Basic Sciences
QUESTIONS
Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation.
- What is a laser?
- What is laser wavelength?
- What is a laser diode?
- What is a gas laser?
INTRODUCTION
LASER is an acronym for Light Amplification by Stimulated Emission of Radiation which describes the theory of laser operation. Albert Einstein published the theoretical basis for the laser in 1917, but it was only in 1960 that the first functioning laser was constructed by Theodore Maiman in California, using a ruby crystal to produce laser light. An extract from the newspaper article following a public demonstration of the laser, read:
“Suddenly a light from hell appeared in the middle of the ruby. Then, from the end of a cylinder, a hundred thousand times brighter than the sun, burst forth a thin red light, a perfectly parallel monochromatic beam. Maiman and his assistants were silent for some time, enthralled by the beauty of this spectacle… ‘Einstein was right’ he murmured, ‘light can be concentrated and coherent.”
The device produces a beam of coherent light with a specific wavelength in the infrared, visible or ultraviolet regions of the electromagnetic spectrum. Further development of this technology led to lasers becoming widely used in medical practice.
LASER PHYSICS
Properties of laser light
Unlike other forms of light, laser light has special properties which make it significantly more effective and dangerous than conventional light of the same power. The laser light particles (photons) are usually:
- Monochromatic: consisting of a single wavelength or colour
- Coherent: photons are in phase (like marching soldiers)
- Collimated: photons are almost in parallel (aligned), with little divergence from the point of origin
Components of a laser
A laser consists of 3 basic components:
- A lasing medium or “gain medium”:
May be a solid (crystals, glasses), liquid (dyes or organic solvents), gas (helium, CO2 ) or semiconductors - An energy source or “pump”:
May be a high voltage discharge, a chemical reaction, diode, flash lamp or another laser - An optical resonator or “optical cavity”:
Consists of a cavity containing the lasing medium, with 2 parallel mirrors on either side. One mirror is highly reflective and the other mirror is partially reflective, allowing some of the light to leave the cavity to produce the laser’s output beam – this is called the output coupler.The laser is usually named according to the type of lasing medium. This also determines the type of pump required and the wavelength of the laser light which is produced.
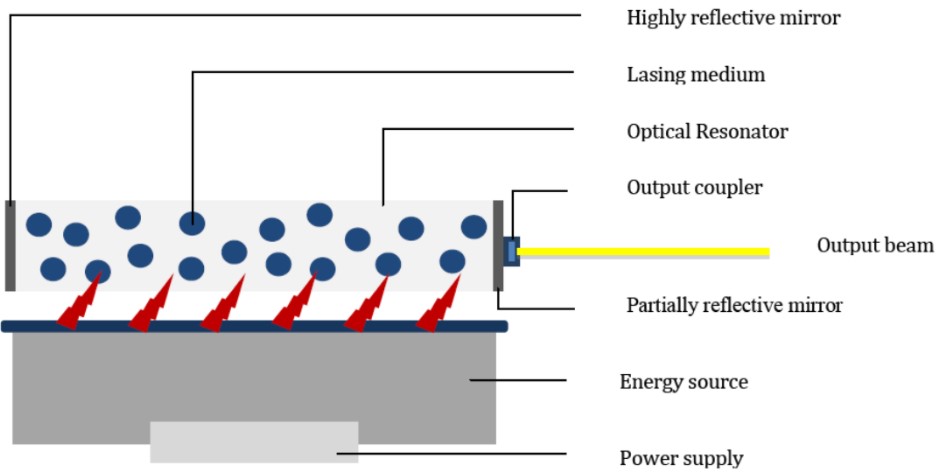
Figure 1. The 3 Components of a laser
The laser is usually named according to the type of lasing medium. This also determines the type of pump required and the wavelength of the laser light which is produced.
Principle of operation at atomic level (Figures 2 and 3)
One model in atomic physics describes an atom as a central nucleus of protons and neutrons, surrounded by a cloud of electrons which encircle the nucleus in different orbitals. When appropriate energy is supplied to the atom, electrons can jump from low-energy orbitals (ground state) near the nucleus to high-energy orbitals further away, leading to atomic excitation by the process of energy absorption.
Some of the electrons in the high-energy orbit spontaneously return to the ground state, releasing the difference in energy in the form of a photon, with a wavelength which depends exactly upon the difference in energy of the 2 states and has a random phase and direction. This process is called spontaneous emission and forms the basis of light emitted by a neon sign, fluorescent light bulb and television tube.
This emitted photon can collide with one of the mirrors in the resonating cavity and reflect back into the lasing medium causing further collision with some of the already excited atoms. If an excited atom is struck, it can be stimulated to decay back to the ground state, releasing 2 photons identical in direction, phase, polarization and energy (wavelength). This process is termed stimulated emission.
A cascade effect of stimulated emission of photons occurs, resulting in further amplification (optical gain) and soon many of the atoms emit light along the same axis. For a laser to sustain function, the majority of the atoms must be maintained in the excited state, hence called “population inversion”. This is achieved by the continuous input from the energy pump (continuous wave laser) or by intermittent pumping resulting in a pulsed wave laser.
A small number of photons are allowed to escape from the lasing medium though the partially reflective mirror of the output coupler. This is the usable laser light and may be in the visible spectrum or beyond (infrared or ultraviolet). It is directed to the target via a delivery system which consists of fibre-optic light guides for visible light or a series of mirrors for infrared.
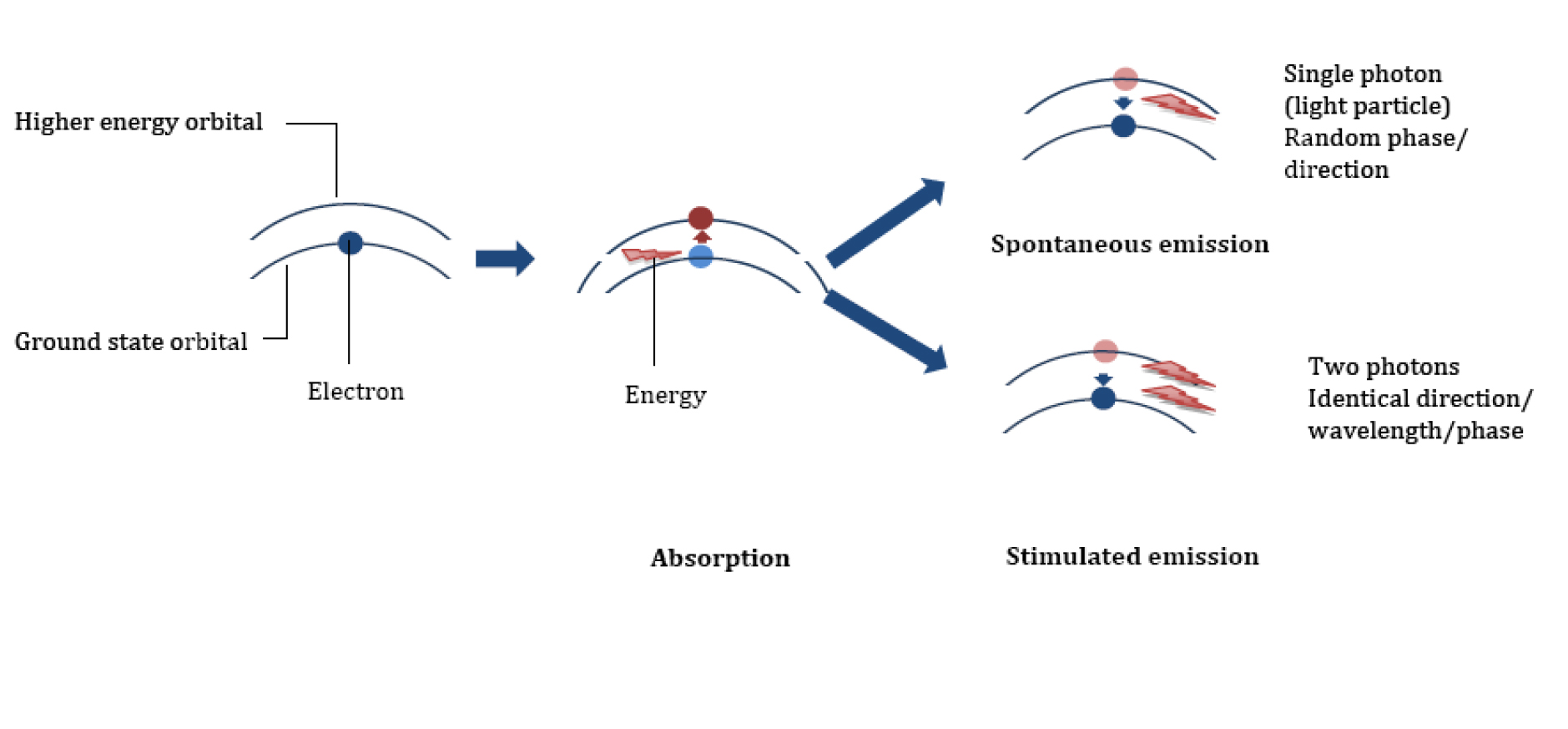
Figure 2. Absorption and Emission
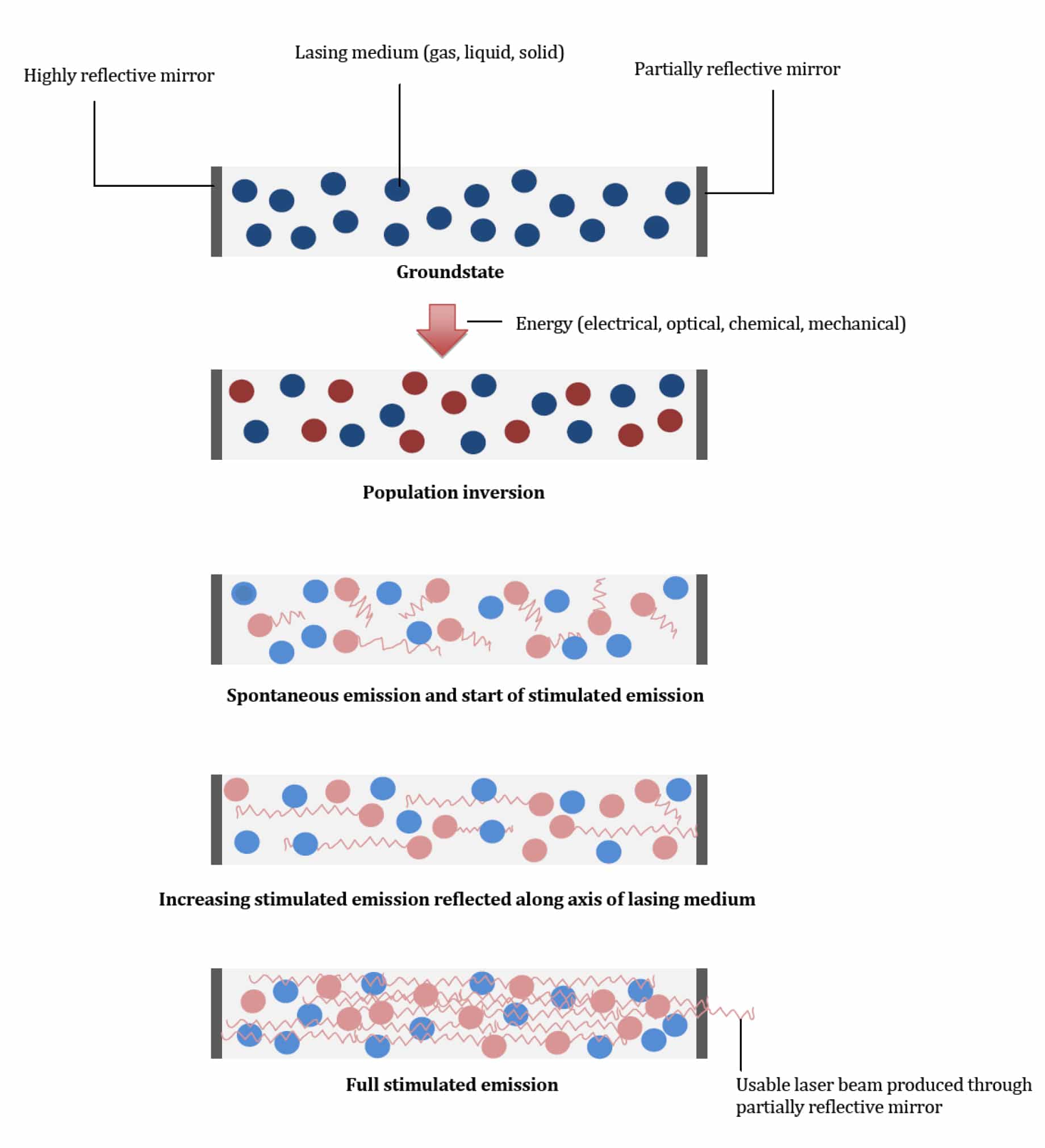
Figure 3. Production of the light beam
MEDICAL LASERS
Medical lasers may be operated in continuous wave or pulsed wave modes. The output of continuous wave lasers is measured as power in watts, and for pulsed lasers the output is measured as energy in joules.
Irradiance, or power density, refers to laser power per unit area (W/cm2)
Fluence, or energy density, is irradiance multiplied by exposure time (J/cm2)
The interaction between the laser beam and the tissue is determined by the wavelength (figure 4), power density and exposure time.
It is the monochromatic nature of laser light that is responsible for its selective effect on biological tissues. When the light comes into contact with the tissues, it can be transmitted, scattered, reflected or absorbed. This depends on the nature of the tissue and the wavelength of the light. The laser light has to be absorbed by the tissue in order to exert biological effects. Examples of the main absorbing components in tissues are:
- Water – absorbs infrared light
- Haemoglobin – absorbs visible light, especially green
- Melanin – absorbs visible and ultraviolet light
The wavelength also determines the depth of penetration. As the wavelength decreases towards the ultraviolet spectrum more scattering occurs which limits the depth of penetration within the tissues. Hence the Argon laser is used for retinal surgery and port-wine birthmarks. The Nd:YAG laser operates at the near infrared spectrum, which has a greater depth of penetration and is therefore used for the cutting and coagulation of tissues.
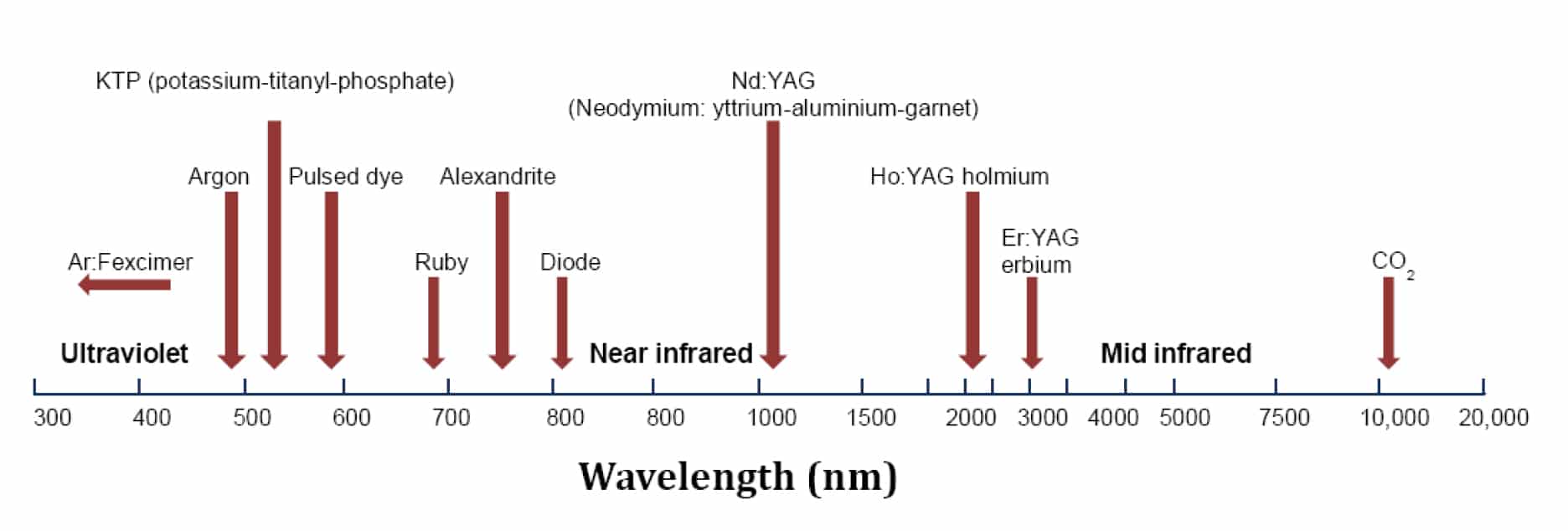
Figure 4. Wavelength of medical laser
Examples of lasers in medical practice
CO2 laser:
Used for cutting and coagulation of soft tissue, which consists primarily of water, e.g. laryngeal surgery. It creates a photo-thermal effect, rapidly heating the tissues. Depending on the exposure time, tissue vaporisation (ablation), coagulation, or both may occur. Pulsing the laser exposure can minimize thermal conduction that may cause collateral tissue damage.
Holmium:YAG laser:
Used for tissue ablation or lithotripsy via a photo-mechanical effect. An extremely intense, but very brief, pulse of laser causes an explosive expansion of the tissue or water within the renal calculi, causing photoacoustic disruption.
Excimer (Argon:Florine) laser:
Used for corneal reshaping. The laser breaks down the covalent bonds in the protein molecules (photodissociation), resulting in non-thermal ablation.
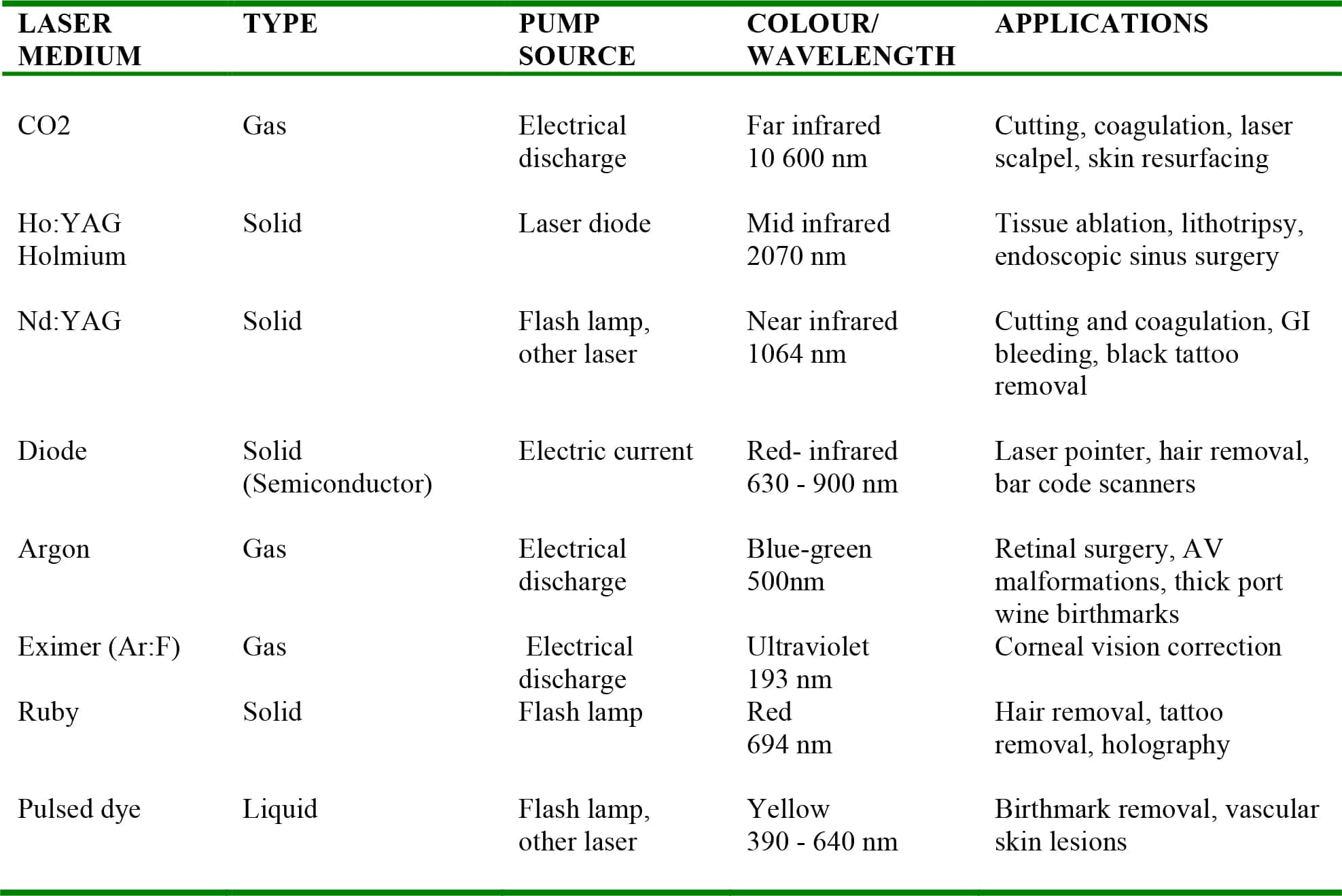
Table 1. Examples of medical lasers
HAZARDS AND LASER SAFETY
The properties of laser light make it significantly more effective and dangerous than conventional light of the same source, i.e. a 30W surgical CO2 laser compared with a 60 W incandescent light bulb. A laser delivers much greater irradiance than a conventional light source of the same power, as the light is coherent (resulting in constructive interference at the target) and collimated (negligible loss of power with distance from the source). Both direct and reflected laser beams are therefore potentially dangerous. The principle dangers are injury to the eye, burns and ignition. Laser light from the ultraviolet to the far infrared wavelengths can cause burns to the skin.
If a parallel laser output beam is focused on a smaller spot using a lens, it greatly increases the power density at the focal point. The lens of the eye may refocus stray visible or near infrared laser light onto the retina, causing painless retinal burns which can result in a permanent blind spot in the field of vision due to damage to the photoreceptors. Staring directly into a laser beam should be avoided. Safety goggles must be appropriate for the specific laser in use, giving protection at the appropriate wavelength.
Classification
The classification of lasers is based on the Maximum Permissible Exposure (MPE) levels and effects on the eyes and skin. MPE is a calculation of the highest power density (W/cm2) or energy density (J/cm2) allowed for a laser that is considered to be safe and unlikely to cause damage. MPE is measured at the skin or the cornea of the eye, for a given wavelength or exposure time.
The International Electrotechnical Commission (IEC) standard 60825-1 (2007) include methods of calculating MPE levels and defines seven classes of lasers. Class 1, 1M, 2, 2M, 3R, 3B and 4 with Class 1 the safest and class 4 the highest and most dangerous class of laser. Medical lasers are in category 4.
Anaesthesia related risks
Injury or deaths resulting from the use of medical lasers have been mostly associated with upper airway surgery, especially airway fires. The effects of lasers on anaesthetic agents and equipment, as well as on the shared airway, must be anticipated and methods for avoiding these complications should be employed.
Endo tracheal tubes:
Direct or reflected laser beams can ignite non-metallic endotracheal tubes. Laser resistant tracheal tubes are commercially available and are constructed of a flexible stainless steel spiral. These tubes are non-combustible, easily sterilised, gas tight and non-reactive with human tissue. Alternatively, conventional PVC tubes may be wrapped with self-adhesive non-reflective metal tape, which is adequate, but not without danger.
The cuff is also vulnerable to rupture by the laser beam. If a cuff inflated with air is ruptured, it allows a massive leak of anaesthetic gasses, providing a richer environment for possible ignition. Filling the cuff with saline will acts as a heat sink and ensure that the heat from the laser beam is dissipated. Methylene blue may be added to the saline to provide a visible indication of inadvertent rupture. An additional safety measure is to have twin distal cuffs.
Skin and eyes:
Combustible drapes should be avoided, and spirit-based solutions to clean the skin should either be avoided or allowed sufficient time for evaporation. Drapes must not create pockets for accumulation of oxidizing agents. Any exposed facial hair can be coated with aqueous lubricating jelly to make it non-combustible. The patient’s eyes should be protected by taping them shut and covering with moist eye pads.
Gas mixtures:
Neither nitrous oxide nor oxygen are flammable, but as nitrous oxide is a better oxidizing agent than oxygen, it does support combustion at very high temperatures and should be avoided especially in open anaesthetic systems. Provided adequate oxygenation occurs, an oxygen concentration of less than 30% in nitrogen or helium as a carrier gas is recommended.
Steps in the management of an airway fire:
The triad of fuel (tube, drapes, skin prep), oxidizing agent (oxygen) and heat (laser beam) may cause a theatre or airway fire. The following steps should be taken in this event;
- Discontinue laser surgery and make the surgeon aware
- Stop ventilation
- Disconnect the oxygen source
- Remove the burnt endotracheal tube
- Douse operating site in water
- Re-instate ventilation via a self-inflating bag or re-intubate and ventilate with room air
- Perform a rigid bronchoscopy to assess the extent of the thermal injury and remove foreign bodies / debris. Plan further management accordingly i.e. tracheostomy
- Commence a short course of steroid therapy if indicated to prevent inflammation
- Consider antibiotic therapy and transfer to critical care for ventilator support if concerned about upper airway swelling or injury to the lungs
Theatre safety
A formal safety programme that defines the hazards of the laser to be used and the control of those hazards (including clinical aspects) should be instituted and a designated advisor should ensure that all the personnel are adequately trained. The hazard classification of the laser should be clearly marked on the outer casing. Laser should only be used by those trained to do so. Only the person using the laser must be able to activate it and it should be placed in the standby mode when not in active use. Regular servicing of the equipment and maintaining a log of laser use will minimize the risk of an accident. An appropriate non-water based fire extinguisher should be available in the clinical area.
All personnel in theatre should wear protective eyewear. The designated theatre must be clearly identified as a “laser controlled area” and warning signs placed at all the entry points to restrict admission. Non-essential doors have to be locked and the windows covered to prevent injury to passers-by.
SUMMARY
- LASER is an acronym for Light Amplification by Stimulated Emission of Radiation
- Laser light has a single wavelength, is coherent and collimated
- A laser is constructed from 3 basic components: a lasing medium, an energy source and an optical resonator
- Laser is produced by the energy released by electrons moving from high-energy to low-energy orbits , followed by the collision with excited atoms (stimulated emission) releasing 2 photons identical in wavelength, phase and in parallel.
- Laser light has to be absorbed by the tissue in order to exert biological effect. The main absorbing components are water, melanin and haemoglobin.
- The wavelength determines the depth of penetration.
- The principle dangers of lasers are damage to the eye, burns and flammability.
ANSWERS TO QUESTIONS
- “Laser” is an acronym for Light Amplification by Stimulated Emission of Radiation. A laser generates energy in the form of light which is in or close to the optical portion of the electromagnetic spectrum. The laser energy is amplified to extremely high intensity by an atomic process called stimulated emission. The color of the laser is defined by the laser wavelength.
- Laser light and energy can be thought of as a continuous series of waves that define the laser output. The distance between these waves, crest to crest, is referred to as the laser’s wavelength and is typically measured in nanometers (nm). Lasers with a wavelength of 400 to 700 nm produce energy or light in the visible spectrum, which we can see. Lasers with shorter wavelengths in the 100 to 400 nm range are called Ultraviolet (UV) and those with longer wavelengths in the range of 700 nm to 1mm are in the infrared (IR) spectrum.
- A laser diode, also known as a semiconductor laser, is a light-emitting diode that uses stimulated emission to form a coherent light output. Typically, laser diodes are small, compact electronic devices that can be placed into housings and have a small window on the end where the laser light is emitted. The light exits the diode in many directions and a lens or collimating system is then used to form a collimated beam of laser light.
- Gas lasers typically rely on a pair of mirrors placed into a gas atmosphere and the laser energy is formed by an external optical source or an electric arc. The increasing laser energy, caused by stimulated emission, is reflected between the pair of opposing mirrors and eventually passes through one of the mirrors as a collimated beam of laser energy. Gas lasers are typically defined by the gas or gasses used in the laser cavity, for example; Argon, Helium-Neon and CO2.
FURTHER READING
- Medicines and Healthcare products Regulatory Agency. DB 2008(03) Guidance on the safe use of lasers, IPL systems and LEDs. Also available at:
http://www.mhra.gov.uk/Publications/Safetyguidance/DeviceBulletins/CON014775 (accessed 17 December 2010). - Laserfest: celebrating 50 years of laser innovation, http://www.laserfest.org (accessed 21 December 2011).
- Bayley G, McIndoe AK. Fires and explosions. Anaesthesia& Intensive Care Medicine. 2004;5:364–366
- ERCI .A clinician’s guide to surgical fires. Health Devices. 2003;32:5–25
- Muchatuta NA, Sale SM. Fires and explosions. Anaesthesia & Intensive Care Medicine. 2007;8:457–460



