General Topics
Valvular Heart Disease
- You visit a patient who is due to have an orthopaedic procedure. He tells you he gets occasional chest pain and shortness of breath on exertion. You notice he has an ejection systolic murmur. What investigations should you obtain if possible?
- You are asked to anaesthetise a patient who has known mitral stenosis who has broken their tibia and fibula. The orthopaedic surgeons want to perform an MUA. The patient tells you he gets short of breath on exertion. What is the best way to anaesthetise him?
- You visit a patient before their hernia operation. They are perfectly fit and can “walk miles”. You notice they have a ejection systolic murmur when you listen to their chest. Should you proceed with the proposed surgery or perform further investigations?
- Which patients tolerate general anaesthesia better? Those with stenotic heart valve disease or those with regurgitant heart valve disease?
- Which patients require antibiotic prophylaxis to prevent bacterial endocarditis?
Introduction
Valvular heart disease is found in 4% of patients over the age of 65 in the developed world. Patients may already be under a cardiologist with a known valve problem. Sometimes a murmur may be picked up during preoperative assessment. In each case the anaesthetist must:
- Assess the significance of the cardiac lesion for the proposed surgery
- Plan anaesthesia according to the haemodynamic picture
- Remember to administer antibiotic prophylaxis
Two dimensional echocardiography indicates abnormal valvular motion and morphology, but does not indicate the severity of stenosis or regurgitation except in mitral stenosis. Doppler echocardiography identifies increased velocity of flow across stenotic valves from which pressure gradients and severity of a stenosed valve may be estimated. Doppler flow imaging can also provide estimates of the severity of regurgitant valve disease.
Broadly speaking stenotic valvular heart disease (aortic stenosis and mitral stenosis) are the conditions which cause most concern. Patients have a fixed cardiac output and are unable to compensate for the reduction in systemic vascular resistance caused by the vasodilating effect of a general anaesthetic. This can sometimes have disastrous consequences
All patients with abnormal heart valves are at risk of bacterial endocarditis. It is important to give appropriate doses of the right antibiotics to prevent this complication.
Aortic stenosis
- Occasionally due to a congenital bicuspid aortic valve (2%), but usually due to rheumatic heart disease or valve calcification. Anatomic obstruction to left ventricular ejection leads to concentric hypertrophy of the left ventricular heart muscle. This reduces the compliance of the left ventricular chamber making it difficult to fill.
- Elevated filling pressures and sinus rhythm are required to fill the non-compliant left ventricle. “Normal” left ventricular end diastolic pressure may in fact reflect hypovolaemia.
- Properly timed atrial contractions contribute as much as 40 % to left ventricular preload in patients with aortic stenosis (normal = 20%). Rhythms other than sinus may produce a critical reduction in cardiac output as impaired filling of the left ventricle causes a fall in stroke volume.
- There is a high risk of myocardial ischaemia due to increased oxygen demand and wall tension in the hypertrophied left ventricle. 30% of patients who have aortic stenosis with normal coronary arteries have angina. Sub-endocardial ischaemia may exist as coronary blood supply does not increase in proportion to the muscular hypertrophy. Tachycardia is detrimental as it may produce ischaemia. Maintenance of diastolic blood pressure is crucial to maintain coronary perfusion.
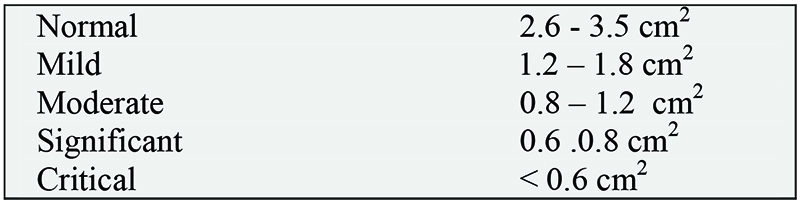
Aortic Valve Area
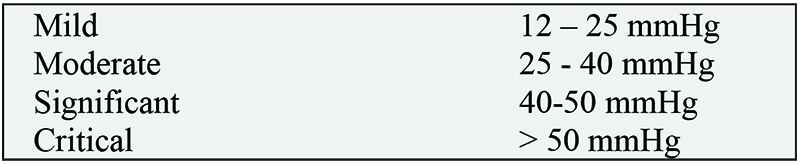
LV-Aortic Gradient
History
- Angina,
- Breathlessness
- Syncope
Symptoms do not correlate well to the severity of stenosis; some patients with small valve areas can be asymptomatic.
Examination
- Slow rising pulse with narrow pulse pressure
- Ejection systolic murmur maximal at the 2nd intercostal space, right sternal edge radiating to the neck
Investigations
- ECG will show left ventricular hypertrophy and strain (with secondary ST-T wave abnormalities)
- CXR remains normal until the left ventricle begins to fail. Post stenotic dilatation of the aorta and a calcified aortic annulus may be seen.
- An echocardiogram will enable calculation of valve gradient (see above) and a quantitative assessment of left ventricular performance.
- Cardiac catheterisation may be used to estimate the gradient across the valve. It will also give information about any concurrent coronary artery disease.
Perioperative care
- Symptomatic patients for elective non-cardiac surgery should have aortic valve replacement first as they are at great risk of sudden death perioperatively (untreated severe symptomatic stenosis has a 50% one year survival).
- Asymptomatic patients for major elective surgery associated with marked fluid shifts (thoracic, abdominal, major orthopaedic) with gradients across the valve > 50 mmHg should have valve replacement considered prior to surgery.
- Asymptomatic patients for intermediate or minor surgery generally do well if managed carefully.
Haemodynamic goals
- (Low) normal heart rate
- Maintain sinus rhythm
- Adequate volume loading
- High normal systemic vascular resistance
Patients with severe aortic stenosis have a fixed cardiac output. They cannot compensate for falls in systemic vascular resistance which result in severe hypotension, myocardial ischaemia and a downward spiral of reduced contractility causing further falls in blood pressure and coronary perfusion.
The selected anaesthetic technique should maintain afterload and avoid tachycardia to maintain the balance between myocardial oxygen demand and supply in the presence of a hypertrophied ventricle and reduced coronary flow. Performing the operation using local anaesthetic infiltration may be the safest method of all.
Titrate all anaesthetic drugs very carefully. Direct measurement of arterial blood pressure should be routine except for very short procedures. This should be commenced before induction of general anaesthesia.
Treat hypotension using direct acting alpha-agonists such as metaraminol or phenylephrine as these improve systolic and diastolic LV function. Aim to maintain blood pressure at pre-induction values. Careful fluid balance is essential, guided by invasive monitoring if possible (CVP, Oesophageal Doppler, Trans-oesophageal Echocardiography if available).
Arrhythmias must be treated promptly or haemodynamic collapse may ensue. Effective analgesia avoids catecholamine induced tachycardia and hypertension and the risk of cardiac ischaemia. However, central neuraxial blocks (epidurals/spinals) must be used with extreme caution because of the danger of hypotension due to afterload reduction. Limb blocks can be used alone or in conjunction with general anaesthesia.
Postoperative Management
- Have a low threshold for admission to ICU / HDU
- Meticulous attention must be paid to fluid balance and post operative pain management
- Infusions of vasoconstrictors may be required to maintain haemodynamic stability
Aortic regurgitation
- Primary aortic regurgitation is a sequelae of rheumatic heart disease or endocarditis.
- Aortic dissection and connective tissue disorders that dilate the aortic root (tertiary syphilis, Marfan’s Syndrome and ankylosing spondylitis) result in secondary aortic incompetence.
- Valvular regurgitation usually develops slowly over many years allowing the left ventricle time to adapt to increased volume load.
- Acute aortic regurgitation secondary to endocarditis or aortic dissection presents with acute left heart failure and pulmonary oedema. Such patients require emergency valve
surgery.
In patients who have chronic aortic regurgitation
- Afterload and heart rate determine the degree of regurgitation. Lower aortic pressure decreases left ventricular afterload, augmenting forward flow.
- Vasodilators by lowering afterload increase forward flow, decrease left ventricular size and enhance ejection fraction.
- Heart rates greater than 90 beats per minute reduce the diastolic regurgitation time and degree of regurgitation. This improves forward flow and thus cardiac output.
- Aortic diastolic pressure is dependant on the aortic valve and decreases when the valve becomes incompetent.
History
- Dyspnoea, secondary to pulmonary congestion
- Palpitations
Examination
- Widened pulse pressure
- Collapsing (‘waterhammer’) pulse. Corrigan’s Sign – visible neck pulsation. De Musset’s Sign – head nodding. Quincke’s Sign – visible capillary pulsations in the nail beds
- Diastolic murmur loudest in the 2nd intercostal space at the right sternal edge
Investigations
- CXR shows cardiomegaly with a boot shaped heart
- ECG shows the voltage criteria for left ventricular hypertrophy
- Echocardiography gives qualitative analysis of the degree of regurgitation
Perioperative care
Asymptomatic patients usually tolerate non-cardiac surgery well. Patients with a functional capacity less than 4 MET’s (unable to climb a flight of stairs or walk on level ground at greater than 6 km/hr) need to be considered for valve replacement surgery first.
Haemodynamic goals
- High normal heart rate – around 90 bpm
- Adequate volume loading
- Low systemic vascular resistance
- Maintain contractility
The selected anaesthetic should maintain afterload in the low normal range whilst maintaining diastolic pressure. Spinal and epidural anaesthesia are well tolerated. Treat SVT / atrial fibrillation if associated with hypotension promptly with synchronised DC cardioversion. Persistent bradycardia can be treated with beta-agonists. Intra-arterial pressure monitoring is useful for major surgery.
Mitral stenosis
- Rheumatic fever is the commonest cause. The minority have isolated mitral valve stenosis, the majority mixed mitral valve disease (stenosis and regurgitation). Mitral valve stenosis under fills the left ventricle and increases both pressure and volume upstream of the valve.
- The left ventricle functions normally but is small and poorly filled.
- Initially the left atrium dilates keeping the pulmonary artery pressure low. As disease progresses pulmonary artery pressure increases and medial hypertrophy develops resulting in chronic reactive pulmonary hypertension. The right heart hypertrophies to pump against a pressure overload, then fails. Secondary pulmonary / tricuspid regurgitation develops.
- The pressure gradient across the narrow mitral orifice increases with the square of cardiac output (e.g. pregnancy). Rapid heart rates, especially with atrial fibrillation, decrease diastolic filling time and markedly decrease cardiac output.
- LV filling is optimised by a slow heart rate.
Patients are frequently dyspnoeic due to fluid transudate into the lungs which reduces lung compliance and increases the work of breathing. Pulmonary oedema may occur if the pulmonary venous pressure exceeds the plasma oncotic pressure. This is especially likely if a large fluid bolus, head down position or a uterine contraction raises pulmonary pressure suddenly.
History
- Dyspnoea, haemoptysis, recurrent bronchitis
- Fatigue
- Palpitations
Examination
- Mitral facies – malar flush on cheeks
- Peripheral cyanosis
- Signs of right heart failure (elevated JVP, hepatomegaly, peripheral oedema, ascites)
- Tapping apex beat. Loud first heart sound, opening snap (if in sinus rhythm) and low pitched diastolic murmur heard best at the apex (with the bell of the stethoscope).
Investigations
- ECG: P mitrale (left atrial enlargement) if sinus rhythm. Atrial fibrillation usual.
- CXR: valve calcification. Large left atrium (lateral film). Double shadow behind heart on PA film. Splaying of the carina. Kerley B lines indicating pulmonary congestion.
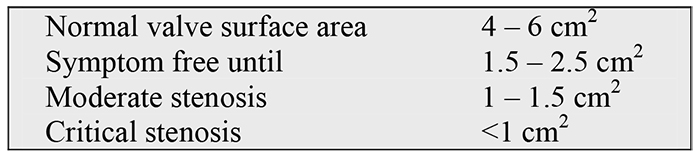
- Echocardiography; Measures the gradient and valve area – see above
Perioperative care
Asymptomatic patients usually tolerate non cardiac surgery well. Patients with poor functional capacity (less than 4 MET’s) need to be considered for mitral valve replacement.
Haemodynamic goals
- Low normal heart rate 50-70/min. Treat tachycardia aggressively with β blockers
- Maintain sinus rhythm if possible. Immediate cardioversion if atrial fibrillation occurs peri-operatively
- Adequate preload
- High normal systemic vascular resistance
- Avoid hypercarbia, acidosis and hypoxia which may exacerbate pulmonary hypertension
Anaesthesia – similar to aortic stenosis as there is a relatively fixed cardiac output. Maintain adequate afterload, slow heart rate and avoid hypovolaemia. Measure CVP/PAOP and maintain a high preload. Spinal and epidural anaesthesia may be very hazardous.
Mitral regurgitation
- Mitral regurgitation (MR) results from leaflet, chordal or papillary muscle abnormalities, or is secondary to left ventricular dysfunction.
- Leaflet MR is a complication of endocarditis, rheumatic fever or mitral valve prolapse.
- Chordal MR follows chordae rupture after acute myocardial infarction or after bacterial endocarditis.
- Papillary muscle MR results from ischaemic posterior papillary muscle dysfunction.
- Left ventricular failure leads to varying amounts of MR when the mitral annulus dilates.
- As much as 50% of the left ventricular volume flows into a massively dilated left atrium through the incompetent mitral valve before the aortic valve opens. Left ventricular ejection fraction is therefore supranormal.
- Pulmonary vascular congestion develops followed by pulmonary hypertension.
- The degree of regurgitation is determined by the afterload , size of the regurgitant orifice and the heart rate. A moderately increased heart rate (>90 bpm) decreases the time for regurgitation in systole and decreases the time for diastolic filling reducing LV overload.
- Stroke volume is maintained until late in the disease process despite as much as 50% of the left ventricular volue being ejected into the left atrium through the regurgitant mitral valve.
History
- Fatigue, weakness,
- Dyspnoea
Examination
- Displaced and forceful apex (the more severe the regurgitation the larger the ventricle)
- Soft first heart sound, apical pansystolic murmur radiating to the axilla, loud third heart sound
- Atrial fibrillation
Investigations
- ECG: left atrial enlargement. Atrial fibrillation.
- CXR: left atrial and left ventricular enlargement. Mitral annular calcification.
- Echocardiography assesses the degree of regurgitation It may also show thrombus in the enlarged left atrium. (Transoesophageal echo particularly useful as mitral valve close to the oesophagus).
Perioperative care
Asymptomatic patients usually tolerate non-cardiac surgery well. Patients with poor functional capacity (< 4 MET’s) need to be considered for valve replacement surgery.
Haemodynamic goals
- High normal heart rate
- Adequate preload
- Low systemic vascular resistance
- Low pulmonary vascular resistance
Anaesthesia aims are similar to aortic regurgitation. Preload can be difficult to estimate; for major non-cardiac surgery a pulmonary artery catheter may be useful. In advanced disease pulmonary hypertension is common thus avoid factors that increase pulmonary artery pressure (hypoxia, hypercarbia, high inspiratory pressures, acidosis)
Mitral valve prolapse
- Common (incidental finding in 5%) most common in young females
- Associated with atypical chest pain, palpitations, syncope and embolic phenomena.
- A mid systolic click and late diastolic murmur may be heard.
- Echocardiography shows enlarged redundant mitral valve leaflets prolapsing into the left atrium during mid to late systole causing arrhythmias and regurgitation.
- Patients may be taking antiarrhythmic’ medications must be continued perioperatively.
Mixed valve lesions
The patient with an undiagnosed heart murmur
Most heart murmurs do not signify cardiac disease. Many are related to physiological increases in blood flow.
An important consideration is the presence or absence of symptoms and the ability of the patient to exercise. Many asymptomatic children and young adults with a murmur need no further work after an initial history and examination. However there are many elderly asymptomatic patients who have systolic murmurs related to sclerotic aortic valve leaflets, flow into tortuous non compliant vessels or a combination of these. It is important that these murmurs are distinguished from the murmur caused by aortic stenosis which is prevalent in this age group.
Take a full history and look at the ECG and CXR. The patient with a murmur who has a reasonable exercise tolerance (able to climb a flight of stairs, walking at 6 km/hr on the flat) associated with a normal ECG and CXR will withstand minor and intermediate surgery without problem. Conversely poor functional capacity in association with abnormal ECG (e.g. evidence of ventricular hypertrophy or of a previous myocardial infarction) should be investigated initially with an echocardiogram. Asymptomatic patients presenting for major surgery with the associated large fluid shifts should have an echocardiogram to rule out significant valvular pathology.
Two dimensional echocardiography indicates abnormal valvular motion and morphology but does not indicate the severity of stenosis or regurgitation except in mitral stenosis. Doppler echocardiography identifies increased velocity of flow across stenotic valves from which the severity of the stenosis may be implied. Doppler flow imaging will also show regurgitant jets and can provide semi quantitative estimates of the severity or regurgitant valve disease.
Bacterial endocarditis prophylaxis during general anaesthesia for adults
Indicated for patients with heart valve lesions, septal defects, patent ductus, prosthetic valves or previous endocarditis. For full details please consult current BNF.
Dental treatment
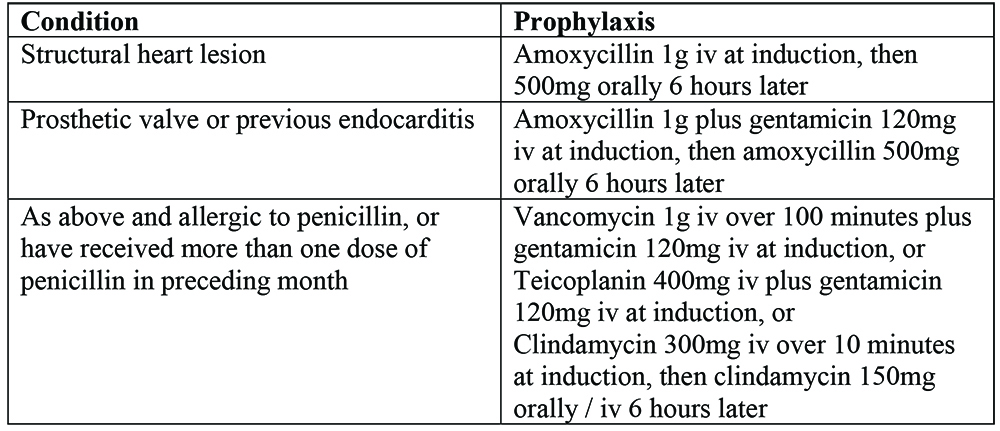
Genitourinary or gastro-intestinal procedures
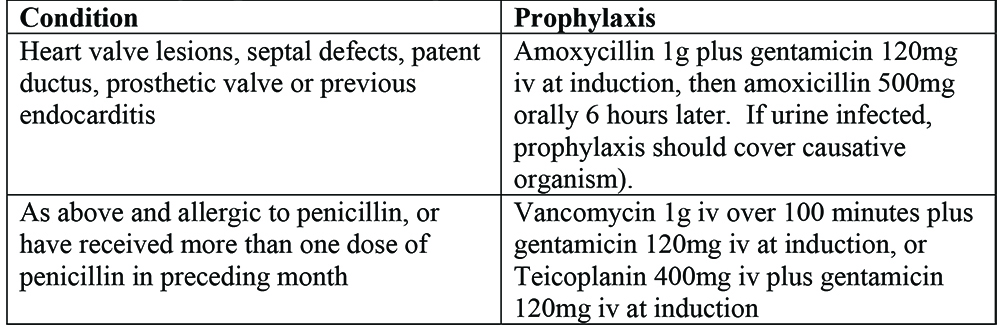
Obstetric and gynaecological surgery prophylaxis as for genitourinary, if prosthetic valve or previous endocarditis
Answers to questions
- An ECG and an echocardiogram would be useful .In addition a cardiac catheter might reveal coronary artery disease. (50% of patients with aortic stenosis will have significant coronary artery disease). If the patient has severe aortic stenosis the aortic valve should be replaced before the proposed surgery. The indications for coronary artery surgery prior to elective surgery are severe left main stem stenosis or severe triple vessel disease.
- Try and find out if the patient has any idea about the severity of their mitral stenosis. The patient is symptomatic which is usually associated with a valve surface area of less than 1.5 cm2 . Such patients have a fixed cardiac output and need careful handling. A carefully titrated general anaesthetic is probably best, ideally with an arterial line inserted before induction.
- The fact that the patient has a good functional capacity is reassuring. If the proposed surgery does not involve entering body cavities with the associated large fluid shifts it is reasonable to proceed. However if major thoracic or abdominal surgery is proposed an echocardiogram is a useful investigation if available.
- Patients with regurgitant heart valve lesions tolerate anaesthesia and surgery well. Most general anaesthetics cause vasodilatation which reduces the size of the regurgitant fraction and augments forward blood flow in the aorta. The vasodilatory effects of general anaesthesia can be catastrophic for patients with severe aortic or mitral stenosis.
- All patients with valvular heart disease need antibiotic prophylaxis. Current British National Formulary recommendations for this are:



