Pain
QUESTIONS
Answer the flowing questions true or false:
- Poor recognition and management of acute pain occurs commonly
- Acute pain has no bearing on post-operative complications
- Pain increases anabolic hormone production
- The severity of acute post-operative pain may has been suggested as a risk factor for the development of chronic pain
- In general, pain causes an increase in parasympathetic nervous activity
- Nociception, and a patient’s perception of pain are the same thing
- If possible, pain should be assessed with the patient active
- Pain should be assessed regularly during treatment
- Patient comfort only relates to analgesia
- Adverse effects of analgesic drugs need not be monitored during treatment
- Intramuscular injection provides reliable drug absorption
- Continuous IV opioid infusion carries the highest risk of serious adverse effects
- Patient-controlled analgesia devices are only used to deliver opioid medication
- Multi-modal analgesia aims to reduce opioid doses and adverse effects
- Acute pain service teams have clinical responsibilities only
INTRODUCTION
The International Association for the Study of Pain (IASP) have described pain as, ‘an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage’. Pain experienced as the result of injury, trauma or disease, can be considered acute pain. Usually this pain subsides with healing. Should it persist beyond this period, then this pain is progressing to chronic pain. Acute pain is encountered in a wide variety of clinical situations, including post-operative patients, trauma, and illness. Accurately reporting of the incidence of acute pain is, therefore, very difficult, and most likely often under-estimated
However, the importance of effective pain management cannot be overstated. Acute injury and associated pain can lead to pathological consequences in both the short, and long term.
Several studies have shown that poor recognition of acute pain and inadequate pain management occurs commonly. The reasons for this persisting inadequacy are likely to be multifactorial and may include failure in assessment, underuse of effective analgesic techniques, poor protocol availability or application, and insufficient practitioner education.
This tutorial aims to:
- Explain the need for effective management of acute pain
- Describe the role and method of assessing acute pain
- Discuss modern analgesics and their application
WHY IS EFFECTIVE PAIN MANAGEMENT IMPORTANT?
Acute pain is not just an unpleasant experience for the patient. It may have some bearing on patient outcomes such as post-operative complications and length of hospital stay. Pain is thought to play a role in the activation of the ‘stress’ response to injury. This stimulates catabolic hormone release, increased sympathetic nervous activity and coagulation, and may impair immune function
This stress response manifests itself in several physiological systems and can give rise to complications that threaten a patient’s health.
Stimulation of the sympathetic nervous system increases cardiovascular parameters such as heart rate, blood pressure and systemic vascular resistance. This greater workload increases myocardial oxygen demand, and can provoke myocardial ischaemia or infarction, if such demand exceeds oxygen delivery. Patients with coronary artery disease are at greater risk of such a complication. Furthermore, changes in regional blood flow may decrease supply to the skin, and impair wound healing.
Immobility due to pain, and increased coagulation caused by the ‘stress’ response, can predispose the patient to thromboembolic complications.
Severe pain in the upper abdomen or chest can impair respiratory function and compromise the patient’s ability to clear sputum and secretions. This may lead to atelectasis, hypoxaemia, and lower respiratory tract infections.
Increased levels of catabolic hormones can lead to increased protein breakdown and hyperglycaemia; the former may impair wound healing.
The experience of pain is influenced by several psychological factors including mood, culture, coping skills, beliefs and previous pain experiences. These factors may impact upon the response to both pain and its treatment, and so should be considered when assessing and managing acute pain. Such factorshowever, are often overlooked. Relentless pain can have profound psychological sequelae such as post-traumatic stress disorder (PTSD).
Last, but certainly not least, is the possible development of chronic pain, from the acute pain state. A significant proportion of surgical or trauma patients develop chronic pain states. The severity of acute pain in the immediate period after surgery has been suggested as an important risk factor. Effective pain management in these patients may go some way toward guarding against the development of Persistent Post-Surgical Pain (PPSP).
ASSESSMENT OF PAIN
Pain is a subjective experience, and its severity can be influenced by many factors as mentioned previously. The patient’s perception of pain therefore, is different from nociception.
The type of acute pain, and its cause, may affect the treatment chosen, and the response to this treatment. Acute pain may be nociceptive (somatic or visceral), neuropathic, or a combination of the two (mixed). Consideration of pain in terms of its nature and relationship to injury facilitates effective acute pain management.
From this, it can be realised that assessing pain is as challenging as it is important. This challenge is emphasised by the subjective nature of pain, and the wide variation in individual experience and need for treatment. In order for such an assessment to be applied across a spectrum of patients, it must be both accurate and reproducible.
The main components of such an assessment include a pain history, a measure of severity and treatment response, and ideally consideration should be given to the psychological factors that contribute to the pain experience.
Pain History
A pain history should include the character, intensity, location, underlying cause, associated symptoms and current analgesic use. In addition, the patient’s ideas and concerns in relation to pain, and their expectations with regard to analgesia should be elicited. This history can be repeated after treatment has begun to monitor progress.
Measurement
Given the subjective nature of pain, its measurement through self-reporting would seem the most valid technique. Assessment of function also forms an important part of measuring pain.
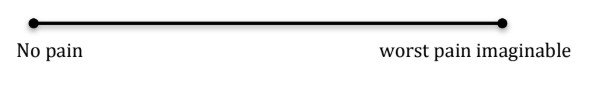
A number of uni-dimensional scales are available for the measurement of acute pain. The categorical scales include verbal (verbal descriptor scale VDS), numerical (Verbal Numerical Rating Scale VNRS) and visual (Visual Analog Scale).
The VNRS is most commonly employed. The patient is asked to score their pain using a numerical scale of zero to ten. The absence of pan is reflected by a score of zero with increasing score reflecting worsening pain. A score of ten describes the ‘worst imaginable pain’. This scale does not require any equipment, and is easily repeatable. However, the patient must be able to understand the scoring system and communicate their answer.
The VAS is similar to the VNRS. A 10cm line with descriptors such as ‘no pain’ and ‘worst pain imaginable’ at opposite ends is shown to the patient. The patient is asked to mark on the line the point that best reflects their level of pain. The distance from ‘no pain’ to this mark is then measured in millimetres, giving a VAS score of 1-100. (see figure 1 below).
This scale requires a small amount of equipment, but can be adapted to measure other variables such as treatment side effects or pain relief.
The VDS is a quick and simple scale that uses different words to rate the severity of pain. An example would be a four-point scale containing the words ‘no pain’, ‘mild pain, moderate pain, and ‘severe pain’.
Assessment of Functional Pain
Pain can also be assessed with the patient active. The Functional Activity Score ranks impairment caused by pain into three categories:
- A – no limitation,
- B – mild limitation,
- C – significant limitation
The patients’ surgical circumstances and pre-existing co-morbidities may determine the type of activity chosen. Examples would include deep inspiration in a patient after thoracic or abdominal surgery, or walking following lower limb joint arthoplasty. In this way, the score is specific to the patient and facilitates re-assessment following therapy.
Adverse effects
In order to deliver effective yet safe analgesia, any on-going assessment of pain should include the identification of adverse effects associated with the analgesic drugs employed. Examples of such effects would be nausea, vomiting, sedation or respiratory depression associated with opioids, or the possible hypotension or neurological injury that can occur with epidural anaesthesia.
Pain has been described as ‘the fifth vital sign’, a moniker that reflects the need for regular assessment and measurement during the treatment regimen. In this way, the response to treatment, and any incumbent adverse effects, can be gauged, and the regimen tailored appropriately.
Finally, it is important for both clinician and patient to realise that complete pain relief may not be possible, and that the aim is to establish patient comfort. This notion of comfort will vary significantly between patients and encompasses not only pain scores, but also side effects of analgesic drugs and functional ability.
TREATMENT OF ACUTE PAIN
Acute pain can now be treated by a large variety of analgesic agents, applied in many different ways, in hospital or in the community. This allows the clinician, in consultation with the patient, to tailor an analgesic regime that is specific to that patient’s pain, analgesic requirements, and individual circumstances.
In order to treat pain effectively, several factors should be considered and understood. In addition to the history of the pain, its severity, cause, and effect upon the patient, thought should be given to the type of analgesic agent to be used, the most suitable method of delivery, and the frequency required. Consideration should also be given to the resources available for administration of these drugs, and the continued assessment of their beneficial and adverse effects.
METHOD OF DELIVERY
The chosen method of delivery should reflect the consideration given to several factors including patient preference, aetiology and nature of their pain, clinical condition, and the characteristics of the delivery method itself.
Oral administration is the most commonly employed route. It is simple, economical, well-tolerated and suitable for self-administration. Onset time can be slow and this route does require a functioning gastro-intestinal tract.
The rectal route offers an alternative to the oral route, but offers unreliable absorption and requires specific patient consent if not self-administered.
The intravenous route is the preferred route when treating severe, acute pain. Fast onset allows dose to be given in a titratable fashion. This route requires a higher level of staff training, an intravenous cannula with subsequent infection risk, and carries the highest risk of adverse drug effects.
Intramuscular injections have commonly been used on hospital wards to administer opioid medication in the belief that it is a safer alternative to the intravenous route. However, current evidence disputes this. Administration can be painful for the patient, and poses an infection risk. In addition, muscle hypo-perfusion, if present, can produce unpredictable drug absorption.
The subcutaneous route is better tolerated by patients and can prove to be as effective as the intramuscular route in delivering opioid drugs. However it provides only slow onset pain relief and may require a subcutaneous cannula to be used.
Transdermal patches are commonly used to deliver opioid medication to patients suffering chronic or cancer pain. The specific kinetics of this method include slow onset and offset, long half-life and the possibility of delayed absorption after patch removal. These features hinder this routes suitability in the management acute pain
The transmucosal route includes intranasal, sublingual and buccal delivery. Preparations of fentanyl are available for both intra-nasal and sublingual administration. As yet, these preparations have only received approval for the treatment of breakthrough pain in cases of chronic or cancer pain. Ketamine can be delivered via this route for treating procedural pain or acute pain in the emergency department.
Patient-Controlled Analgesia (PCA)
With this technique a programmable infusion pump administers a specified drug bolus when commanded by the patient. These boluses are separated by a minimum lockout period that prevents further drug delivery, even if the patient commands it. This serves as a control to prevent excessive dosing and limit side effects. This system is designed to address the variability in individual dose requirements. It also provides the patient with a greater degree of control over their pain therapy, allowing them to balance their own level of analgesia against any side effects the medication may bring.
This concept is often applied to opioid drug administration and has been employed in regional anaesthetic techniques such as epidural or peripheral nerve catheters. When compared to more conventional methods of delivery, the use of morphine and fentanyl in PCA results in improved analgesia and greater patient satisfaction.
Patients’ analgesic requirements and sensitivity to medication vary and so treatment protocols, although standardised, must be adjustable. Therefore, to provide effective pain relief to individual patients, trained staff must to be able to review each case and alter the PCA device’s program.
Causes of complications include equipment malfunction, operator error, and patient error. Reported serious adverse effects have been the results of errors made in prescribing, device programming or drug dilution. To minimise these risks, regular equipment maintenance, thorough staff training and standardised drug concentrations should be employed. Only the patient should have control of drug delivery. Administration by a family member, described as “PCA by proxy”, has resulted in significant mishap.
Side effects common to opioid use are not always reduced by PCA, however the risk of respiratory depression, is smaller than that with continuous IV infusion.
More recently, an iontophoretic fentanyl patient-controlled transdermal delivery system, or PCTS, has been developed in several studies shown to be both as effective and as safe as traditional intravenous morphine PCA regimens. However, potentially dangerous equipment faults have resulted in the withdrawal of this technique for now.
OPIOID ANALGESIA
Opioids are the cornerstone of the treatment of moderate or severe acute pain. A huge range of different drugs is available in a variety of formulations. Morphine represents the “gold standard” and provides the benchmark for the comparison of new agents.
Opioids produce effects by activating both central and peripheral opioid receptors. Activation of the mu-receptor (MOR) produces both analgesia and other unwanted effects. Some contribution to these effects is given by the concurrent activation of Delta and Kappa opioid receptors.
Unpleasant side effects of opioid drugs include sedation, nausea, vomiting, reduced gastrointestinal motility or constipation, pruritus, urinary retention and dysphoria. Respiratory depression is rare but extremely serious as it can result in hypoventilation, hypoxia and if even death if not treated.
The oral, subcutaneous, intramuscular, intravenous, and transdermal routes can deliver opioids. In addition, opioids can be given as adjuncts in central neuraxial anaesthesia.
Oral opioids
The oral route is considered the route of choice to treat mild or moderate acute pain. Oral opioids are usually well tolerated and prove as effective as parenteral opioids when appropriate doses are administered. They can be prescribed and continued in the outpatient setting.
Examples include morphine, tramadol, oxycodone and codeine.
Oral morphine and oxycodone are formulated in immediate release (IR) and slow release (SR) preparations. This allows greater flexibility when prescribing a regimen. The IR form proves useful managing the early period of pain. Should extended treatment be necessary, conversion to the SR form can provide a stable background level of analgesia, which may be supplemented by the IR form to treat breakthrough pain.
Tramadol is centrally-acting and provides analgesia both through MOR activation and through other pharmacological mechanisms. It is available in IR or SR forms, carries a lower risk of sedation, constipation and respiratory depression, and along with codeine, can provide good relief from moderate acute pain.
Intramuscular and Subcutaneous Opioids
Until recently, post-operative opioid analgesia for the majority of patients was commonly prescribed as a standard, four hourly dose of 10 milligrams (mg) of morphine, to be given via the intramuscular route. This rigid approach meant underdosing some patients, leaving them in pain, whilst overdosing others and risking serious side effects. If possible, it is now recommended to avoid this route. If selected, then drug dosage should take into account age, weight and clinical condition. Furthermore a dose interval of one or two hours, as required, would offer more flexibility.
Subcutaneous opioids exhibit similar absorption to the IM route and can be given as intermittent boluses or as a continuous infusion. Patients prefer this route. One drawback of this route is skin irritation with some opioids. Morphine and hydromorphone are best tolerated.
Intravenous opioids
This is the preferred route for the management severe acute pain. Available regimens include continuous infusion, nurse administered bolus doses or PCA. Excessive dosing can easily result in respiratory depression and so close monitoring by well-trained staff should be employed.
Fast relief from pain in the immediate post-operative period is often delivered through intermittent IV boluses. This offers a rapid and predictable response to opioid agents. With careful and regular monitoring of pain scores and vital functions, further boluses may safely be given, and dosing can be titrated to each individual’s pain.
Continuous infusion has the advantage of maintaining a steady, therapeutic drug concentration in the bloodstream, however, of all the parental routes described, this one poses the greatest risk of respiratory depression. In order for this method to be administered both safely and effectively, pain scores and adverse effects should be frequently assessed and infusion equipment must be reliable and well maintained.
NON-OPIOID/ADJUVANT ANALGESIC DRUGS
Several drugs other than opioids or local anaesthetic are used in the management of acute pain, either as an adjunct, or as the sole treatment.
Paracetamol/acetaminophen
Paracetamol is an analgesic drug that also acts as an anti-pyretic. It is one of the most commonly prescribed, and widely used drugs in the world, and is often employed as the first agent in any analgesic regimen.
Despite its popularity, its mechanism of action is not well understood. Current ideas include modulation of the serotonergic anti-nociceptive system, antagonism at the NMDA receptor and prostaglandin inhibition in the hypothalamus.
As an analgesic it is relatively effective and the small risk of side effects is reflected in its high tolerability. Administration is via the oral, rectal or intravenous route. It is used as the first line analgesic in the management of mild or moderate acute pain, and has been shown to reduce post-operative opioid requirements. Whilst demonstrating a good side effect profile, it should be remembered that excessive doses of paracetamol could prove hepatotoxic and result in fulminant liver failure and death.
Non-steroidal anti-inflammatory drugs (NSAIDs)
NSAIDs are used in the management of mild or moderate acute pain.
They have anti-inflammatory, analgesic, anti-pyretic and anti-platelet effects, which vary from drug to drug. These effects are due to the reduction in inflammatory mediators, released at the site of injury, due to the inhibition of the cyclo-oxygenase (COX) enzyme. These inflammatory mediators, which include prostaglandins, prostacyclins and thromboxane A2., also have roles to play in platelet function, and in both kidney and intestinal mucosal protection. It is the inhibition of these roles that account for the majority of the adverse effects of these drugs.
The COX enzyme is expressed in two isoforms, COX-1 and COX-2. NSAIDs inhibit both of these isoforms. Recently selective COX-2 inhibitors, known as coxibs, have been developed. Both types of drugs demonstrate similar efficacy and can be delivered via oral, rectal and intravenous routes. Some NSAIDs are available as a topical gel.
Adverse effects include renal toxicity, gastro-intestinal irritation and ulceration, impaired platelet function, bronchospasm, dizziness, headaches, and even cardiac failure. Some of these effects are due to the inhibition of COX-1, and provided the stimulus for the development of coxibs, which would avoid such effects. These selective COX-2 inhibitors do not reduce platelet function, or increase the risk of gastric ulceration during short-term administration. They also do not cause bronchospasm in patients susceptible to aspirin-induced asthma.
However, uncertainty remains regarding the effect of coxibs on renal function. Therefore, careful consideration should be given before they are prescribed to patients who are hypovolaemic, hypotensive, already taking nephron-toxic medication, or who have pre-existing renal impairment.
Concerns have been raised with regard to cardiovascular morbidity caused by the use of NSAIDs and coxibs. These concerns remain a matter for debate. Currently, a short course of coxib therapy after non-cardiac surgery is acceptable, however, their use is contraindicated following coronary artery bypass surgery. The impairment of bone healing following orthopaedic surgery is another concern. The evidence for this is not conclusive, and short-term coxib use is still recommended in patients not on concurrent steroid therapy, who do not smoke, and in whom there is no evidence of non-union.
NSAIDs and coxibs can form an important part of any analgesic regimen prescribed to manage acute pain, particularly in cases that involve an inflammatory component.
N-Methyl-D-Aspartate (NMDA) receptor antagonists
Central sensitisation describes the development of spinal cord neuron hyper-excitability caused by repetitive and persistent painful stimuli from the periphery. This produces exaggerated responses to further painful stimuli known as hyperalgesia, and the experience of pain to a non-painful stimulus, known as allodynia. This phenomenon occurs in all patients after acute injury, but in the vast majority it appears to relent as the injury heals. The condition can become chronic and lead to chronic pain states. It is thought that the NMDA receptor plays a significant role in both central sensitisation, and in neural transmission for many types of pain.
In the treatment of acute pain, the NMDA receptor antagonist Ketamine, is often given in addition to opioid medication. Ketamine, itself an anaesthetic agent, can be delivered via oral, intravenous, subcutaneous, sublingual or transdermal routes. It provides good analgesia for procedural pain and neuropathic pain and offers a useful adjunct or alternative to opioids when managing the opioid tolerant patient. Concurrent use with opioid PCA has revealed an opioid sparing effect, better pain control and reduced nausea and vomiting.
Given its anaesthetic qualities, large doses should be administered with great care, by trained staff using sufficient monitoring equipment. Other adverse effects include hallucinations, nightmares, delirium and agitation. These effects can usually be tempered by the administration of a benzodiazepine.
α-2 adreno-receptor agonists
Pain transmission can be inhibited by potentiation of descending, inhibitory spinal pathways. This potentiation can be realised through activation of α-2 adreno-receptors in the spinal cord, brain stem or on peripheral sensory nerve terminals. Clonidine is the most commonly used drug in this class.
Administration routes include oral, IM, IV, and SC routes. Clonidine has been found to provide analgesia and so reduce opioid requirements. It does however, exhibit several side effects including sedation, dizziness, dry mouth hypotension, bradycardia, and decreased bowel motility.
Nitrous Oxide
Nitorus oxide is an inhalational anaesthetic agent. It is used in a 50:50 mixture with oxygen, known as Entonox, which ensures a sub-anaesthetic, non-hypoxic mixture is delivered. It has a rapid onset and short duration of action, which prove ideal for providing analgesia for labour pain, dental surgery or short procedures such as joint relocation. Self-administration via a one-way demand mouth piece or face mask is recommended as this provides an extra degree of safety.
Anticonvulsants and Antidepressants
Some of these drugs are known to be effective in treating chronic neuropathic pain. Acute forms of neuropathic pain may also be amenable to this therapy.
The tricyclic antidepressant amitriptyline provides some analgesia after a few days of low dose therapy. Its action centres upon the inhibition of monoamine re-uptake into nerve terminals. Monoamines such as noradrenaline and serotonin modulate pain transmission via descending inhibitory pathways. The adverse effects of dry mouth, blurred vision, tachycardia, constipation and urinary retention are due to the anticholinergic qualities of these drugs.
Alternative anti-depressants, which may have a better side effect profile, include the Serotonin-Noradrenaline Reuptake Inhibitors (SNRIs) venlafaxine and duloxetine.
Pregabalin and gabapentin are often employed to treat neuropathic pain, however, both are becoming more popular as analgesics given pre-operatively. They temper the central sensitisation of pain pathways stimulated by injury, and so confer analgesic benefit. They also provide a degree of anxiolysis. Evidence has shown both drugs to reduce post-operative pain, and exhibit opioid sparing effects. It is also thought that these drugs may have a role to play in preventing the development of persistent post-surgical pain. Dosage remains a point for discussion and further research is required to advise a dose that offers good analgesic benefit whilst minimising adverse effects such as dizziness and sedation.
Calcitonin
This hormone is involved in calcium homeostasis. A role in acute pain management has been suggested from evidence of salmon calcitonin proving effective shown in the reduction of acute pain caused by osteoporotic related vertebral fractures. It has also been shown to reduce acute phantom limb pain. This effect is believed to be due to modulation of serotonergic activity in central pain pathways, and this mechanism may explain the side effects of nausea, vomiting, flushing and drowsiness. At present evidence for its use in acute pain management is limited and further research is required.
REGIONAL ANAESTHESIA
Detailed description of regional anaesthetic techniques is beyond the scope of this article, but procedures such as epidural or spinal anaesthesia, peripheral nerve blocks and catheters can play a very effective role in acute pain management.
In essence, regional anaesthesia involves the blockade of pain transmission from the peripheral site of pain to the central nervous system through the targeted deposition of local anaesthetic agents and analgesic agents around individual nerves, nerve plexi, or the spinal cord. These techniques are commonly employed for treating post-surgery pain, but also have a role for treating other forms of acute pain. They have been shown to improve pain scores post-operatively, reduce opioid requirements and adverse effects, and may aid rehabilitation.
Such procedures are not without risk of complications and thus should be performed by a skilled clinician, usually an anaesthetist, and require follow-up to detect complications, manage infusions, and ensure quality control.
MULTI-MODAL ANALGESIA
Multi-modal analgesia describes the use of more than one class of analgesic drug when treating pain. This approach provides improved pain relief and allows for the moderation of drug doses, with the added benefit of reduced drug-related side effects. This concept has expanded with the development of new agents that alleviate pain via different pharmacological mechanisms. Regimens may also include invasive techniques such as regional anaesthesia.
Multi-modal regimens often combine opioid analgesics with non-opioid analgesics, reducing required opioid dose required to deliver good pain relief. This in turn should produce a reduction in opioid-related side effects such as nausea and vomiting. A number of international guidelines now support the use of multi-modal analgesia in the management of acute pain.
One common example of this technique is the combination of a NSAID drug with an opioid. Analgesia is provided as the centrally acting MOR-mediated analgesia of the opioid is complimented by the anti-inflammatory action of the NSAID at the site of injury. Studies have shown such a combination toprovide improved analgesia with an opioid sparing effect, thus reducing the incidence of opioid related side effects.
ACUTE PAIN SERVICE (APS)
The recognition of the importance of good acute pain management has prompted the development of teams specialised at managing acute pain. The first service to be led by an anaesthesiology department was described in Seattle in 1986. These teams can be multidisciplinary and may include doctors, nurses, pharmacists, physiotherapists, and occupational therapists. Whilst many hospitals would say they have an APS, these vary from nurse-led, to anaesthetist led, to comprehensive teams providing 24-hour cover. As yet, no consensus exists as to the best model.
APS teams take on both clinical and organisational duties. They provide education to both staff and patients, undertake research and audit, and of course, deliver a range of pain management techniques. Such services have been shown to reduce pain scores and improve management of post-operative pain.
SUMMARY
Despite increased awareness of the importance of providing effective management of acute pain, there is still a significant deficit in its provision. Acute pain is not only unpleasant to experience, but may also have short and long term psychological and physiological consequences. Proper management should result in good analgesia and patient satisfaction. Early recognition and thorough assessment can provide the patient and clinician with sufficient information so that they may tailor an appropriate analgesic regimen and achieve this goal.
REFERENCES
- Macintyre, P. E. & Schug, S. A. 2007. Acute pain management : a practical guide, Edinburgh ; New York, Elsevier Saunders.
- Macintyre PE, Schug S., Scott D.A., VIsser E.J., Walker S.M. 2010. Acute Pain Management: Scientific Evidence (3rd edition). Working Group of the Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine.
- Mowat I, Hughes E, Schug S. 2014. The Management of Acute Pain. In: Armati P ed. PAIN The person; The Science; The Clinical Interface. IP Communications. Ch. 4
- Wu, C. L. & Raja, S. N. 2011. Treatment of acute postoperative pain. The Lancet, 377, 2215-2225.
MCQ Answers
- T,F,F,T,F
- F,T,T,F,F
- F,T,F,T,F



