Regional Anaesthesia
QUESTIONS
Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation.
- Which one of the following statements is incorrect?
- The paravertebral space communicates laterally with the intercostal space and medially with the intervertebral foramen.
- When performing a thoracic paravertebral block sympathetic blockade is essential for reliable postoperative analgesia.
- In a 70kg patient 5 dermatomes can safely be anaesthetised using 5 injections, each of 5ml 0.5% bupivacaine.
- The superior aspect of the tip of the spine of T2 lies adjacent to the transverse process of T2.
- Which of the following are relative contraindications to thoracic paravertebral block?
- Ipsilateral empyema
- Mesothelioma
- Competent adults declining the procedure
- Previous anaphylaxis to procaine.
- Before surgery, under general anaesthetic and 20 minutes after insertion of a paravertebral block a patient has a cardiac arrest. Which of the following are possible causes?
- Local anaesthetic toxicity
- Hypotension due to sympathetic blockade
- Anaphylaxis
- Tension pneumothorax
INTRODUCTION
In 1905 Hugo Sellheim performed the first documented thoracic paravertebral block (TPVB) in Leipzig. Originally the technique was used to provide muscle relaxation and anaesthesia for upper abdominal surgery.1 The introduction of curare and volatile gases replaced the need for TPVB. Concerns about the safety of the block accentuated the decline of its use. In 1979 a “seminal” paper describing a loss of resistance technique reignited interest in TPVB.2 Evidence and experience in the use of paravertebral blockade has mounted. It can be used for abdominal, thoracic and breast surgery, chronic pain and other niche areas (see indications below). The safety concerns from previous decades have proved to be unfounded with TPVB having a comparable rate of complications to thoracic epidurals and intercostal blockade.3
As TPVB use has risen other possible clinical benefits have been explored. Early research has suggested a reduction in breast cancer recurrence in patients where TPVB was used for their initial mastectomy.4 A large phase III multinational, multicenter trial is presently recruiting to examine breast cancer five year recurrence rates in patients receiving TPVB compared to morphine postmastectomy.5
ANATOMY
Paravertebral blockade (PVB) is achieved by placement of local anaesthetic around the nerve bundles as they arise from their corresponding intervertebral foramina. PVB is often used without prefix to refer to thoracic PVB (TPVB). It should be noted that cervical stellate ganglion block), lumbar paravertebral blocks and lumbar plexus blocks are also types of PVB. For clarity a spinal level should be stated when describing the block as the anatomy will obviously differ.
The thoracic paravertebral space (TPVS) is a wedged shape with the apex lying laterally and the base medially as shown in Figure 1.
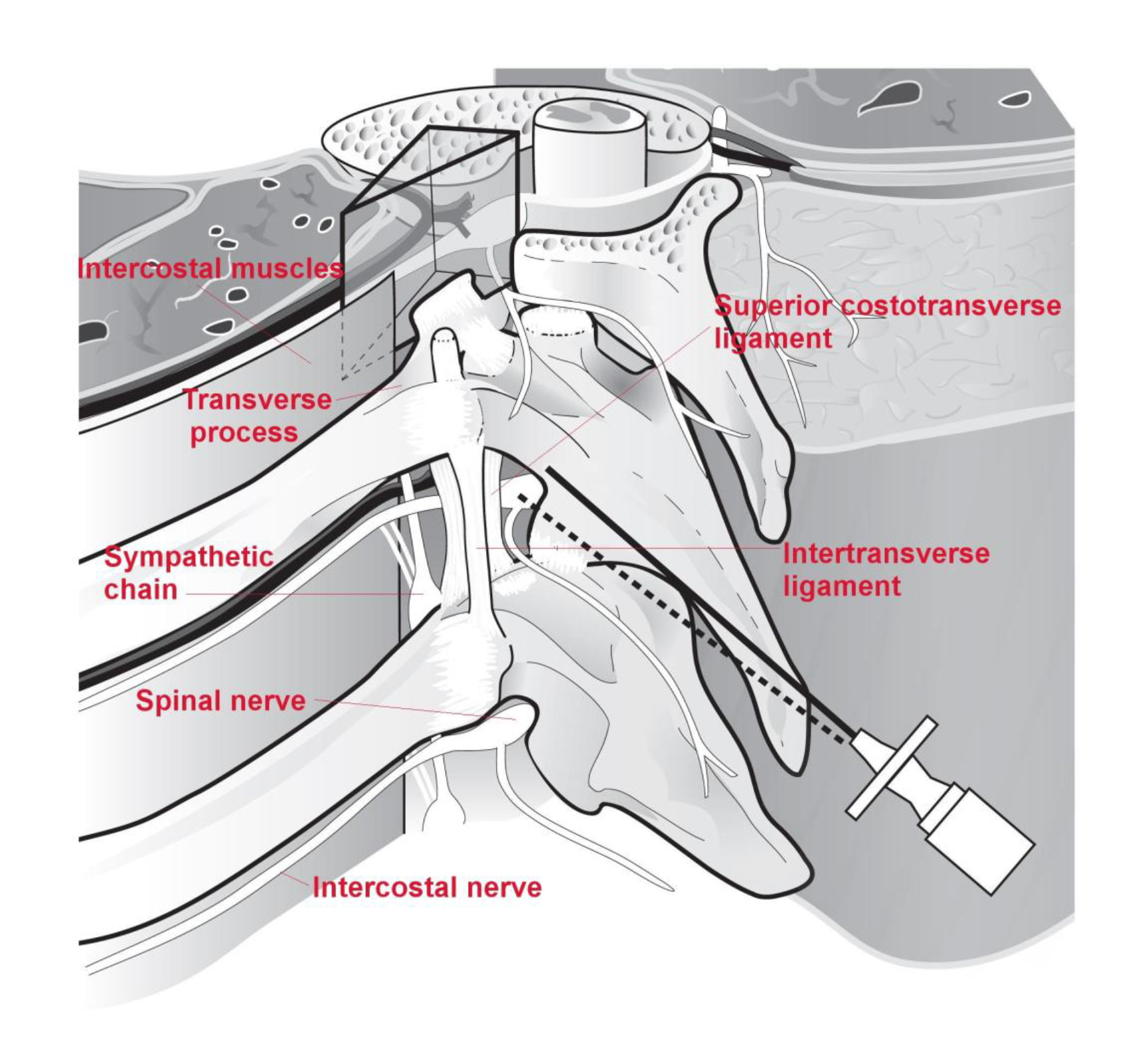
Figure 1: Drawing of the thoracic paravertebral space. The boundary of the space is depicted by a transparent wedge.
Relationships
Anterolaterally (from posterior to anterior) lie the parietal pleura, the pleural space, visceral pleura and lung parenchyma.
Medially lies the posterolateral portion of the vertebral body, the vertebral disc and the vertebral foreman with its corresponding spinal nerve.
Posteriorly the TPVS is limited by the superior costotransverse ligament.
Laterally the space is bound by the posterior intercostal membrane and the intercostal space.
Communications
The TPVS is continuous from T1 to T12. For descriptive purposes the space is split into dermatomes and each segment of the PVS is said to be limited superiorly and inferiorly by the heads of the corresponding ribs. The cervical and thoracic PVS are directly continuous with one another. There are conflicting contrast studies in cadavers with regards a communication between the thoracic and lumbar PVS. Clinically lumbar plexus block is rarely seen following lower TPVB.
The TPVS communicates medially with the epidural space via the intervertebral foramina and laterally with the intercostal spaces. The prevertebral fascia lies anterior to the vertebral bodies and can provide a conduit to the contralateral TPVS for local anaesthetic but this is unusual.
The TPVS may be divided into anterior and posterior segments by the endothoracic fascia. This a thin fibroelastic structure and may affect the pattern of spread of local anaesthetic during TPVB. The existence of the endothoracic fascia is debated.
Nerves
The nerve root passes through its respective intervertebral foramen to enter the medial aspect of the TPVS. There is no fascial sheath covering the nerve as it emerges as a loose bundle of neurones. This allows for direct and quick action of local anaesthetic on the neurones. Each root projects a somatic dorsal ramus and a ramus communicantes within the medial aspect of the TPVS. The larger ventral portion passes through loose areolar tissue and exits the TPVS via the corresponding intercostal space. The sympathetic chain lies on the neck of the ribs lateral to the heads and anterior to the intercostal bundles. Nociceptive pathways are diverse and multiple and include fibres passing through the sympathetic chain. Blockade of the chain is therefore essential for effective analgesia.
INDICATIONS
TPVB lends itself to unilateral surgery but bilateral TPVB have been described. More superficial surgery such as inguinal hernia repair, mastectomy and breast augmentation can be performed using paravertebral block as the sole anaesthetic technique.
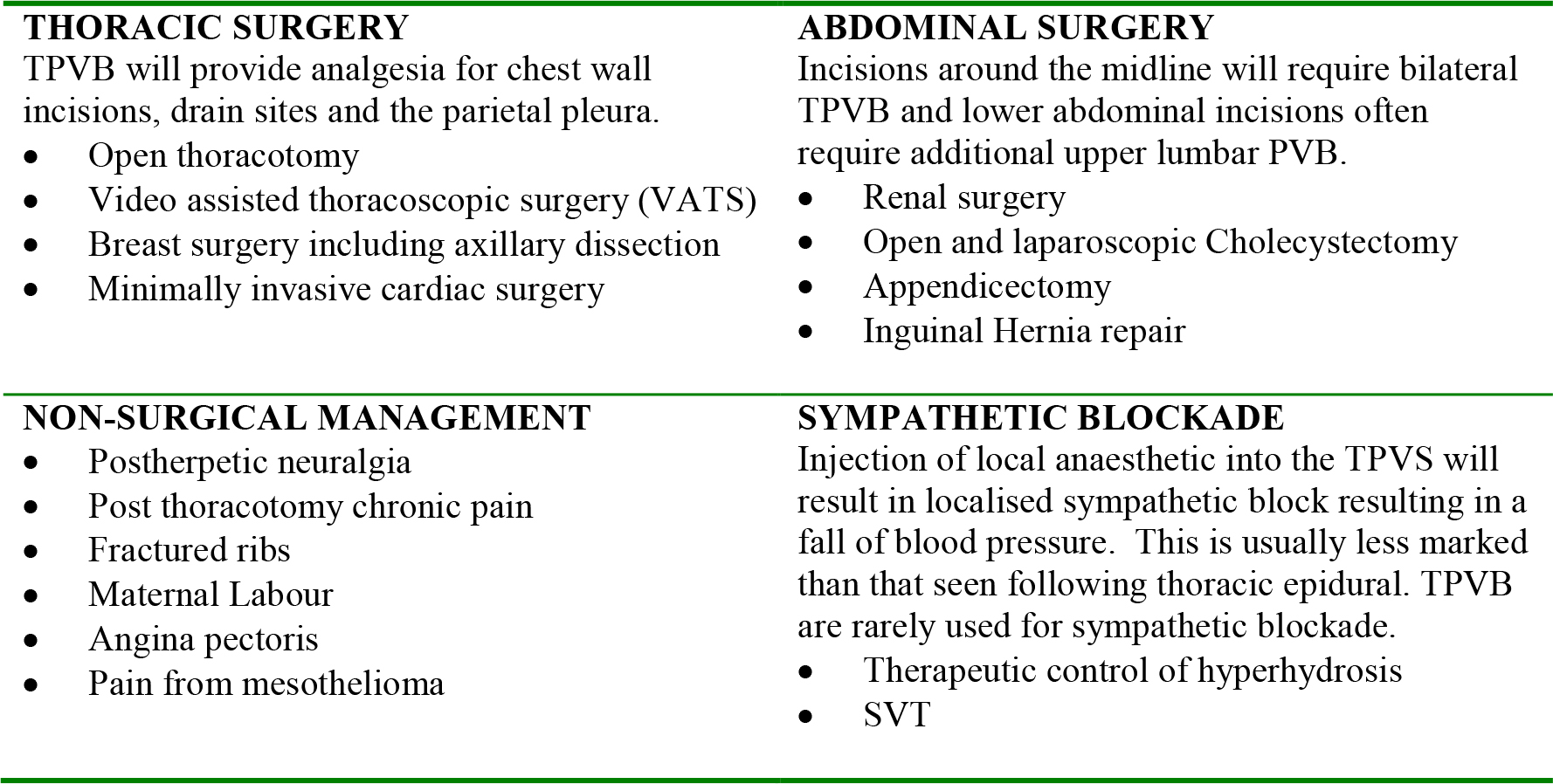
Table 1: Clinical applications of thoracic paravertebral blocks.
CONTRAINDICATIONS
Before any regional procedure a risk assessment must be made and balanced against the patients’ requirements. Perhaps the only absolute contraindications are patients who have an allergy to local anaesthetic or whom decline the procedure. Contraindications should be considered in the context of the surgery, the patient, co-morbidity and alternative forms of analgesia available.
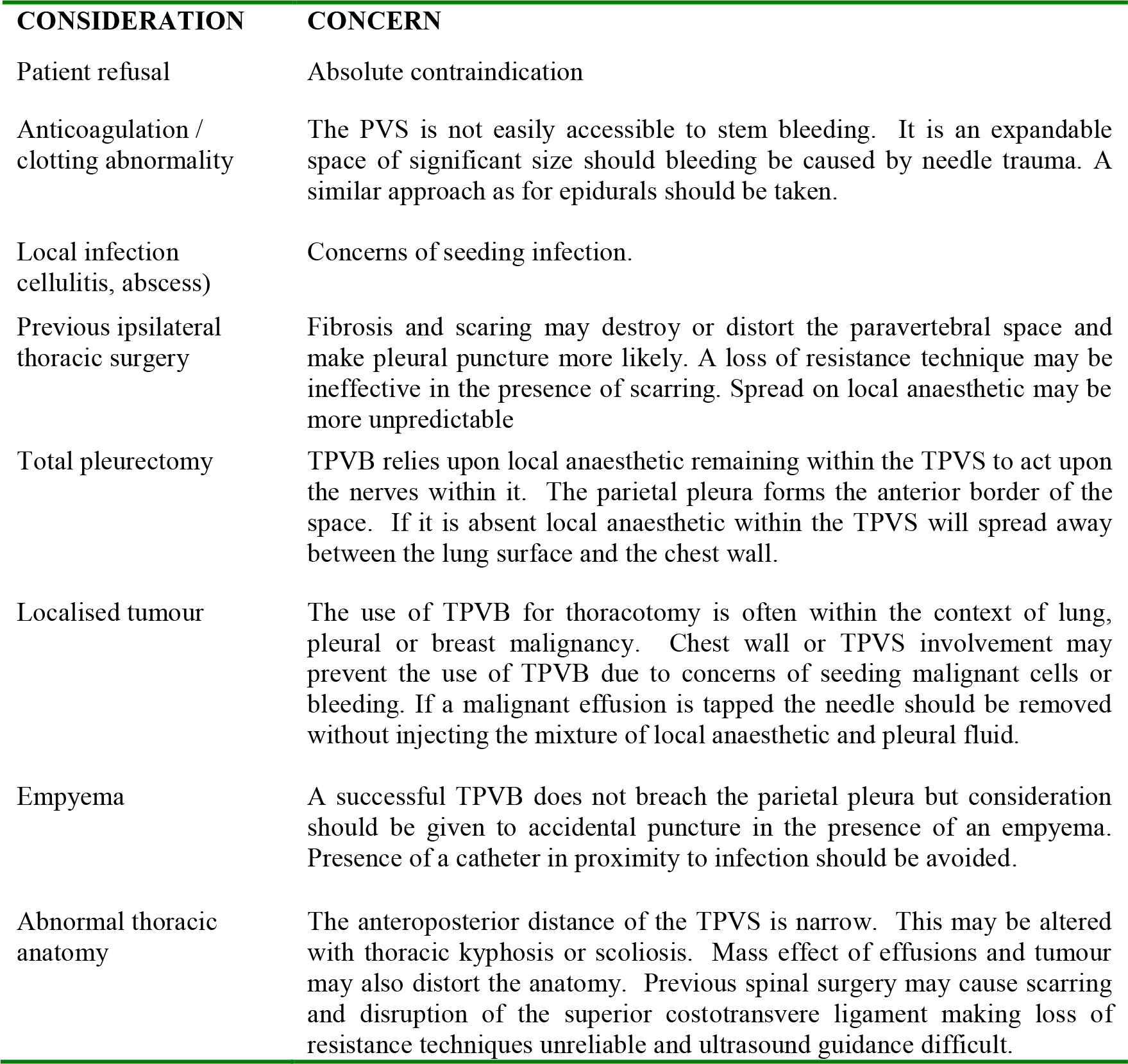
Table 2: Considerations before insertion of a TPVB.
TECHNIQUES
As with all regional anaesthetic procedures: consent must be obtained from the patient; iv access established and standard monitoring attached; resuscitation facilities must be available and the procedure carried out in an aseptic manner.
Spread
The TPVB has been shown to have an unpredictable spread. A large volume injected at a single space may be confined to that space, spread longitudinally across several dermatomes or both. The pattern of spread may depend upon whether the anaesthetic is injected into the dorsal or ventral compartment of the TPVS. The endothoracic fascia, if present, is thin and not amenable to identification by loss of resistance or ultrasound.
A large volume, single injection technique will provide analgesia/anaesthesia for the dermatome level at which it is injected. It will usually spread one or two dermatomes caudal and cranial but reliance on further spread should be avoided. If anaesthesia of several dermatomes is required a small volume, multiple injection technique is recommended. A reliable technique used in our institute uses three injections of 10mls of local anaesthetic separated by several dermatome levels. Typically injections at T3/4, T6/7 and T8/9 are used to provide analgesia for thoracotomy and VATS procedures. The surgical drain sites are covered by this technique. When used for thoracotomy an indwelling catheter is placed to provide continued postoperative analgesia at the level of surgical incision. For VATS procedures no catheter is required. Reducing the number of injections may reduce needle related complication rates and the time the procedure takes to perform.
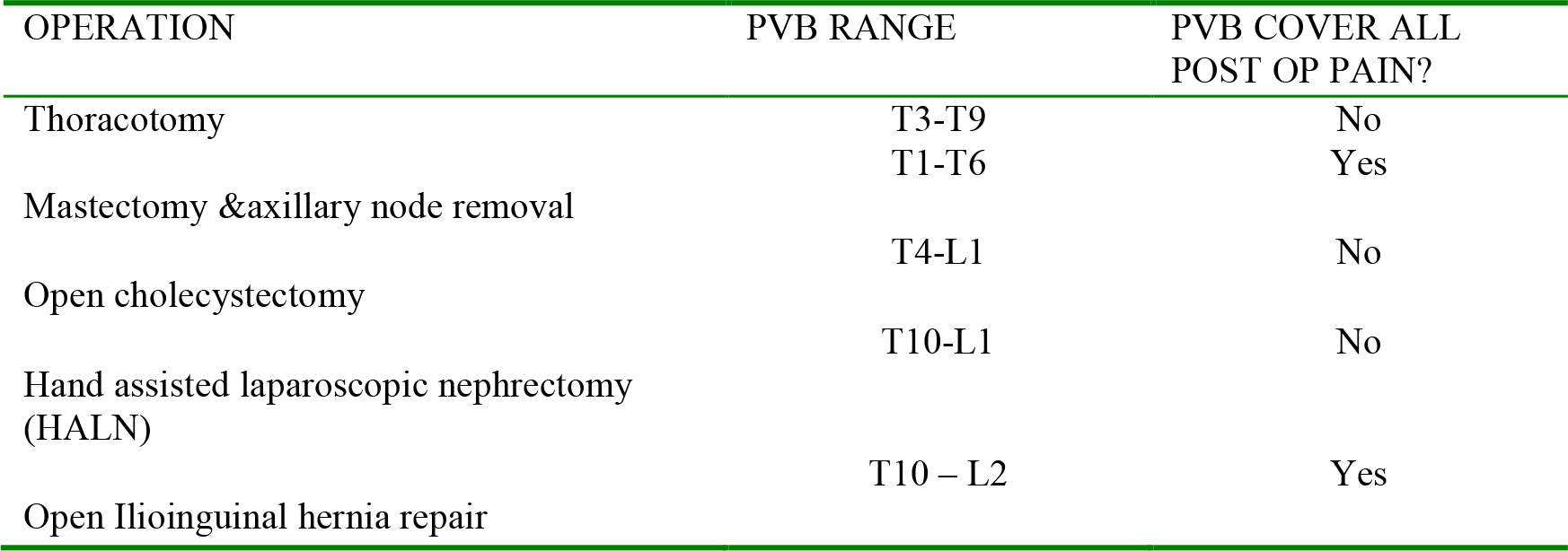
Table 3: The Range of TPVB needed for different operations. Some procedures require additional post operative analgesia due to nerve innervations of differing types.
Patient position
TPVB can be performed with the patient sitting, shoulders and head relaxed and leaning forward or with the patient lying in the lateral position with the side to be operated on uppermost. Sedation may be used. The lateral position is convenient for patients under general anaesthesia and this position commonly matches that for surgery. Debate exists regarding the risks of regional techniques performed either awake or after general anaesthetic. There is no definitive evidence to suggest either state to be safer than the other. An individual approach to each patient is perhaps the best practice including discussion with the patient. Nerve trauma is rare and is reported with both techniques.
Landmarks
The spines of the thoracic vertebrae are angled caudally such that the superior aspect of the tip of the spine lies adjacent to the transverse process of the vertebra immediately below. The tip of the spine of T1 is adjacent to the transverse process of T2.
The spinal process one above the highest level of the dermatome range to be anaesthetised and one above the lowest level are palpated, marked with a sterile pen and a vertical line drawn between these two points. For example if T4-T8 are to be anaesthetised a midline line between the superior level of the T3 and T7 spines is marked. The superior aspect of each spine is then marked along the line.
A parasagittal line, parallel and 2.5cm lateral to the midline mark is drawn on the side to be anaesthetised. Points are marked on the parasagittal line directly adjacent to each of the midline marks. A transverse process lies deep to each parasagittal mark.
Procedures
Landmark technique:
When placing an indwelling catheter a Tuohy epidural kit may be used. Alternatively a 100mm insulated nerve stimulator needle or a spinal needle may be used. A weal of local anaesthetic is raised at each point marked on the parasagittal line. The needle is advanced through the weal perpendicular to the skin in all planes until the bony resistance of the transverse process is met. This depth varies. It is deepest in the higher thoracic area (6-8cm at T1-2) and shallowest at mid thoracic levels (2-4cm at T5-10).
The pleura lies deep to the needle tip as it enters the TPVS and will be breached if the needle is advanced too far. By keeping a syringe attached to the epidural or stimulating needle the risk of pneumothorax is reduced should a breach of the pleura occur. Take note of the depth of the needle and do not insert further than the expected bone contact depth. If this occurs, withdraw the needle, and reassess the landmarks and angle of needle insertion. Needle insertion can then be reattempted. Ensure a perpendicular approach in all planes. A more lateral approach meets the intercostal space, rib or pleura and medially the intervertebral foramen may be entered.
When the transverse process is contacted the needle depth is noted. This will help predict the depth of contact on the subsequent blocks if using the multiple injection technique. The needle is walked off the inferior border of the process and further advanced by approximately 1cm as measured by the needle markings.
After gentle aspiration to check for blood, CSF, pleural effusion and air, the local anaesthetic is injected slowly. Little resistance should be felt. Resistance to injection may indicate the tip of the needle is within the costo-transverse ligament, the vertebral foramen, a nerve bundle or lung parenchyma.

Figure 2: A patient in the lateral position. The superior border of thoracic spines are identified in the midline and the corresponding “x” is 2.5cm lateral to this and marks the entry points for left thoracic paravertebral block.
Loss of resistance technique (LRT)
The LRT landmark technique is employed using an epidural needle. After the needle is walked off the inferior border of the transverse process a loss-of-resistance syringe is connected to the needle hub. Saline or air may be used at the operators’ preference. Resistance to the syringe is provided by the superior costo-transverse ligament. The needle is carefully advanced in the same manner as an epidural technique. Loss of resistance should be found after approximately 1cm. If it is not the needle should be withdrawn to the skin and the process repeated again after checking the landmarks and patient position. The superior costo-transverse ligament provides a subtle resistance and loss of resistance which may not be obvious. If the needle is inserted too laterally the costo-transverse ligament is missed and the first loss of resistance may be the pleural space. This should be suspected if the patient coughs or reports pain. Care should be taken to advance the needle no more than 1cm past the transverse process while remaining perpendicular to the skin.
Nerve Stimulation
The landmark technique is carried out as described above. Before insertion the stimulating needle is connected to a nerve stimulator and set to deliver 2.5mA at 2-5Hz. The return of a train-of-four following muscle relaxation must be confirmed with a peripheral nerve stimulator before starting the procedure. The paraspinal muscles are seen to contract as the needle is advanced past the skin. As the needle tip enters the superior costo-transverse ligament the muscle contraction ceases. Almost immediately on entering the TPVS the somatic nerve is stimulated. The electrical current should be reduced slowly and the needle tip repositioned to provide a muscle contraction above 0.5mA and loss of contraction at or below this current. Corresponding intercostal or abdominal wall contraction will be seen and/or reported by the patient and will disappear on injection of the local anaesthetic.
Ultrasound guided
The use of ultrasound to guide the needle tip into the TPVS has been described recently with low levels of complications and high rates of therapeutic success.6 The use of ultrasound is outside the remit of this article.
Surgical Placement
During thoracotomy or thoracoscopy a TPVB may be reliably placed under direct vision by the surgeon (Figure 3a). The percutaneous approach uses the landmark technique to place an epidural needle in the PVS. From within the thorax the needle tip can be seen to appear in the TPVS as it tents the parietal pleura (Figure 3b). 10-20ml of local anaesthetic is injected and an indwelling catheter then placed under direct vision (Figures 3a and 3b). An alternative method is for the surgeon to make a small incision through the parietal pleura from within the thorax. A subpleural pocket is dissected and local anaesthetic placed within the pocket. No indwelling catheter is used. The pocket is then closed with suture.
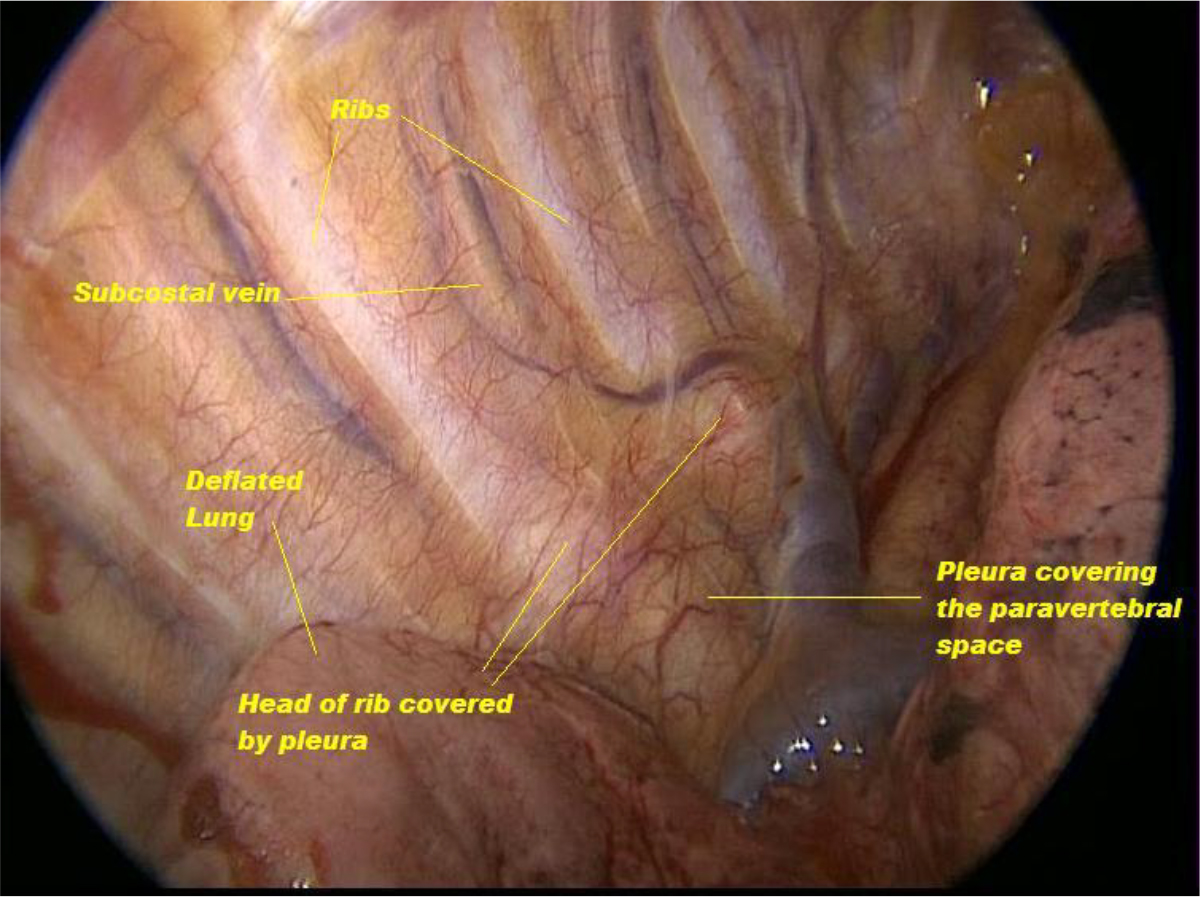
Figure 3a: View of the paravertebral space before percutaneous PVB under direct vision.
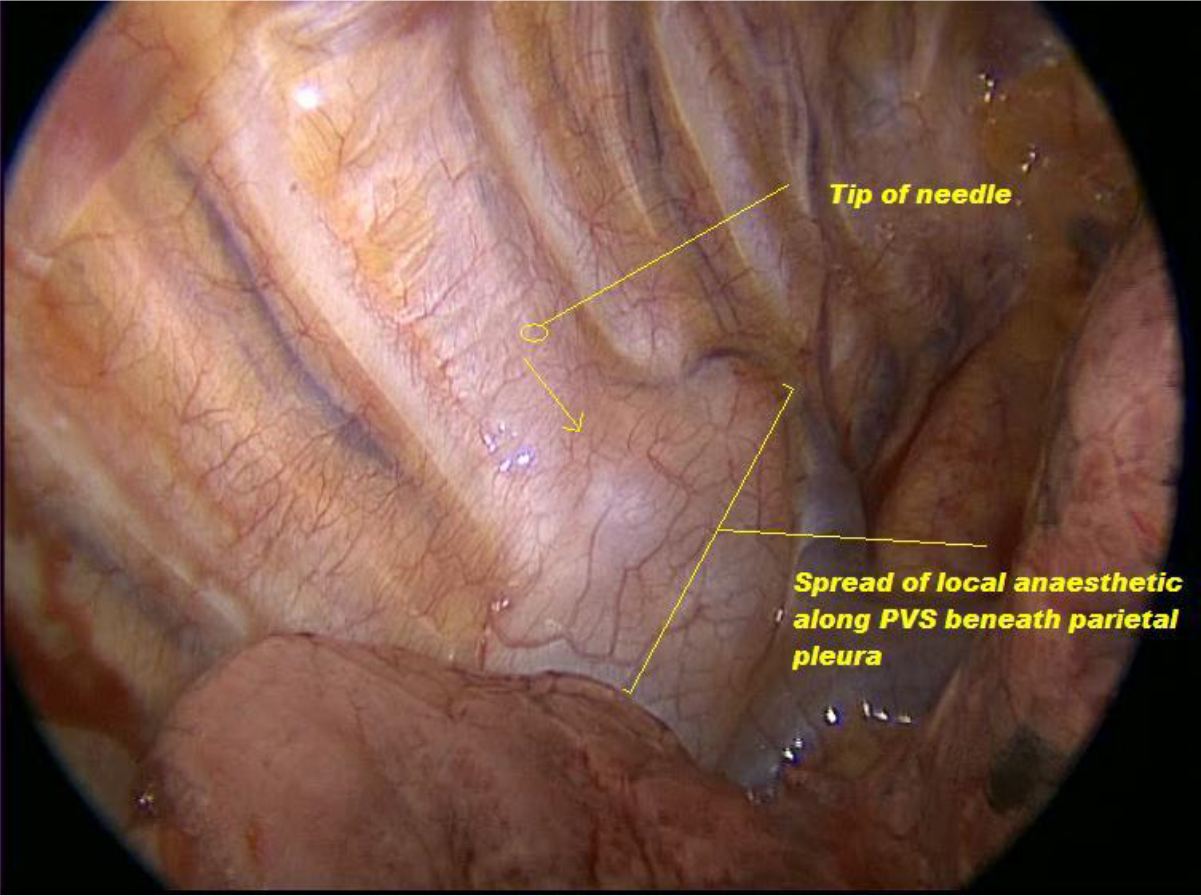
Figure 3b: An epidural needle is inserted percutaneously from the posterior thoracic wall to tent the pleura. The tip is seen to tent the pleura lateral to the PVS in the medial aspect of the intercostal space. The arrow shows medial spread of anaesthetic from the tip into the PVS. The PVS is seen to fill beneath the pleura spreading caudally and cranially.
LOCAL ANAESTHETIC
Typical volumes of 15-30ml of local anaesthetic are needed for PVB. Bupivacaine/Levo-bupivacaine 0.25-0.5% is commonly used in the UK. The higher volumes mean toxic doses are often approached and for this reason the maximum dose should be calculated before the start of the procedure. For thoracotomy the drain site is often several dermatomes below the incision. A lower concentration of anaesthetic may be used to spare a final volume for infiltration at the drain site by the surgeon. The time to peak affect is approximately 40 minutes with peak plasma concentration occurring between 10-60minutes. Vigilance should be kept for some time after injection for signs of local anaesthetic toxicity given the possible delay in peak plasma concentrations.
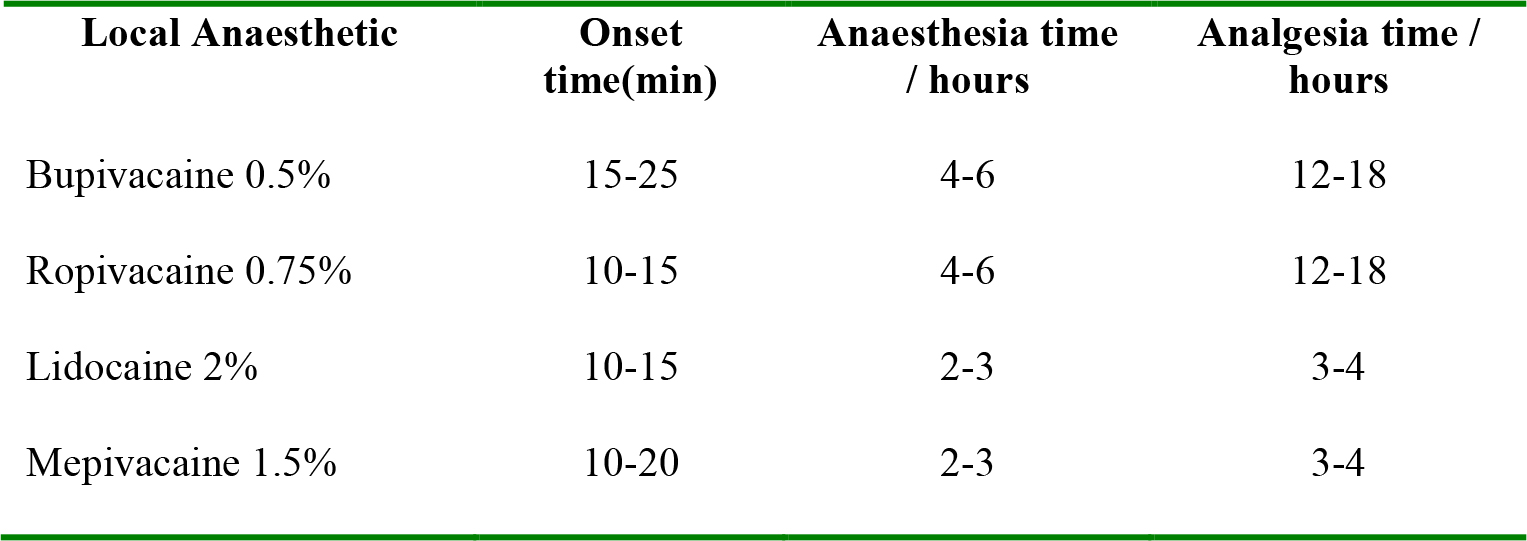
Table 4: Local anaesthetics used for PVB with typical onset, anaesthesia and analgesia times.
COMPLICATIONS
As for any procedure the rate and risk of complications is dependent on factors such as the operators’ experience, patient habitus and anatomical anomalies, equipment and the technique used. The absolute rate of complications for TPVB is therefore difficult to estimate.
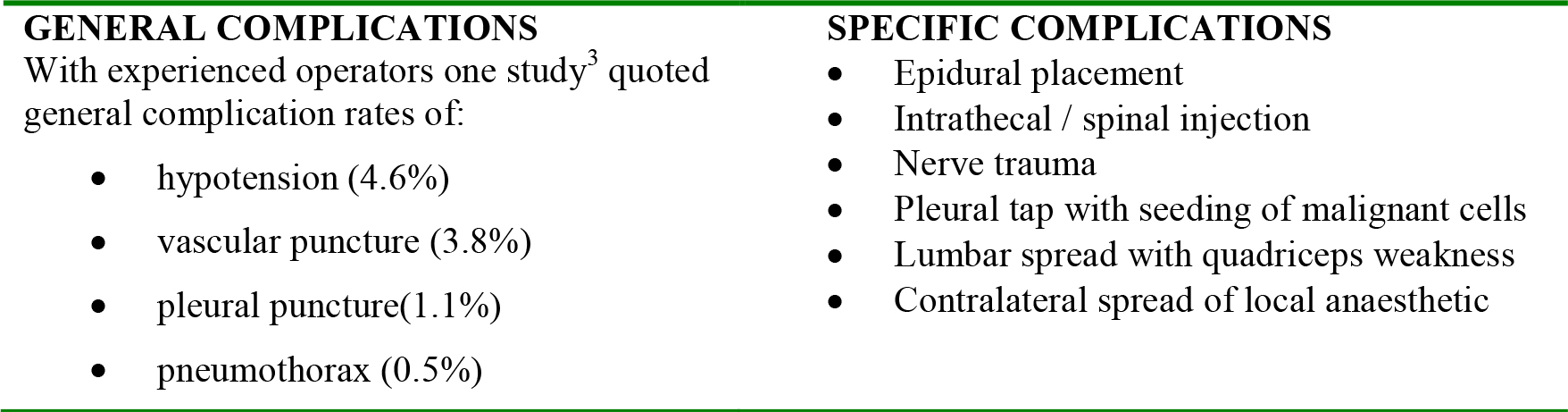
Table 5: General and specific complications of thoracic paravertebral blockade.
The rate of general complications are similar to epidural, intercostal and intrapleural techniques. Use of ultrasound guidance and/or nerve stimulation may reduce complication rates although there is no firm evidence to support this notion.
SUMMARY
- Thoracic paravertebral blocks can be used as analgesia for abdominal and thoracic surgery and also in chronic pain.
- Thoracic paravertebral block has a similar analgesic efficacy and complication rate to other forms of thoracic regional anaesthetic techniques.
- Longitudinal spread of local anaesthetic is unpredictable with a single injection. Multiple injections are recommended.
- Due the large volume of LA needed, doses should be calculated before starting a PVB.
- The antero-posterior distance of the PVS is shallow. If the needle is advanced more than 1cm past the transverse process there is greater risk of pneumothorax.
ANSWERS TO QUESTIONS
- a,b,c are correct. d is incorrect. The superior aspect of the tip of the spines of thoracic vertebrae lie adjacent to the transverse process of the inferior vertebra. The T2 spine lies adjacent to the transverse process of T3.
- a,b,d are relative contraindications. Procaine is an ester and anaphylaxis is commonly due to it’s metabolite para-aminobenzoic acid. Amides (lidoocaine, bupivacaine) are widely used and do not possess this metabolite. Anaphylaxis to amide local anaesthetics is rare. A competent adult declining the procedure is an absolute contraindication.
- a,b,c,d are all possible causes. Toxicity is always a consideration with any regional technique. Doses close to the recommended maximal dose are often used in paravertebral blocks. Peak serum levels may be delayed. Marked hypotension is less common than with thoracic epidural but does occur. Regular monitoring should be commenced before and after injection. Anaphylaxis due to latex or any drug is a consideration in any cardiac arrest. Allergy to amide local anaesthetics is rare but causes other than the block should be considered. Puncture of the pleura can occur during paravertebral insertion and may go unnoticed. Tension pneumothorax may then develop in a ventilated patient.
WEBLINKS
- New York School of Regional Anaesthesia 2009, “Continuous Thoracic Paravertebral Block”, http://www.nysora.com/peripheral_nerve_blocks/classic_block_tecniques/3070-continuous_thoracic_paravertebral_block.html. (accessed: 28th June 2010)
- Defense & Veterans Pain Management Initiative (DVPMI) 2008, Paravertebral nerve block, http://www.arapmi.org/maraa-book-project/Chapt12.pdf. (accessed 28th June 2010)
- Update in Anaesthesia, Volume 25, Number 1 (2009) Page 4-7 http://update.anaesthesiologists.org/wp-content/uploads/2009/10/Update-251-2009.pdf
REFERENCES and FURTHER READING
- J. Richardson and P. A. Lonnqvist. Thoracic paravertebral block. British Journal of Anaesthesia 1998; 81: 230-238
- Eason MJ, Wyatt R. Paravertebral thoracic block-a reappraisal. Anaesthesia 1979; 34: 638-642
- Lönnqvist PA, MacKenzie J, Soni AK, Conacher ID. Paravertebral blockade: failure rate and complications. Anaesthesia 1995; 50: 813–15
- Deegan C.A, Murray D, Doran P, Ecimovic1 P, Moriarty D.C, Buggy D.J, Effect of anaesthetic technique on oestrogen receptor-negative breast cancer cell function in vitro, Br J Anaesth 2009; 103: 685–90
- Outcomes Research Consortium, “Regional Anesthesia and Breast Cancer Recurrence”, http://www.clinicaltrial.gov/ct2/show/record/NCT00418457, (accessed: 1st September 2010)
ACKNOWLEDGEMENTS
Thanks to Neil Hodge Photography, UK for photographic services (Figure 2)
Thanks to Mr John Edwards, Cardiothoracic consultant surgeon, Northern General Hospital, Sheffield, UK for supply of Figure 3a/3b.



