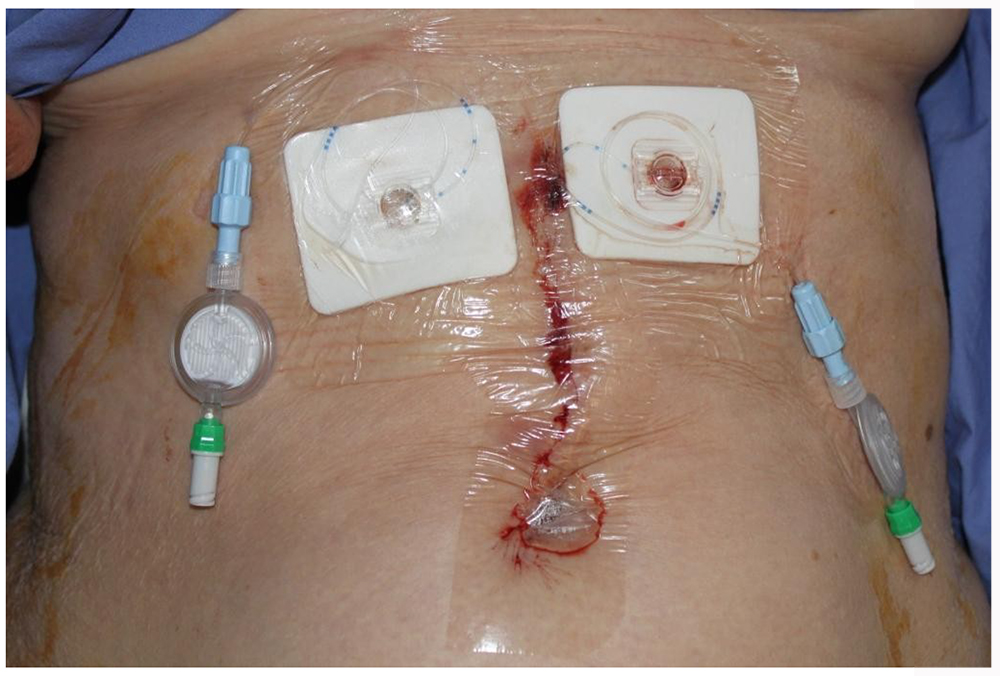
Figure 3 Rectus sheath catheters in place



