Regional Anaesthesia
QUESTIONS
- Regarding the anterior abdominal wall:
- This is supplied by the posterior primary rami of intercostal nerves T7-T12.
- The muscles of the lateral abdominal wall are the external, internal and innermost oblique muscles.
- The Ilioinguinal and Iliohypogastric nerve are branches of T12 and L1.
- The transversus abdominis plane is between the deep fascia of internal oblique and the superficial fascia of transversus abdominis muscles.
- The Lumbar Triangle of Petit lies between the anterior and mid-axillary lines.
- The TAP block:
- Reliably provides anaesthesia to the entire abdominal wall.
- Is best performed using a high-concentration, low-volume technique.
- Short-bevelled needles provide the best feedback during passage through fascial layers.
- Can be used reliably as the sole mode of analgesia.
- Must always be performed bilaterally.
- With regards to the Ultrasound-Guided TAP block:
- The transversus abdominis plane is best visualised in the midline of the abdomen.
- When advancing the needle during TAP blocks, the needle tip is best seen with an in-plane needle view.
- There is no need to visualise the spread of local anaesthetic with this technique.
- Saline can be used as the initial injectate to open the fascial plane.
- A “posterior” TAP block will spread to cover T7-T9 dermatomes only
INTRODUCTION
The Transversus Abdominis Plane (TAP) Block is a local anaesthetic block used to provide analgesia to the anterior and lateral abdominal wall. Rafi et al (2001)[1] and McDonnell et al (2004)[2] were the first to describe this novel abdominal field block. They described an anatomical landmark technique and provided evidence of blockade to the mid/lower thoracic and upper lumbar spinal nerves as they travelled in the fascial plane between the transversus abdominis and internal oblique muscles. Hebbard et al (2007)[3] have subsequently described an ultrasound-guided approach to the TAP block.
This tutorial will outline the relevant anatomy, the landmark and ultrasound techniques described for TAP Blocks, and some of the evidence for the use of these blocks.
ANATOMY
Muscles of the Abdominal Wall relative to the TAP Block
As we will discuss later, the TAP Block is performed in the lateral part of the anterior abdominal wall. In this region of the abdominal wall there are 3 muscle layers (Fig 1).
The External Oblique Muscle
The external oblique muscle is the largest and most superficial of the 3 muscles. It runs inferiorly from the external, inferior surfaces of the lower 8 ribs. The fibres originating from the lower ribs run inferiorly and insert into the iliac crest. The fibres originating from the middle and uppermost ribs run infero-anteriorly and end in a thick aponeurosis. Anteriorly, the aponeurosis joins the aponeurosis from the transversus abdominis and internal oblique muscles forming the linea alba. Inferiorly the aponeurosis forms the inguinal ligament.
The Internal Oblique Muscle
The internal oblique muscle is a smaller thinner muscle than the external oblique. It originates from the inguinal ligament and the iliac crest. Its’ fibres cover the anterolateral part of the abdomen inserting anteriorly into the linea alba, above the transversus abdominis muscle, and superiorly into the cartilages of the lower 6 ribs.
The Transversus Abdominis Muscle
The transversus abdominis muscle is the most internal of the 3 muscle layers, lying directly beneath the internal oblique muscle. Its’ fibres arise from the inguinal ligament, the iliac crest, the lumbodorsal fascia and the inner surfaces of the cartilages from the lower 6 ribs. Its’ fibres run transversely across the abdomen ending in a broad aponeurosis. This aponeurosis is formed more laterally than the aponeuroses of the external and internal oblique muscles. It continues medially and inserts into the linea alba.
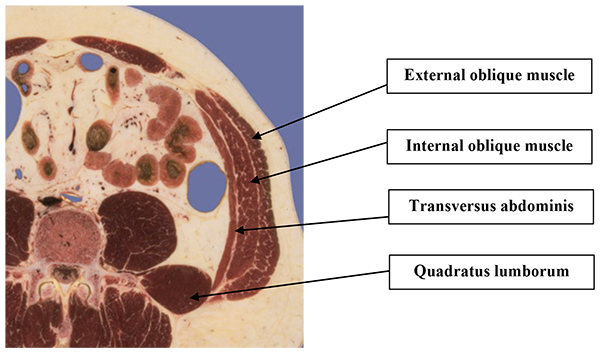
Figure 1: Cross section though the abdomen. The 3 muscle layers of the lateral / anterior abdominal wall can be seen.
Sensory Supply of the Abdominal Wall
The lower 6 thoracic nerves and the first lumbar nerve supply sensation to the abdominal wall (Fig 2).
Thoracic Nerves T6 – T11
The anterior divisions of nerves from T6 – T11 travel along their relevant intercostal space, before passing under the costal cartilages where they enter into the fascial plane between transversus abdominis muscle and internal oblique muscle. The nerves continue on to pierce the rectus abdominis muscle terminating as the anterior cutaneous branches supplying sensation to the skin of the anterior abdomen. About half way along their course the thoracic nerves give off lateral cutaneous branches, which travel posteriorly, piercing the external oblique muscle to supply sensation to the skin of the lateral abdomen and back.
Thoracic Nerve 12
The anterior division of the nerve from T12 is a large nerve. It runs anteriorly along the inferior border of the 12th nerve and then passes under the lumbocostal arch to run along with the other lower intercostal nerves between the transversus abdominis muscle and the external oblique muscle. The T12 nerve gives a communicating branch to the L1 nerve as part of the upper part of the lumbar plexus. The lateral cutaneous branch of T12 supplies the skin over the upper gluteal region.
The Ilioinguinal and Iliohypogastric Nerves (T12 / L1)
The Iliohypogastric and Ilioinguinal nerves of the lumbar plexus both enter the transverse abdominis plane near to the iliac crest. The Iliohypogastric nerve divides into an anterior cutaneous branch, supplying the skin over the hypogastrium, and a lateral cutaneous branch supplying skin over the gluteal region. The Ilioinguinal nerve travels within the inguinal canal and supplies sensation to the skin of the upper thigh, base of penis and scrotum.
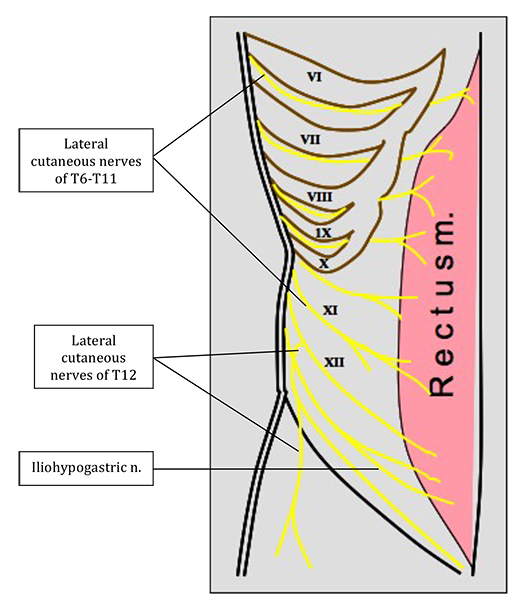
Figure 2: Nerve supply to the anterior abdominal wall. Each Roman numeral indicates the thoracic nerve seen below it.
INDICATIONS FOR TAP BLOCK
The TAP block can be used as part of an analgesic regimen for abdominal surgery. Initial studies were able to demonstrate blocks extending from T7-L1 using bilateral injections[4]. Subsequent studies have been unable to reproduce these findings with most studies achieving uppermost sensory levels around T9/10. This lower block is supported by findings in a cadaveric study, looking at spread of local anaesthetic after a single posterior TAP injection[5]. It therefore sensible to recommend that the TAP block can only reliably be used for analgesia in surgery on the lower abdomen, for example:
- Hernia repair
- Open appendicectomy
- Caesarian section
- Total abdominal hysterectomy
- Radical prostatectomy
A subcostal TAP block has been described in addition to the posterior TAP injection. This can be performed to provide analgesia for abdominal surgery extending above the umbilicus[6].
For a comprehensive review of the evidence for the use of the TAP block please refer to an article published in ‘Update in Anaesthesia’. The article gives an in-depth description of the results of recent studies[7].
CONTRAINDICATIONS TO TAP BLOCK
Absolute
- Patient refusal
- Allergy to local anaesthetic
- Localised infection over injection point
Relative
- Coagulopathy
- Surgery at injection site
COMPLICATIONS
The TAP block is a relatively safe technique with only a few case reports of significant complications. Complications reported include:
- Failure
- Local anaesthetic toxicity
- Intraperitoneal injection
- Bowel injury
- Hepatic injury
TECHNIQUES
The aim of the TAP block is to deposit a large volume of local anaesthetic into the transversus abdominis plane with at least 20 ml of solution being for used each side. The concentration of solution used will depend on the calculated maximum dose of local anaesthetic allowed. There are both landmark and ultrasound guided techniques to the TAP block and we will describe each below.
General Preparation
You will need:
- Full resuscitation equipment
- Patient monitoring (ECG, pulse oximeter, BP)
- Antiseptic skin preparation and sterile gloves
- Short bevel (30° ) block needle (50 – 100 mm), or 16-G Tuohy needle, with an extension set
- 20 ml syringes
- Local anaesthetic – a long acting local anaesthetic (Levobupivacaine, Ropivacaine) should be used in the majority of cases. 0.3-0.6 ml/kg per side can be used as to a guide for volume calculation.
The blocks can be performed awake but are most commonly performed with the patient under general anaesthetic.
Landmark Technique
The landmark technique, described by McDonnell et al, accesses the transversus abdominis plane via the lumbar triangle of petit. This is a surface landmark bound by the external oblique muscle anteriorly, the latissimus dorsi muscle posteriorly and the iliac crest inferiorly (Fig 3).
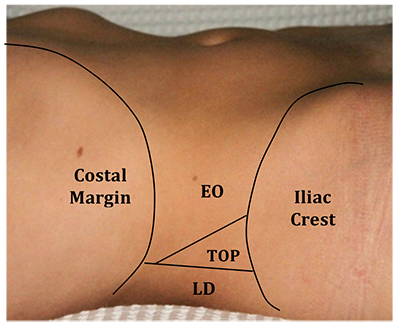
Figure 3: Landmarks outlining the Triangle of Petit (EO, external oblique muscle; TOP, triangle of petit; LD, latissimus dorsi muscle).
The Block
- Identify the triangle of petit using the anatomical landmarks described above. A depression can sometimes be palpated between the posterior border of the external oblique muscle and the anterior border of the latissimus dorsi muscle. As a guide this normally found in the region of the posterior axillary line, directly above the iliac crest.
- Insert the short bevel regional block needle perpendicular to the skin. A Tuohy needle can also be used.
- After piercing the skin, the needle is advanced until a ‘pop’ is felt – this is the needle piercing the fascial extension of the external oblique muscle. The needle should be advanced until a second ’pop’ is felt, as the needle passes through the fascial extension of the internal oblique muscle. A loss of resistance technique can also be combined with this ‘fascial click’ technique to satisfy theoperator that the fascia has been breached. The needle should now lie superficial to the transversus abdominis muscle, in the transversus abdominis plane (Fig 4).
- After aspiration, to exclude malposition of the needle tip, the local anaesthetic is injected. A minimum of 20 ml of local anaesthetic per side should be used.
- Be careful not to exceed the maximum safe dose of local anaesthetic
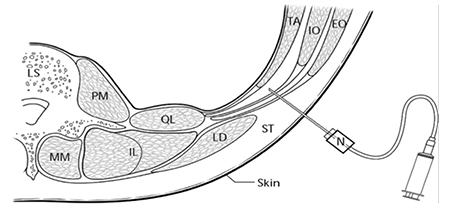
Figure 4: Diagram of transverse section of abdominal wall during landmark TAP block performance (N, needle; ST, subcutaneous tissue; EO, external oblique muscle; IO, internal oblique; TA, transversus abdominis; LD latissumis dorsi; QL, quadratus lumborum)
Ultrasound Guided Technique
We will discuss first the technique for the ultrasound guided posterior TAP block, which can be reliably used for lower abdominal incisions. We will then describe the subcostal modification to achieve analgesia for the upper abdomen.
This technique is more time-consuming than the landmark approach, due to preparation of ultrasound equipment. However it can be recommended due to the benefit of viewing the needle during insertion, therefore ensuring that the needle is placed correctly and that no other structures are injured. It must be emphasised that the needle should be continuously seen during insertion.
Preparation
- As for the landmark technique
- Ultrasound machine
- High frequency (6-13MHz) linear array probe with probe cover and sterile gel.
- The use of vascular access probes (e.g. Sonosite iLook) for this block cannot be recommended unless already proficient in ultrasound-guided regional anaesthesia. Intra-abdominal injury has resulted from inadequate needle visualisation with this equipment.
- An assistant to perform injection of the local anaesthetic (optional)
The Block (Posterior Injection)
- The ultrasound transducer is positioned horizontally across the abdomen
- The muscle layers in the antero-lateral part of the abdomen can be traced by scanning from the midline towards the area between the iliac crest and the costal margin, in the mid-axillary line.
- The rectus abdominis muscle is identified, just off the midline, as an oval / elliptical structure.
- As you scan laterally the rectus abdominis abuts a fascial plane (linea semilunaris). This fascial plane then gives rise to 3 muscle layers: external oblique, internal oblique and transversus abdominis (Fig 5)
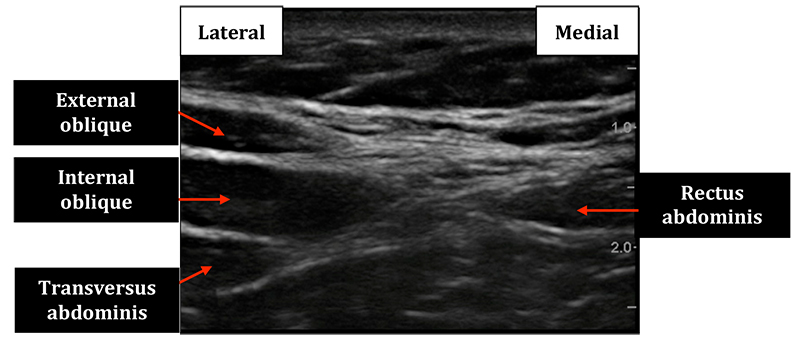
Figure 5: Ultrasound image of the view if probe is place adjacent to the midline to visualise the rectus abdominis muscle medially and the origins of the external oblique, internal oblique and transversus abdominis muscles laterally.
- The ultrasound transducer is moved to scan laterally where the 3 muscle layers can be seen running parallel to one another (Fig 6)
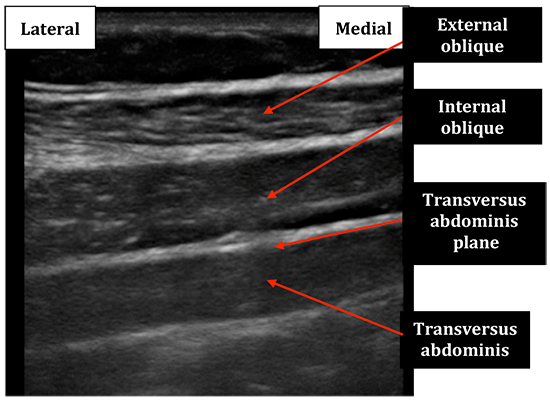
Figure 6: Ultrasound image obtained as the probe is moved laterally away from the midline
- The ultrasound transducer is moved more posteriorly, aiming to view the point where the transversus abdominis muscle begins to tail off. With an adequate ultrasound image, the regional block needle is inserted anterior to the transducer. This allows an in plane view of the needle as you pierce the transversus abdominis plane (Fig 7 & 8)
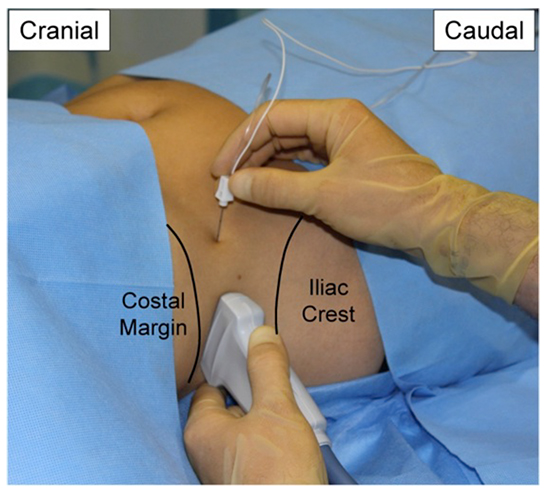
Figure 7: Picture showing the ultrasound transducer position and in-plane needle technique for the posterior TAP block on the right side of the patient.
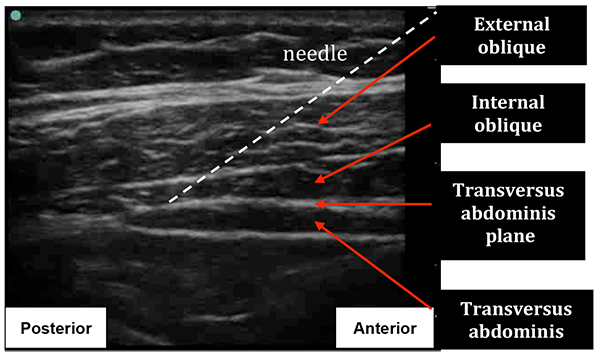
Figure 8: Ultrasound image during posterior TAP Block. The transversus abdominis muscle can be seen to taper into a fascial line. The approximate needle insertion angle is indicated.
- The local anaesthetic is then slowly injected. If the needle is correctly positioned, the fascial plane is seen to separate and form a well-defined, hypoechoic, elliptical shape between the internal oblique and transversus abdominis muscles.
- It is essential to watch for the spread of local anaesthetic. If a patchy opacity appears within the muscle either superficial or deep to the transversus abdominis plane, then the needle should be repositioned until local is seen to spread within the plane, separating the fascia between the muscles. Obviously if no local is seen to appear – stop; the needle tip may not be where you think it is, or the local is being injected into a vessel or the peritoneal cavity (Fig 9).
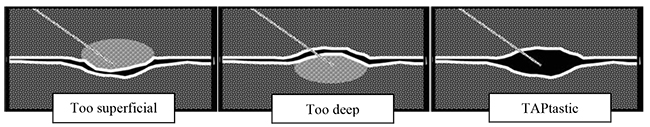
Figure 9: Figure highlighting the optimal needle position during ultrasound-guided TAP block.
The Block (Subcostal Injection)
- This should be performed if analgesia of the abdominal wall above the umbilicus is required. It will provide analgesia for areas of the upper abdomen that are not usually adequately covered by the landmark or posterior TAP approaches.
- The ultrasound transducer should be placed under the costal margin, close to the midline, and the upper portion of the rectus muscle identified. In the midline of the subcostal region the transversus abdominis muscle can be seen deep to the rectus abdominis muscle, unlike near the umbilicus where it is seen only lateral to the rectus muscle. (Fig 10 & 11).
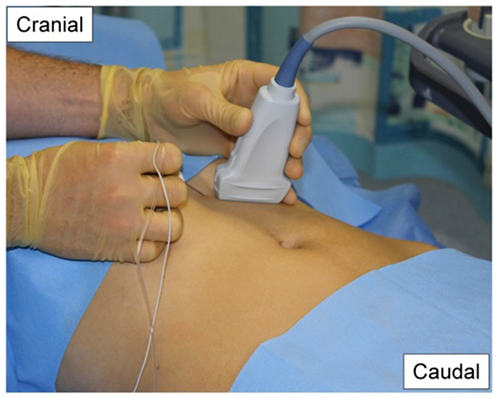
Figure 10: Picture showing the ultrasound transducer position and in-plane needle technique for the oblique subcostal TAP block on the left side of the patient.
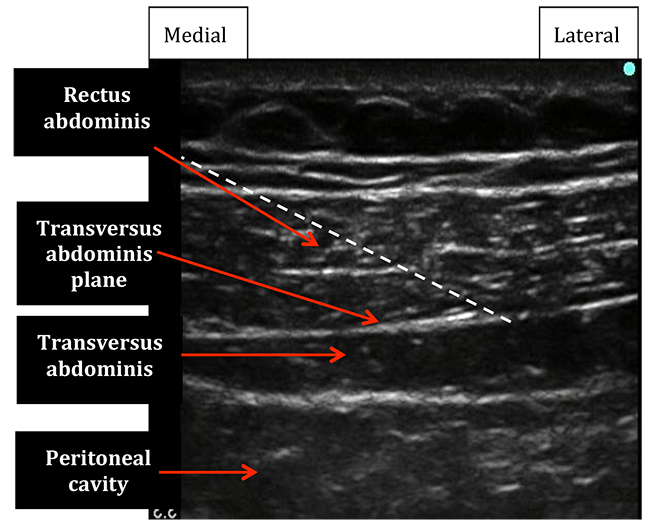
Figure 11: Ultrasound image of rectus abdominis and transversus abdominis muscles immediately adjacent to the midline. Dotted white line indicates the desired needle position.
- Insert the needle at the medial end of the transducer to obtain an in-plane view. Use a long regional block needle for a single-shot technique or a Tuohy needle if a catheter is to be placed as for a continuous technique.
- Once the tip of the needle is placed between the posterior rectus sheath and superficial borderof transversus abdominis, inject a small amount of local anaesthetic (after aspiration). The needle should then be cautiously advanced into the space created by the local anaesthetic.
- Further injection and needle advancement should continue following along an oblique line from the xiphoid process towards the anterior part of the iliac crest. As you scan along this line you reach the lateral border of rectus abdomins. Here you find the origin of the internal and external oblique muscles. The transversus abdominis muscle continues to run deep to the IO muscle. (Fig 12 and Fig 13)
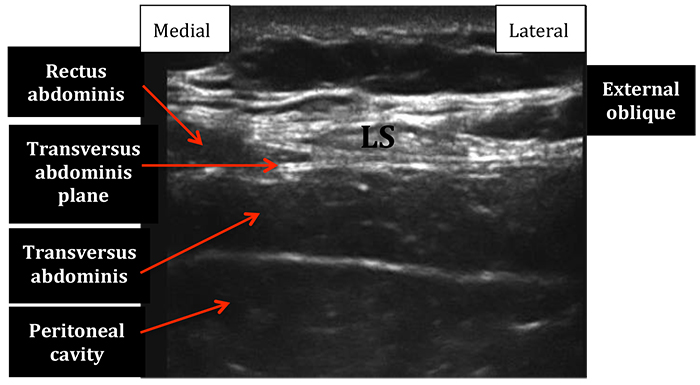
Figure 12: Ultrasound image of the subcostal transversus abdominis plane as you scan laterally from the midline along an oblique line form the xiphoid process towards the anterior superior iliac spine. Note the lateral border of rectus abdominis and the origin of external oblique muscle. LS=linea semilunaris.
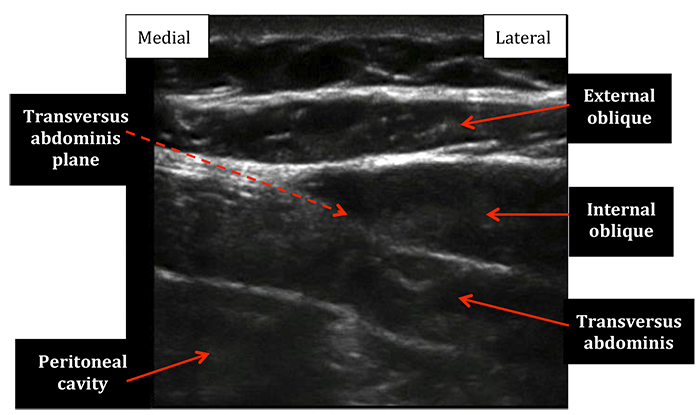
Figure 13: Ultrasound image of the lateral subcostal transversus abdominis abdominis plane as the ultrasound probe continues further toward the ASIS. Note the continuation of transversus abdominis muscle and the origins of external and internal oblique muscles.
- Up to 20mls of local anaesthetic may be needed to fill the TA plane along this oblique subcostal line. Some recommend using higher volumes of more dilute local anaesthetic.
- It should be said that this is an advanced level block, as significant needle-guidance skills are required to safely perform this block.
IMPORTANT POINTS
- TAP blocks are adjunctive techniques for analgesia. They do not adequately provide anaesthesia for surgery as it provides no visceral anaesthesia or analgesia.
- Landmark and Posterior USG TAP blocks, if performed correctly, will reliably provide analgesia for operations at or below the umbilicus.
- Oblique Subcostal TAP blocks can be considered for areas above the umbilicus.
- These are fascial plane techniques, and rely on the deposition of large volumes of local anaesthetic to anaesthetise multiple small abdominal wall nerves.
Maximum local anaesthetic doses must be calculated to avoid the effects of systemic toxicity.
ANSWERS TO QUESTIONS
-
- F The nerve supply originates from the anterior primary rami of T7-T12
- F The muscles of the lateral abdominal wall are: external oblique, internal oblique and transversus abdominis
- T
- T
- F The lumbar triangle of petit lies posterior to the mid axillary line
-
- F TAP block reliably provides analgesia for operations at or below the umbilicus (T10 – L1)
- F TAP block is best performed using a high volume technique. The concentration should be guided by the maximum calculated dose for the patients weight
- T
- F The TAP block provides analgesia to the abdominal wall but provides no visceral analgesia. It should be used in combination with an oral or intravenous analgesia
- F The TAP block can be used for unilateral procedures e.g. appendicectomy / inguinal hernia repair
-
- F The rectus abdominis muscle is best viewed close to the midline of the abdomen. The transversus abdominis plane can be traced from its’ insertion to the linea alba (lateral to rectus abdominis) and is best viewed in the lateral part of the abdomen.
- T
- F Observing the spread of local anaesthetic is key to ensuring you are in the transversus abdominis plane. It is important to identify if your needle is intramuscular and reposition your needle as necessary
- T
- F A posterior TAP block will reliably provide analgesia to dermatomes T9/10 – L1. Some studies have reported higher blocks, upto T7[4], from a single posterior injection. However, consideration should be given to a second injection using the oblique subcostal technique if analgesia is required for the upper abdomen.
REFERENCES and FURTHER READING
- AN Rafi, Abdominal Field Block: a New Approach Via The Lumbar Triangle; Anaesthesia; 2001; 56:1024-6
- JG McDonnell, BD O’Donnell, D Tuite, T Farrell, C Power, The Regional Abdominal Field Infiltration Technique Computerised Tomographic and Anatomical Identification of a Novel Approach to the Transversus Abdominis Neuro-Vascular Fascial Plane; Anaesthesiology; 2004; 101: A899
- P Hebbard, Y Fujiwara, Y Shibata, C Royse. Ultrasound Guided Transversus Abdominis Plane Block. Anaesthesia & Intensive Care; 2007; 35(4): 616-7
- JG McDonnell, B O’Donnell, G Curley, A Heffernan, C Power, JG Laffey. The analgesic Effect of Transversus Abdominis Plane Block After Abdominal Surgery. Anaesthetsia & Analgesia; 2007; 104(1): 193-7
- TMN Tran, JJ Ivanusic, P Hebbard, MJ Barrington. Determination of Spread of Injectate After Ultrasound Guided Transversus Abdominis Plane Block: A Cadaveric Study. British Journal of Anaesthesia; 2009; 102(1): 123-7.
- P Hebbard, M Barrington, C Vasey. Ultrasound-Guided Continuous Oblique Subcostal Transversus Abdominis Plane Block. Regional Anesthesia & Pain Medicine; 2010; 35(5): 436-41
- K Webster. The Transervsus Abdominis Plane (TAP) block: Abdominal plane regional anaesthesia. Update in Anaesthesia; 2008; 24(1): 25-30. http://update.anaesthesiologists.org/wp- content/uploads/2009/10/Transversus-Abdominis-Plane-TAP-Block.pdf
The anatomy section was written with help from Gray’s Anatomy: The Anatomical Basis of Clinical Practice, 40th edition (2008), 1576 pages, Churchill-Livingstone, Elsevier. ISBN 978-0-443-06684-9
SOURCES of IMAGES
Figure 1 – Regional Anatomy Atlas Viewer. Robert Livingston. March 2010 (RAA Viewer is a free resource and may be freely distributed for non-commercial use) Other images provided by Authors



