Regional Anaesthesia
KEY POINTS
- Similar to traditional interscalene block (ISB), superior trunk block (STB) is generally used for shoulder and/or proximal humerus analgesia and anaesthesia.
- STB has approximately equal analgesic potency and distribution as ISB, with the advantage of greater sparing of the phrenic nerve.
- The incidence of phrenic nerve palsy following STB is ~5% compared with .70% after ISB when both blocks are performed with the same volume (15 mL) of either bupivacaine 0.5% or ropivacaine 0.5%.
- STB should be performed proximal to the takeoff of the suprascapular nerve to ensure adequate sensory coverage of the shoulder.
- A supplemental injection over the middle scalene muscle, on the way out with the block needle, anaesthetising the supraclavicular nerve branches (targeting primarily the lateral and intermediate supraclavicular nerves) is recommended to improve analgesia of the shoulder cape.
- Adequate knowledge of STB-related sonoanatomy is paramount. Practitioners must identify the transverse cervical and dorsal scapular arteries to prevent inadvertent vascular injury, intravascular injection and/or hematoma formation.
INTRODUCTION
The superior trunk block (STB) is a variation of the ultrasound-guided interscalene block (ISB), with similar sensory distribution, noninferior analgesia and significantly less phrenic nerve involvement.1–3 While the indications for STB are similar to ISB (namely, procedures involving the shoulder and/or proximal humerus), the injection site for ISB is in much closer proximity to the phrenic nerve, thus making it more likely for the local anaesthetic (LA) to diffuse toward it, resulting in (either partial or complete) phrenic nerve palsy. Accordingly, initial comparative studies have shown promising results with an incidence of complete inadvertent ipsilateral hemidiaphragmatic paralysis >70% following ISB compared with ~5% after STB.2,3 Caution, however, is advised while analysing these results, given the heterogeneity in study protocols for assessing diaphragmatic paralysis.
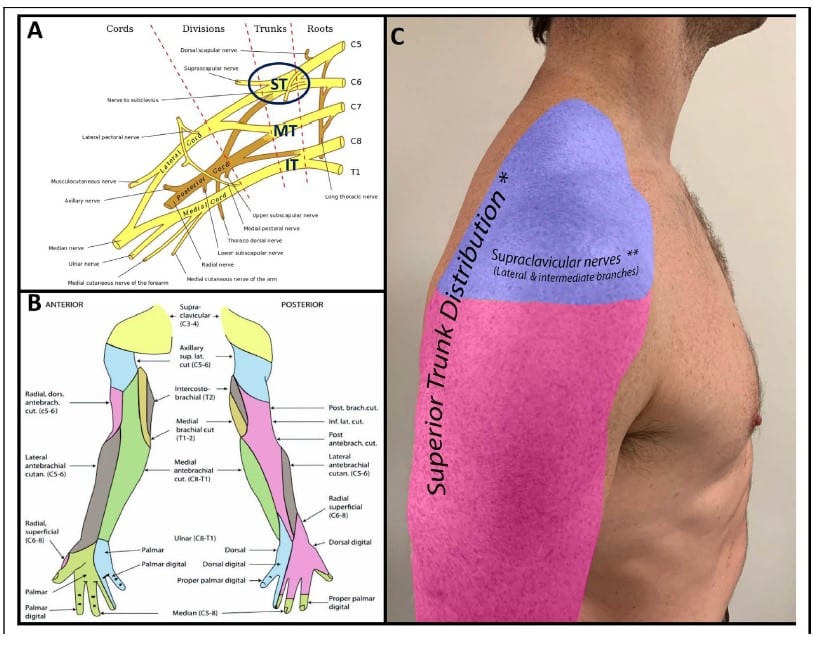
Figure 1. (A) Brachial plexus and its typical branching pattern. Source: Gray [public domain], Wikimedia Commons: https://upload.wikimedia.org/wikipedia/commons/0/0e/Brachial_plexus_2.svg. ST¼superior trunk; MT¼middle trunk; IT¼inferior trunk. (B) Sensory innervation of the upper extremity. Source: Henry Vandyke Carter [Public domain], Wikimedia Commons: https://upload.wikimedia.org/wikipedia/commons/d/de/ Gray812and814.PNG. (C) Sensory distribution of shoulder innervation. *Note the overlap between sensory innervation from the superior trunk and the supraclavicular nerves. **The technique of injecting local anesthetic over the middle scalene muscle targets primarily the lateral and intermediate supraclavicular nerves which provide sensory innervation to the shoulder cape. The medial branch may or may not be anesthetized and is not targeted for shoulder surgery given its sensory distribution involving the neck and medial aspect of upper chest. Source: Original Image.
SUPERIOR TRUNK
Anatomy
The brachial plexus is formed by the C5-T1 nerve roots and provides innervation for the upper extremity (Figure 1).
Brachial plexus branching as well as sensory and motor innervation are well described, allowing for the development of techniques to block specific points in the plexus to obtain desired patterns of anaesthesia/analgesia. Specifically, the shoulder and proximal humerus are supplied by branches originating from the C5 and C6 nerve roots, with the former also receiving sensory innervation from the supraclavicular (C3-C4) nerve (Figure 1).
When a linear, high-frequency ultrasound probe is placed transversally over the interscalene groove at the level of the C7 transverse process, the C5 and C6 nerve roots are generally visualised as a characteristic ‘stoplight sign’, with the lower 2 lights often representing the dual fascicles of the C6 nerve root (Figure 2A). This stoplight is the target for ISB. Distal to the stoplight, the C5 and C6 nerve roots converge to form the superior trunk (ST; Figure 2B-D), which is easily visualised under ultrasound due to its more prominent connective tissue sheath.1,4 The ST lies proximal to the clavicle and gives off an important sensory branch, the suprascapular nerve (SSN), which provides approximately 70% of the sensory innervation to the shoulder.5 Hence, identification and adequate coverage of the SSN is paramount to the successful performance of STB.
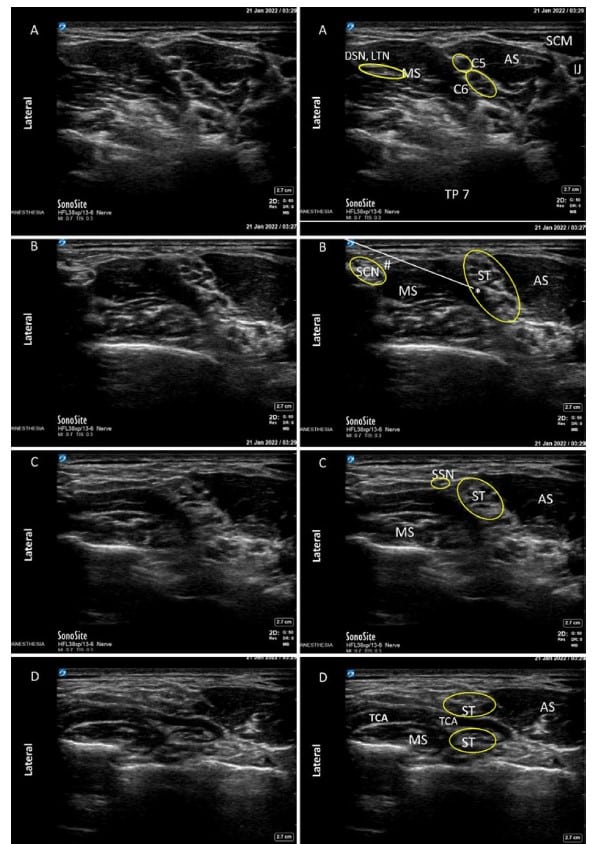
Figure 2. Side-by-side unlabelled and labelled ultrasound views from proximal to distal along the brachial plexus. (A) Brachial plexus at the interscalene block level. Note classic ‘‘stoplight sign’’. (B) Brachial plexus at the superior trunk block level. (C) Superior trunk view just distal to take-off of the suprascapular nerve. (D) Anatomical relationship between the transverse cervical artery and the superior trunk. Anatomical variations are relatively common with the transverse cervical artery lying over, under, or across (as shown in panel D) the superior trunk. Preprocedure identification of the transverse cervical artery is paramount to avoid inadvertent vascular trauma and/or hematoma formation during needle pass. ST ¼ Superior Trunk; SCN ¼ Supraclavicular nerve; SSN ¼ Suprascapular nerve; DSN ¼ Dorsal Scapular Nerve; LTN ¼ Long Thoracic Nerve; C5 ¼ C5 nerve root; C6 ¼ C6 nerve roots; TP7 ¼ Transverse process of C7; TCA ¼ Transverse cervical artery; IJ ¼ Internal jugular vein; SCM¼Sternocleidomastoid muscle; AS¼Anterior scalene muscle; MS¼Middle scalene muscle; (*)¼Injection point for superior trunk block; (#) ¼ Injection point for supraclavicular nerve block; White line ¼ needle trajectory (preferably pass over and depress rather than transect the middle scalene muscle); Yellow circles identify nerves and/or nerve groups. Source: Original Image.
Adjacent Structures
Following are structures adjacent to the ST:
- Phrenic nerve: This nerve originates from the C3-C5 nerve roots and provides motor innervation to the ipsilateral diaphragm.
- The phrenic nerve lies on the anterior surface of the anterior scalene muscle and is in much closer proximity to the brachial plexus at the level of ISB compared with STB.
- Subclavian nerve: In some individuals, the subclavian nerve gives rise to the accessory phrenic nerve, which can be unilateral or bilateral; however, its effect on diaphragmatic function is not well elucidated.6
- As noted above, the SSN is an important sensory branch at the level of the ST, which provides sensory innervation to a large portion of the shoulder.5 The SSN lies on the superficial-lateral aspect (and is the first nerve to branch off) of the ST and must be identified and adequately blocked while performing an STB.1
- The supraclavicular nerve branches (namely, medial intermediate and lateral) arise from the lower aspect of the cervical plexus and provide sensory innervation to the neck (medial branch) and shoulder cape (intermediate and lateral branches). They lie superficial to the middle scalene muscle and are easily blocked with the same needle pass as blocking the ST.1
- Transverse cervical artery and dorsal scapular artery can both cross over, under or through the brachial plexus and interfere with needle placement in STB. Care should therefore be taken to identify and avoid these vessels with needle placement.1,3
BLOCKING THE ST
Indications
Indications for STB include surgical anaesthesia and/or postoperative analgesia for shoulder surgery. Coverage of the supraclavicular nerves (intermediate and lateral branches) is recommended and can be easily achieved with a single needle passage (details below). There are also reports of successful use for proximal humerus surgery.7
Contraindications
Contraindications include patient refusal, LA allergy, lack of equipment/resources (including unavailability of 20% intralipid solution in case of LA systemic toxicity), infection at the injection site, overlying vascular structures (particularly the transverse cervical and dorsal scapular arteries) that cannot be avoided during needle insertion even in different planes of scanning, bilateral block (due to risk of bilateral diaphragmatic paralysis), contralateral hemidiaphragmatic paralysis or other major respiratory impairment. Notably, despite STB being a superficial block performed at a compressible site, caution is advised in case of underlying coagulopathy and/or use of anticoagulants. In such cases, provided the clinical benefits of a STB outweigh the risks, the block should be performed by the most experienced regional anaesthesiologist available to mitigate the risk of inadvertent vascular puncture.
Comparison to ISB
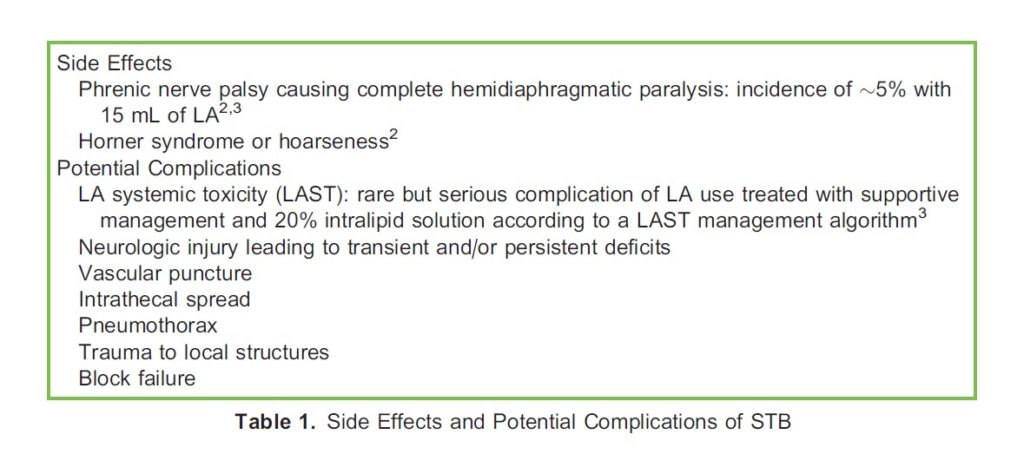
Initial studies have suggested potential advantages of STB over ISB, including a lower incidence of complete phrenic nerve palsy (~5% vs >70% when performed with 15 mL of LA),2,3,8 a thicker nerve sheath that may theoretically reduce the risk of inadvertent traumatic nerve injury,1,3 lower risk of injury to the dorsal scapular and/or long thoracic nerves that run within the middle scalene muscle (often pierced by the block needle during an ISB) at the level of the interscalene groove (Figure 2A) and avoidance of issues related to the anomalous course of C5.1 However, the transverse cervical and/ or dorsal scapular arteries can sometimes traverse (Figure 2D) and/or run in close proximity to the ST, which may pose some technical challenges to the performance of STB. Notably, the shoulder block9 constitutes a suitable alternative if or when a regional technique is planned primarily for perioperative analgesia. See Table 1 for side effects and potential complications.
Equipment
The following equipment is required:
- Standard monitoring equipment (electrocardiogram, pulse oximeter, blood pressure monitor, intravenous access)
- 20% lipid emulsion (must be immediately available)
- Sterile prep solution (such as chlorhexidine), drapes and ultrasound probe cover
- Sterile ultrasound gel
- Ultrasound machine with high-frequency linear probe
- Appropriate block needle
- LA with predetermined dose below the toxic limit (long-acting LAs such as ropivacaine are generally preferred due to prolonged postoperative analgesia; some practitioners may elect to use perineural adjuvants such as epinephrine to prolong the clinical effects of the LA)
- Saline-filled syringe for hydrodissection Nerve pressure guard and/or nerve stimulator, although not mandatory, are recommended to improve safety.10
Positioning
Position the patient supine with the head facing the contralateral side. It can also be helpful to place a pillow under the patient’s ipsilateral shoulder to lift it off the bed, allowing more room for needle placement. Alternatively, the patient can be in the lateral position with the side to be blocked up. The provider should stand either at the head of the bed or on the ipsilateral side of the patient, whichever feels most ergonomic. The ultrasound screen should be positioned in the most ergonomic way/level for the provider prior to initiating the block procedure. In addition, practitioners should ensure that the patient’s bed height is comfortable for scanning.
Approach and Scanning
Start scanning with a high-frequency linear probe in the supraclavicular fossa to identify pleura, first rib, subclavian artery and the brachial plexus, as if you were to perform a supraclavicular brachial plexus block. Follow the brachial plexus proximally to identify its separation into C5 and C6 roots, confirming the nerve root identity by continuing proximally to identify the ‘stoplight sign’ in the interscalene groove (Figure 2A) and the roots’ origins from the cervical spine. Alternatively, you may elect to start scanning proximally, at the level of the interscalene groove, by identifying the brachial plexus between the middle and anterior scalene muscles at the level of the C7 transverse process (Figure 2A). From this point, slowly move the ultrasound probe distally carefully following the C5 and C6 roots to the point where they converge into the ST (Figure 2B). Identify the point in the ST where the SSN branches off, which is generally located at the superficial-lateral aspect of the ST as a hypoechoic circle with a hyperechoic ring around it before splitting off (Figure 2C).1 Also identify the transverse cervical and dorsal scapular arteries, which may lie superficial, across or deep to the brachial plexus,1,3 keeping in mind their location in relation to your needle trajectory when proceeding to conduct the nerve block in order to avoid accidental arterial puncture. Chose a point in the ST proximal to the takeoff of the SSN and without an overlying vessel—this will be your scanning plane for the block (Figure 2). Confirm with colour Doppler the absence of vasculature in the needle path (which will start from the lateral edge of the ultrasound probe with an in-plane approach) before proceeding with the block.
Block Conduct
Procedures are as follows:
- Ensure proper equipment is available and prepared.
- Always perform a preblock neurologic assessment of sensory and motor function to identify and document preexisting neurologic compromise.
- Apply monitors to the patient and position the patient and ultrasound machine appropriately. Conduct the preprocedure checklist per institutional guidelines, confirming the site and surgical procedure and ensuring that all of the patient’s questions
have been answered to his or her satisfaction. - Prepare the skin with chlorohexidine or alternative sterile skin prep solution and apply sterile drapes. Apply a sterile probe cover to the ultrasound probe and use sterile ultrasound gel for ultrasonography.
- Scan to identify relevant anatomic structures and block plane as above (see the Approach and Scanning section; Figure 2).
- When a block plane has been chosen proximal to the SSN takeoff, infiltrate the skin with lidocaine at the needle insertion point.
- Insert your block needle lateral to the ST, starting from the lateral border of the middle scalene muscle and using a lateral-tomedial approach (Figure 2B). If possible, avoid traversing the middle scalene muscle with the block needle; instead, advance the needle over it. Pierce the deep cervical fascia with the block needle directed away from the ST to avoid accidental neural injury through a rebound effect. Once through the deep cervical fascia, pull the needle back and position its tip just below the fascia and next to the ST. Hydrodissection with small aliquots of saline can be used to confirm the position of the needle tip by visualising the injectate surrounding the ST. The LA mixture is then used to perform the block, with intermittent injections of small (3-5 mL) aliquots of LA and aspirations before each injection to ensure that the needle tip has not migrated into a blood vessel/nerve. The standard block volume is 15 to 20 mL. Low-volume analgesic blocks, however, can be successfully performed with 5 mL for a further decreased incidence of hemidiaphragmatic paralysis.8
- Upon withdrawing the needle, the supraclavicular nerves (intermediate and lateral branches), which supply sensory innervation to the shoulder cape, should be anaesthetised by pausing at the superficial tissues over the middle scalene
muscle and injecting another 5 mL of LA (Figure 2B).1 - Upon block completion, continue to evaluate motor and sensory function to assess for block success. In case of hemidiaphragmatic paralysis, the patient may report transient respiratory compromise.
SUMMARY
- STB reliably blocks the C5 and C6 nerve roots of the brachial plexus, providing anaesthesia/analgesia to the shoulder joint and proximal humerus, with a sensory distribution similar to the traditional ISB.
- STB results in less phrenic nerve paralysis than the traditional ISB does, while conferring similar sensory coverage.
- Initial studies have demonstrated a lower incidence of complete inadvertent hemidiaphragmatic paralysis following STB (~5%) compared with traditional ISB (>70%) when both blocks were performed with a similar volume (15 mL) of LA. Nevertheless, caution remains warranted, especially in patients with underlying respiratory compromise and/or contralateral diaphragmatic paralysis, given that the risk of phrenic nerve blockage following STB, despite reduced, is not negligible/non-existent.
- STB should be performed proximal to the takeoff of the SSN to ensure adequate sensory coverage of the shoulder.
- The supraclavicular nerve branches can be blocked with the same needle pass, ensuring coverage of the shoulder cape.
- Important structures to identify before proceeding with STB include the transverse cervical artery, dorsal scapular artery, SSN and the supraclavicular nerve.
REFERENCES
- Burckett-St. Laurent D, Chan V, Chin KJ. Refining the ultrasound-guided interscalene brachial plexus block: the superior trunk approach. Can J Anesth. 2014;61(12):1098-1102.
- Kim DH, Lin Y, Beathe JC, et al. Superior trunk block a phrenic-sparing alternative to the interscalene block: a randomized controlled trial. Anesthesiology. 2019;131(3):521-533.
- Kang RA, Jeong JS, Chin KJ, et al. Superior trunk block provides noninferior analgesia compared with interscalene brachial plexus block in arthroscopic shoulder surgery. Anesthesiology. 2019;131(6):1316-1326.
- Franco CD, Williams JM. Ultrasound-guided interscalene block reevaluation of the ‘‘stoplight’’ sign and clinical implications. Reg Anesth Pain Med. 2016;41(4):452-460.
- Chan C, Peng PWH. Suprascapular nerve block a narrative review. Reg Anesth Pain Med. 2011;36(4):358-373.
- Prates Ju´ nior AG, Vasques LC, Bordoni LS. Anatomical variations of the phrenic nerve: an actualized review. J Morphol Sci. 2015;32(1):53-56.
- Mistry T, Dey S, Kalbande J V. Superior trunk block for humerus surgery: application beyond the shoulder analgesia. Saudi J Anaesth. 2020;14(4):547-548.
- Kim H, Han JU, Lee W, et al. effects of local anesthetic volume (standard versus low) on incidence of hemidiaphragmatic paralysis and analgesic quality for ultrasound-guided superior trunk block after arthroscopic shoulder surgery. Anesth Analg. 2021;133(5):1303-1310.
- Shukla B, Chaddock M, Price D. The shoulder block. Anesthesia Tutorial of the Week (ATOW). 2021;453:1-7.



