Regional Anaesthesia
LEARNING OBJECTIVES
- To understand the anatomy and innervation of the femoral nerve.
- To understand and recognise the sono-anatomical structures of the region and how these affect the practical conduct of the block.
- To be aware of alternative regional anaesthetic techniques.
- Describe the practical steps to perform an ultrasound guided femoral nerve block.
- To gain an understanding of both in-plane and out of plane approaches and catheter techniques.
QUESTIONS
Before continuing, try to answer the following questions.
- Which of the following statements regarding the femoral nerve are true?
a) It always supplies sensation over the lateral aspect of the thigh
b) It is arises from nerve roots L1 – L3
c) It forms from the lumbar plexus within the psoas muscle
d) Its terminal branch supplies cutaneous sensation to the lateral side of the leg - What structures lie immediately to the femoral nerve in the femoral triangle?
a) superior
b) medial
c) inferior - The following statements are true regarding an ultrasound guided femoral nerve block
a) It is a deep block requiring a low frequency probe
b) An out of plane needle approach is the standard approach
c) It is easy to visualise with ultrasound throughout the thigh
d) It is a useful for analgesia to the knee joint
INTRODUCTION
A femoral nerve block (FNB) is a useful and commonly undertaken regional anaesthetic block. This article describes ultrasound-guided approaches to this block. It is considered a basic level block as it is relatively superficial, easy to identify and the potential for complications is low.
A femoral nerve block will provide analgesia for surgical procedures involving the anterior thigh and the hip and knee joints (depending upon type of surgery additional nerves blocks may be required e.g. posterior elements of the knee may require a sciatic nerve block) and by blocking it’s terminal cutaneous branch, the saphenous nerve, superficial analgesia to a variable area of the medial aspect of the leg.
ANATOMY OF THE REGION
An ultrasound-guided femoral nerve block is usually performed just below the inguinal crease. Superficial to the femoral nerve are the skin, subcutaneous tissue, the fascia lata (a thin medial continuation of the iliotibial tract) and the fascia iliaca which covers the iliopsoas muscle and appears as a curved hyper-echoic line on ultrasound blending into the femoral sheath.
Lateral and anteriorly is the belly of sartorius. Medially is the femoral artery and vein enclosed in their femoral sheath and then more medially lymphatic tissues and the pectineus muscle. The femoral nerve is outside of the femoral sheath. See Figures 1 and 2.
The femoral artery gives of several important branches in this region – the large profunda femoris artery that comes off postero-laterally approximately 4 cms below the inguinal ligament and the lateral femoral circumflex artery that arises from either the femoral or profunda femoral artery and can run laterally between the branches of the femoral nerve. Care must be taken to avoid these vessels when performing this block.
The femoral vein and profunda femoris vein are usually medial and inferior to the artery and can be easily compressed with probe pressure. It would seem sensible to ease probe pressure to confirm their positions prior to performing the block.
COURSE AND INNERVATION
The femoral nerve originates from the lumbar plexus, which forms within, the body of the psoas muscle. The femoral nerve is derived from the anterior rami of nerve roots of L2 to L4. It emerges from below the lower lateral border of the psoas to enter the anterior thigh underneath the inguinal ligament, where it divides into anterior and posterior divisions. It then rapidly divides into separate elements making it more difficult to visualise distally using ultrasound. See Table 1.
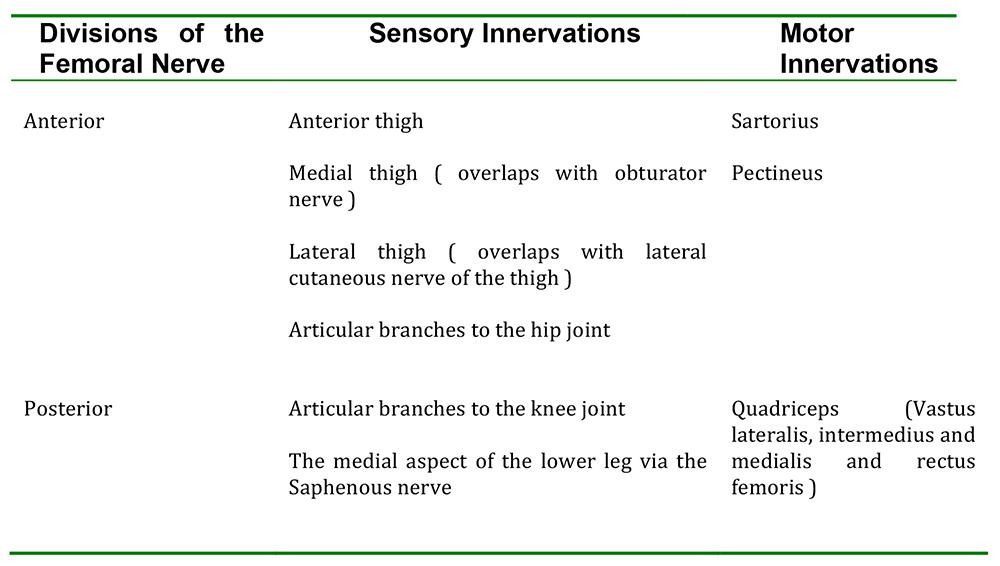
Table 1. Innervations of the Divisions of the Femoral Nerve.
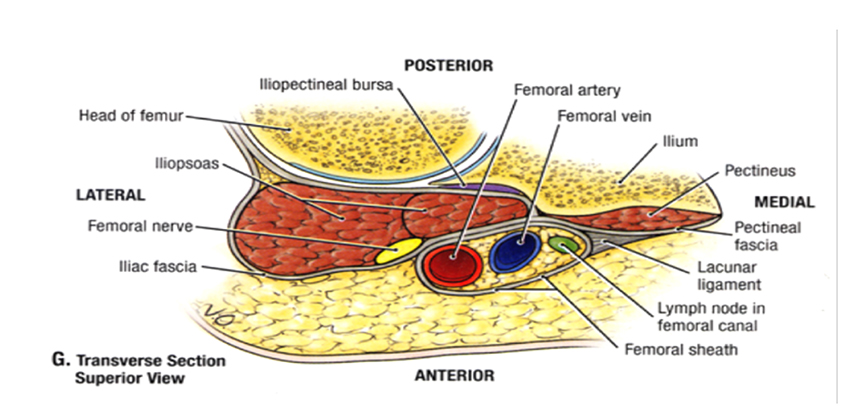
Figure 1: Cross section of femoral region (Grants Atlas of Anatomy 11th edition)
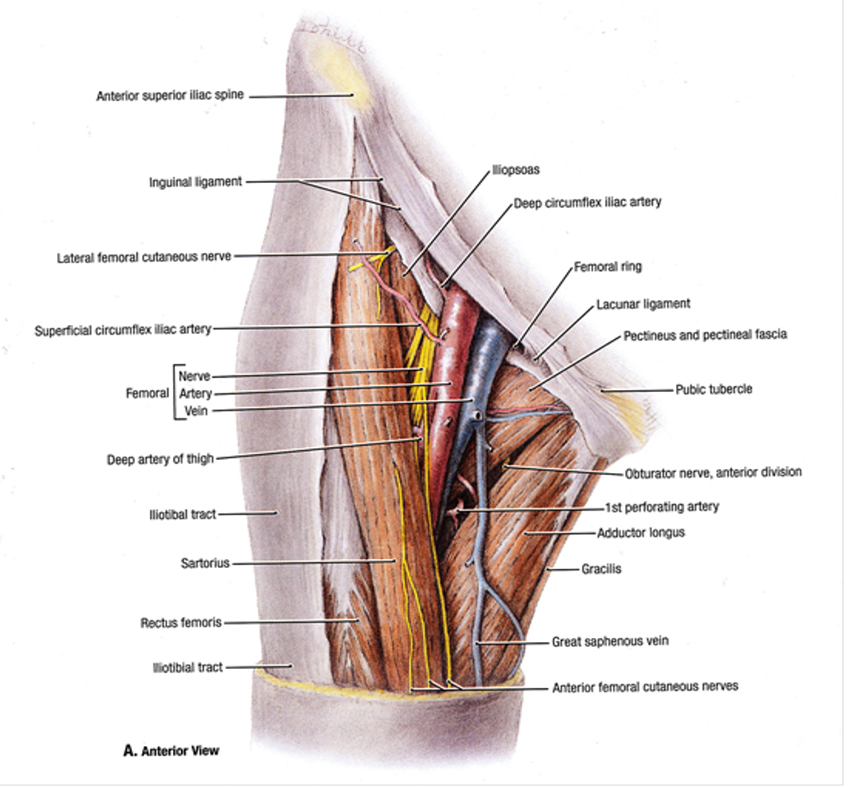
Figure 2: View of anterior thigh (Grants Atlas of Anatomy 11th edition)
SONO CHARACTERISTICS
The nerve usually has a triangular or flattened oval shaped speckled hyperechoic appearance and becomes less obvious as it quickly fans out into branches caudally. See Figures 3 and 4. It can often be situated quite lateral to the femoral artery. See Figures 5 and 6.
It is fairly superficial (usually < 3 cms from the skin). Despite it being a large nerve it can sometimes be surprisingly difficult to discern – look for easy to identify ‘signposts’ such as femoral artery and fascia iliaca to help to locate the nerve. Follow up and down the course of what appears to be the nerve utilising PART manoeuvres (Pressure, Alignment, Rotation and Tilt) to confirm. Note where the femoral artery divides and aim to perform the block prior to the division. See Figures 7 and 8.
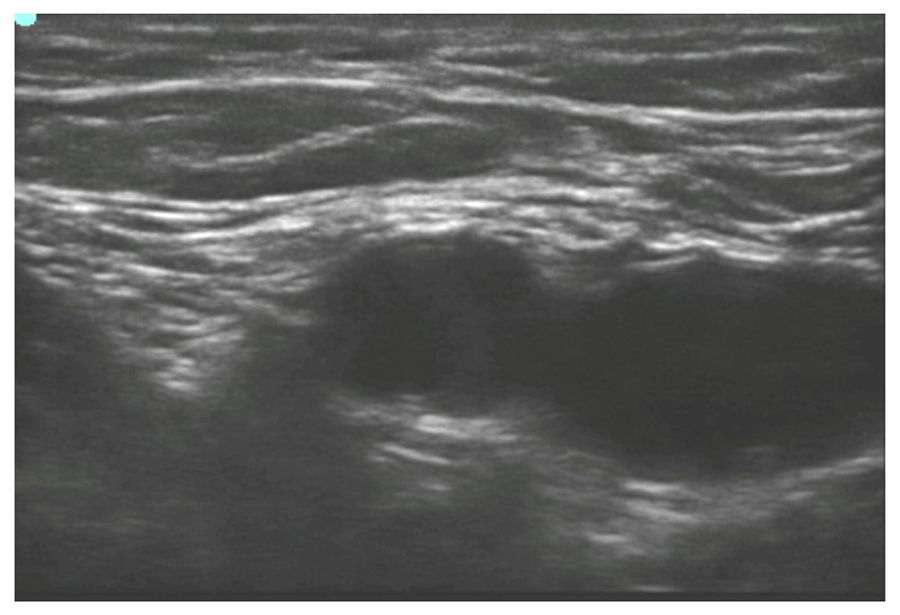
Figure 3: Ultrasound image of the Left femoral region. Left side image lateral, right side medial.
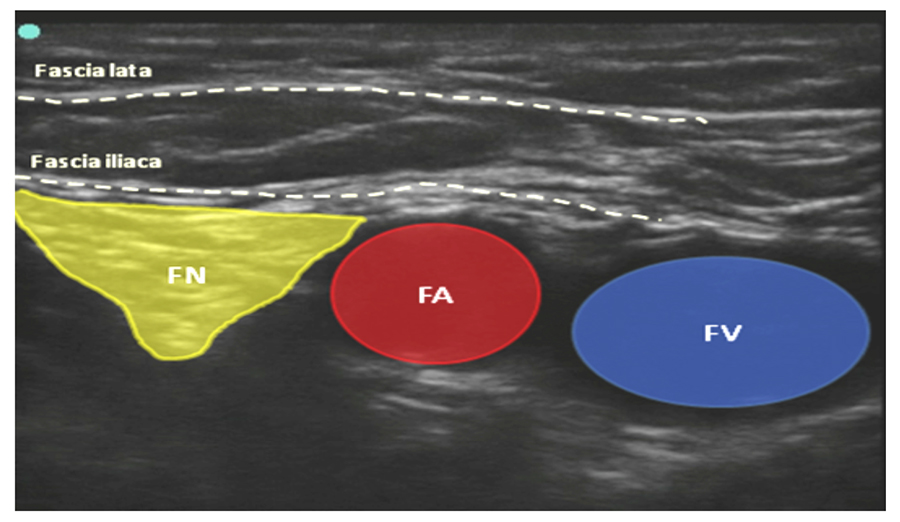
Figure 4: The image 3 showing with the Femoral Vein (blue), Femoral Nerve (yellow) and Femoral Artery (red circle) outlined. Left side image lateral, right side medial.
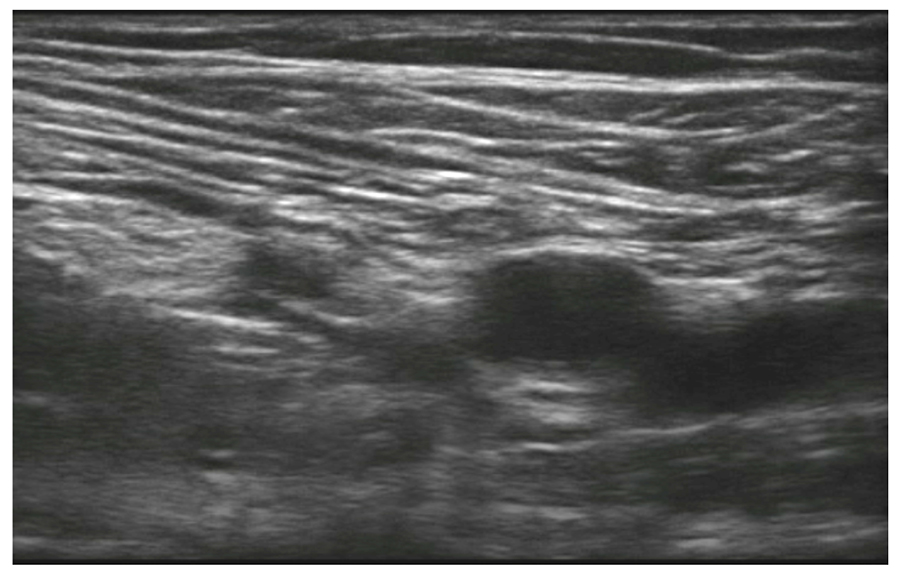
Figure 5: Femoral Nerve lying further lateral to artery Left side image lateral, right side medial.
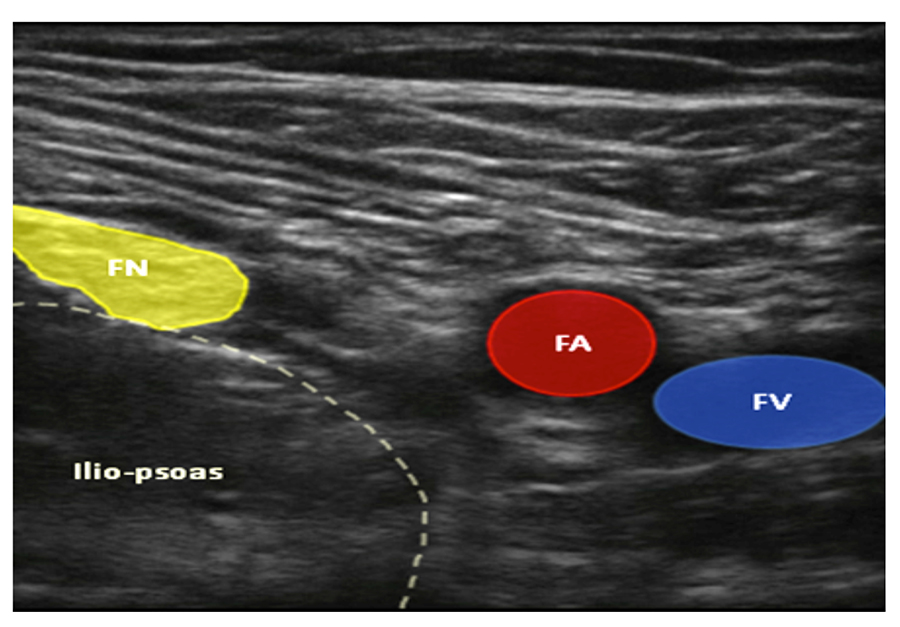
Figure 6: The image 5 highlighted with the Femoral Vein (Blue), Femoral Artery (Red), Femoral Nerve (Yellow) Left side image lateral, right side medial.
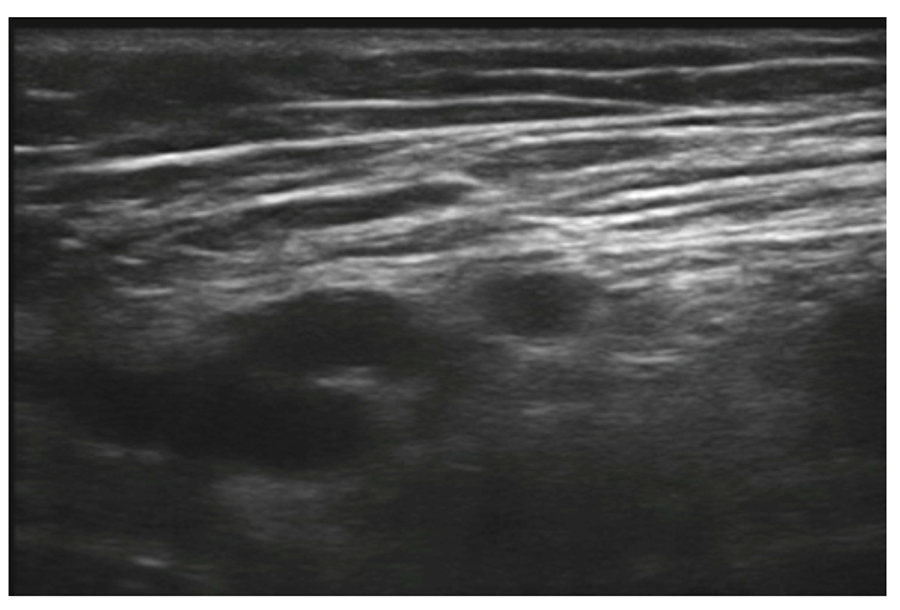
Figure 7: Slightly more caudally the profunda femoral and lateral femoral circumflex artery comes into view. Right side image lateral, left side medial.
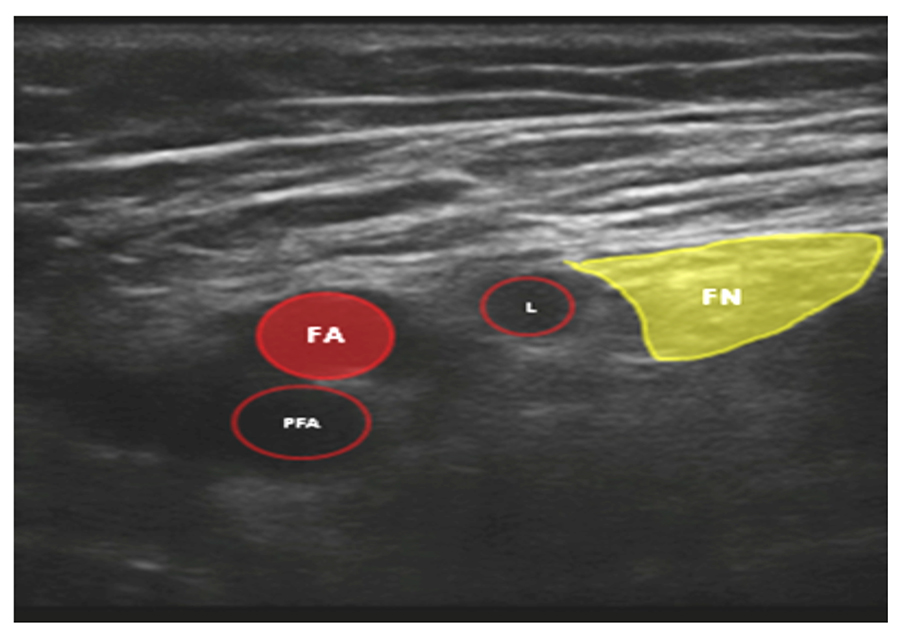
Figure 8: Figure 7 with femoral artery (FA), profunda femoral (PFA) and lateral femoral circumflex (L) artery in relation to femoral nerve. Right side image lateral, left side medial.
ALTERNATIVES
Anaesthesia and or analgesia for the areas covered by the femoral nerve can also be obtained by alternative techniques such as spinal, epidural, psoas compartment / lumbar plexus and fascia iliaca blocks.
Descriptions of fascia ilaica and lumbar plexus blocks can be found in ATOTWs 193 and 263 respectively.
PRACTICAL CONDUCT OF THE BLOCK
As with all regional techniques informed consent should be obtained and appropriate intravenous access, monitoring instituted. The procedure should be undertaken in aseptic conditions with a trained assistant available. This block can be performed in an awake patient with very little discomfort.
- Place yourself on the side to be blocked with the ultrasound machine across the other side of the supine patient. See Figure 9.

Figure 9: Relative position of the operator, patient and ultrasound machine to perform a femoral nerve block.
- The leg should be in a neutral position, slightly abducted or laterally rotated up to 150. The position of the leg is not critical for example if the patient has a fracture accepting a leg position that is most comfortable for the patient is a reasonable approach.
- Place a linear probe (such as 6 – 13 MHz) along the line of the inguinal crease.
- Initially search for the most easily visible structures such as the femoral artery and fascia iliaca.
- Then travel systematically with the probe in both superior-inferior and medio-lateral directions to identify all relevant structures and their relationships.
- The nerve, seen in cross section (short axis view [SAX]), usually appears as a hyperechoic speckled triangular or oval shaped structure just lateral to the artery, although it can occasionally appear thin or flattened or may be distant to the artery. Adjustments using alignment, tilt and rotation may be required to optimise the view of this nerve.
- Use colour flow Doppler to identify vessels and compression to help differentiate arteries and veins.
- The authors favour an in line, lateral to medial approach. This approach has the advantage of being able to see the length of the needle throughout needle advancement and as the nerve is lateral to other ‘hazards’ it can usually be reached without inadvertent vascular puncture. The disadvantages are: a longer course through the tissues and it less convenient for threading a catheter. Also it is better to block the femoral nerve higher up in the groin before the artery divides in order to block both the anterior and posterior division of the femoral nerve.
- Enter the skin on the lateral side of the probe (after local infiltration) using a long needle (up to 100mm) piercing through the sartorius muscle the fascia lata and fascia iliaca.
- When the tip of the needle is visualised next to the nerve aspirate to check for intravascular puncture. Needle tip preferably inferiorly to the nerve so that the local anaesthetics may elevate the nerve and separate it from the artery rather than push it away
- Inject a total of 10 – 30mls of local anaesthetic in small aliquots aspirating every 5mls or so, observing both the image of local anaesthetic spread and the patient for signs of discomfort or toxicity. If there is any pain on injection stop immediately as the needle may be intraneural.
- Spread should be directly visualised below the fascia iliaca and ideally surrounding, isolating and highlighting the nerve (the ‘doughnut’ sign). See Figures 10 and 11.The appearance of local anaesthetic above the nerve only may indicate deposition above the fascia iliaca and result in inadequate analgesia.

Figure 10: Femoral nerve with doughnut sign appearing during the injection of local anaesthetic. IP view of needle seen on right side of image. Right side image lateral, left side medial.
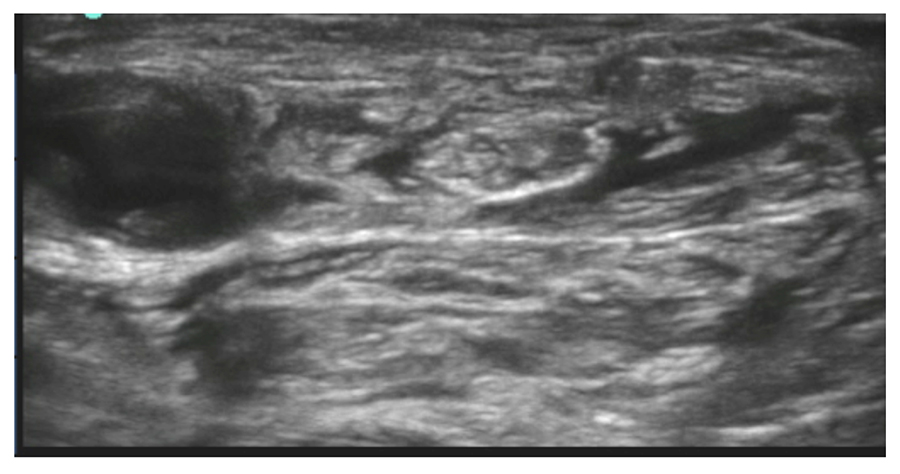
Figure 11: Femoral nerve with doughnut sign outlined after the injection of local anaesthetic. Right side image lateral, left side medial.
- Separation of bundles within the nerve may indicate intraneural injection and should be avoided, as should high pressure or resistance on injection. In Figure 10 the needle is now anterior to (not within) the nerve, having already deposited local anaesthetic posterior to the nerve.
- Scan up and down the thigh to view the extent of the local anaesthetic spread and nerve envelopment.
OUT OF PLANE AND LONG AXIS VIEW
An out of plane (OOP) approach (where the needle approaches perpendicular to the probe and beam) can also be used and has the distinct advantages of a shorter tissue transit plus ease of catheter insertion. As with any OOP approach visualising the tip of the needle can be problematic and one may mistake an image of the shaft for the tip, underestimating how far the tip has advanced. To avoid this, as you advance the needle from a caudal direction (below the inguinal ligament), sequentially adjust the tilt of the probe ahead of the advancing tip to visualise it as passes into the path of the ultrasound beam. The block and catheter insertion can also be done using a long axis view (LAX) of the nerve2. Where the probe is placed parallel to the length of the nerve rather than perpendicular to it as in the more conventional short axis view.
PERIPHERAL NERVE STIMULATOR
Using a peripheral nerve stimulator may assist in confirming the structure as the femoral nerve but has the distinct disadvantages of causing muscle contraction, making viewing the image difficult and possibly causing discomfort. It does not appear to improve success rates compared with ultrasound alone.3 As with the non ultra-sound technique a ‘dancing patella’ should be the sought end point (rather than twitch of sartorius).
IMPORTANT POINTS
- Femoral nerve block can provide analgesia for surgical procedures involving the anterior thigh and the hip and knee joints.
- Ultrasound guidance has the potential to make the block more reliable and safer.
- It is useful to see the relation of femoral nerve to its vessels.
- The needle tip should always be seen throughout the procedure to ensure its location and to avoid intraneural or intravascular injection.
ANSWERS TO QUESTIONS
- Regarding the femoral nerve
a) False – the lateral cutaneous nerve of the thigh (LCNT) usually provides sensation to this area
b) False – usually the nerve arises from L 2 – L4 nerve roots, although this is not always the case and contributions can be seen from L1 and L5
c) True – it is one of the terminal nerves of the lumbar plexus – which also includes LCNT ,
obturator , ilio-hypogastric and ilio-inguinal nerves
d) False – the terminal branch is the saphenous nerve which provides cutaneous sensation to a
variable area on the medial side of the leg down to the first meta tarsal phalangeal joint - Structures adjacent to the femoral nerve
a) The fascia iliaca
b) The femoral artery
c) The ilio-psoas muscle - Regarding an ultrasound guided femoral nerve block
a) False – it is relatively shallow and a higher frequency probe is usually used
b) False – either an in plane ( IP ) or out of plane ( OOP ) approach can be used
c) False – below the inguinal ligament it quickly separates and becomes more difficult to visualise
d) True – it is a major contributor of sensation to the knee joint and blocking it will provide useful analgesia for knee surgery.
REFERENCES
- Dalens B. Anaesth Analg 1989; 69:705-713.
- Wang, Ai-Zhong MD; Gu, LingLing MSc ; Zhou, Quan-Hong MSc ; Ni, Wen-Zong MSc ; Jiang, Wei MD . Ultrasound-Guided Continuous Femoral Nerve Block for Analgesia after Total Knee Arthroplasty: Catheter Perpendicular to the Nerve Versus Catheter Parallel to the Nerve Regional Anesthesia & Pain Medicine: March/April 2010 – Volume 35 – Issue 2 – pp127-131.
- Sites B, Beach M L, Chinn C et al. A comparison of sensory and motor loss after a femoral nerve block conducted with ultrasound versus ultrasound and nerve stimulation. Reg Anesth Pain Med 2009; 34:508-513.
Sources of Figures:
- Figure 1, 2: Grants Atlas of Anatomy 11th edition
- Figure 3 – 11: Author’s personal archive



