Obstetrics Anaesthesia
KEY POINTS
- Vaginal birth after caesarean delivery may be considered for women with a singleton pregnancy and cephalic presentation with no contraindications to vaginal delivery.
- Benefits of vaginal birth after caesarean delivery compared with repeat caesarean delivery include shorter postpartum recovery and length of hospital stay, less postpartum pain, avoidance of surgical complications and reduced impact on subsequent pregnancies.
- Neuraxial labour analgesia is safe and efficacious for women aiming for a vaginal birth after caesarean delivery.
- The major risk of vaginal birth after caesarean delivery is uterine rupture, which may result in massive obstetric haemorrhage and potentially an emergency hysterectomy.
- Cardinal features of uterine rupture include abnormal fetal heart rate, severe abdominal pain that persists between contractions (despite effective neuraxial labour analgesia), vaginal bleeding, cardiovascular instability and loss of fetal station.
- Management of uterine rupture includes early recognition, immediate transfer to an operating room for emergent delivery and maternal and neonatal resuscitation.
INTRODUCTION
Women with a history of caesarean delivery (CD) with a low transverse uterine incision may be offered a repeat CD or a trial of
labour after caesarean (TOLAC) with the aim of vaginal birth after caesarean (VBAC). VBAC has risks and benefits that require
careful consideration. VBAC, compared with a repeat CD, is associated with less postpartum pain, faster return to normal function
and lower risk of certain obstetric complications in subsequent pregnancies (eg, abnormal placentation). An important risk of
TOLAC is uterine rupture (approximately 0.5% incidence after 1 CD), which can lead to significant maternal and neonatal morbidity and mortality.1,2 Although the rate of successful VBAC varies slightly between women who have had 1 CD (72%-75%) compared with 2 CDs (62%-75%), the incidence of maternal complications such as uterine rupture increases with the number of prior CDs.1,2 Women undergoing TOLAC require care within an appropriately staffed obstetric unit that is resourced to provide specialist maternal and neonatal care, including facilities for emergent CD, blood transfusion and neonatal resuscitation.
The aim of this tutorial is to outline the risks and benefits of VBAC versus elective repeat CD, highlight factors that favour
successful VBAC, provide recommendations on intrapartum anaesthetic care and provide an overview of the presentation and
anaesthetic management of uterine rupture.
CAESAREAN DELIVERY RATES AND OPTIONS FOR CHILDBIRTH
The rate of birth by CD continues to increase globally. Rates of CD vary within and between countries, for example, 26% in the United Kingdom,3 28% in New Zealand,4 32% in the United States and 33% in Australia.5 Of 169 countries, 106 (63%) have CD rates greater than the World Health Organisation’s recommendation of 10% to 15%.3 A study of more than 90 000 Australian women with 1 prior CD who met eligibility criteria for TOLAC found that 67% of women subsequently underwent elective repeat CD, 20% had a successful VBAC, and 13% had a nonelective CD for unsuccessful TOLAC.6 VBAC and elective repeat CD have their own individual risks and benefits, but successful VBAC is associated with fewer complications.2
National guidelines (in the United States, United Kingdom, Australia and New Zealand) recommend that women with a singleton pregnancy and history of a prior uncomplicated lower uterine segment CD be offered a TOLAC.6–8 After appropriate counselling of the risks and benefits of VBAC versus elective repeat CD, the planned mode of delivery should be finalised by 36 weeks of gestation.2
FACTORS AFFECTING THE SUCCESS OF VBAC
Contraindications to VBAC1
- Factors associated with high-risk of uterine rupture:
- Previous uterine rupture
- Previous classical (vertical uterine incision) CD
Full-thickness myomectomy - More than 2 previous CDs
- Any contraindication to vaginal delivery
- Placenta praevia
- Abnormal placentation (eg, placenta accreta, increta, percreta)
- Untreated genital herpes simplex virus infection
- Untreated human immunodeficiency virus infection
Women with twin pregnancies require careful assessment and education about delivery options and close intrapartum care for TOLAC.1,2 Successful VBAC occurs in 45% to 76% of women with twin pregnancies, with the rate of uterine rupture being 0.9%.2
BENEFITS AND RISKS OF VBAC AND ELECTIVE REPEAT CAESAREAN DELIVERY
Women with a history of CD should receive antenatal counselling regarding the benefits and risks of VBAC versus elective repeat CD and should be offered a TOLAC if appropriate.
Intrapartum Recommendations
Risks of TOLAC and VBAC are greater than for vaginal delivery in women without a history of CD.1,2 Women planning VBAC should labour in a suitably resourced and staffed hospital that can provide continuous intrapartum care and continuous fetal monitoring during labour, emergent CD and neonatal resuscitation with onsite access to blood products.1,2 Women should be consented for both VBAC and CD, and large-bore (eg, 16G) intravenous (IV) access should be established at the onset of labour and a full blood count and group and antibody screen obtained.
Anaesthetic Evaluation and Management
Anaesthetic assessment of women undergoing TOLAC should include identification of risk factors that indicate a high possibility of an unsuccessful TOLAC. The anaesthetist should discuss available options for labour analgesia, including neuraxial labour analgesia, patient-controlled IV analgesia (eg, remifentanil) or nitrous oxide and establish a plan for urgent/ emergent CD. Appropriate modes of anaesthesia for intrapartum CD include spinal or combined spinal-epidural anaesthesia, conversion of epidural labour analgesia to surgical anaesthesia or general anaesthesia (GA), depending on the maternal/fetal clinical status and urgency.
The woman’s acceptance or refusal of blood products should be discussed and documented as part of the consent process. Because of the risk of unsuccessful TOLAC and requirement for urgent/emergent CD, oral intake should be restricted to clear fluids to reduce the risk of pulmonary aspiration during GA.2
Women aiming to achieve a VBAC can safely receive neuraxial labour analgesia. Neuraxial labour analgesia does not reduce the chance of a successful VBAC and does not mask symptoms and/or signs of uterine rupture.9,10 Neuraxial labour analgesia for TOLAC is supported by national guidelines2,7,8 and is associated with increased VBAC success rates (73% with neuraxial labour analgesia versus 50% without).9 In the event that urgent CD is required, an in situ epidural catheter can be dosed with a potent local anaesthetic solution (eg, lidocaine 2% with epinephrine 1:200 000 in 5-mL aliquots) to rapidly achieve the desired block height and density for surgical anaesthesia. Adequate neuraxial anaesthesia for CD decreases the need for GA and associated risks such as difficult/failed intubation, pulmonary aspiration, accidental awareness during GA and adverse neonatal effects (eg, from maternal systemic effects of GA). However, an emergent CD may necessitate GA.
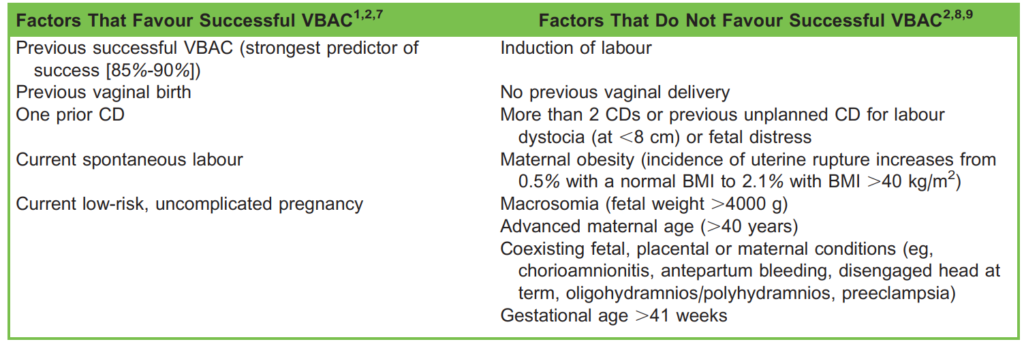
Table 1. Factors Affecting the Success of VBAC. BMI indicates body mass index; CD, caesarean delivery; VBAC, vaginal birth
after caesarean
Uterine Rupture
TOLAC and VBAC are associated with an increased risk of uterine rupture, which can lead to significant maternal and neonatal morbidity and mortality as compared with women who have no history of CD.1,2 The incidence of uterine rupture in women undergoing TOLAC ranges from 0.2% to 0.75%, as compared with <0.02% in women undergoing elective repeat CD and 0.005% to 0.2% in women with no previous CD undergoing vaginal delivery.2 Uterine rupture typically occurs at the site of the previous CD scar but can arise in other parts of the uterus and may cause bladder or urethral injury.11 Myometrial thickness in the lower uterine segment of ≥2.1 mm may be associated with a lower risk of scar rupture than myometrial thickness <2.1 mm.8 However, further prospective studies are required to investigate the utility of antepartum measurements of myometrial thickness before such measurements are used to risk stratify women considering TOLAC.1,2,11 More than 90% of cases of uterine rupture in women undergoing TOLAC occur during the intrapartum period (most commonly at a cervical dilatation of 4-5 cm), with less than 10% identified in the postpartum period.1
The increased incidence of uterine rupture highlights the importance of women to undertake TOLAC/VBAC in an appropriately resourced obstetric unit with an on-site multidisciplinary team experienced in the management of potential complications. The clinical teams should have thorough knowledge and understanding of the risk factors for uterine rupture as the diagnosis is not always obvious. Patients with scar dehiscence can be asymptomatic, and up to 10% of patients with complete uterine rupture do not exhibit the classical triad of acute-onset abdominal pain, vaginal bleeding and an abnormal fetal heart rate.1
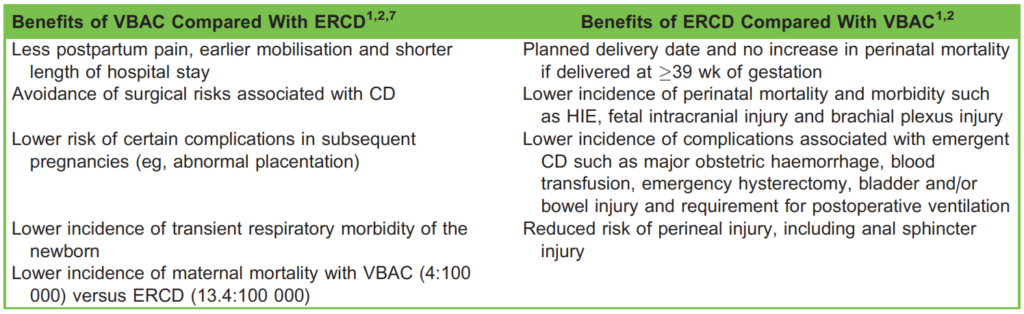
Table 2. Potential Benefits of VBAC and ERCD. ERCD indicates elective repeat caesarean delivery; HIE, hypoxic ischaemic encephalopathy; VBAC, vaginal birth after caesarean
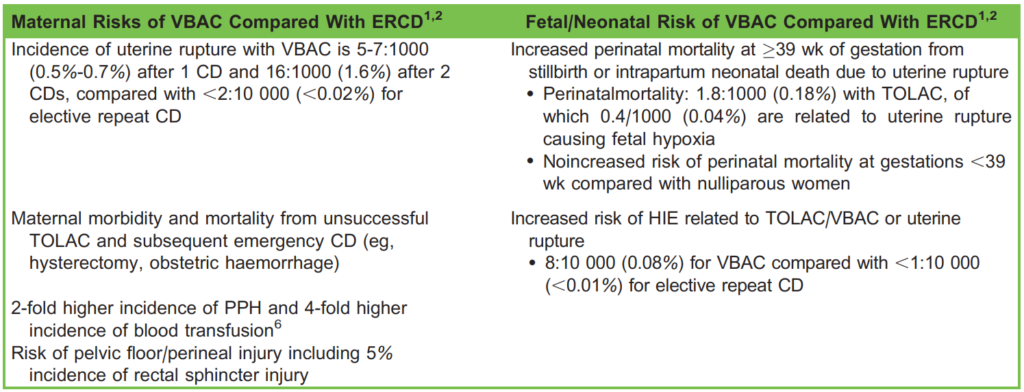
Table 3. Potential Maternal and Fetal/Neonatal Risks Associated With VBAC Compared With ERCD. CD indicates caesarean
delivery; ERCD, elective repeat caesarean delivery; HIE, hypoxic ischaemic encephalopathy; PPH, postpartum haemorrhage;
TOLAC, trial of labour after caesarean; VBAC, vaginal birth after caesarean
Risk Factors for Uterine Rupture in Women Undergoing TOLAC1,2,11
- Pharmacologic induction and/or augmentation of labour; prostaglandins and oxytocin are associated with a 2- to 3-fold increased risk of uterine rupture and a 1.5-fold greater likelihood of unsuccessful TOLAC necessitating CD
- Pregnancy interval less than 24 months: between 18 and 24 months is associated with a 2-fold increased incidence of uterine rupture and <18 months a 3-fold increased risk
- Advanced maternal age (.40 years)
- Macrosomia (>4000 g)
- Gestational age >40 weeks
- History of >1 CD
- Parity >2
Women with a history of vaginal delivery prior to or after a previous CD have a lower risk of uterine rupture when undergoing TOLAC as compared with women who have had a prior CD and no previous vaginal delivery.1,2
Symptoms and Signs of Uterine Rupture11
- Abnormal cardiotocography (present in 55%-87% of cases)2
- Severe abdominal pain–acute onset, especially if it persists between uterine contractions; scar tenderness; or escalating neuraxial labour analgesic requirements with reduced efficacy
- Vaginal bleeding; may be absent or minimal despite major intra-abdominal haemorrhage
- Loss of fetal station
- Haematuria
- Signs of cardiovascular instability (eg, hypotension, tachycardia, tachypnoea, reduced level of consciousness, cool and clammy skin) and/or raised lactate and raised anion gap metabolic acidosis
- Changes in the pattern or strength of uterine contractions
- Inability to auscultate the fetal heart at the previous transducer site
Acute-onset, severe intrapartum abdominal pain with any of the above features should prompt immediate review by an experienced obstetrician and preparation for an emergency laparotomy.
Differential Diagnosis of Acute Intrapartum Abdominal Pain
It is often difficult to distinguish between uterine rupture and other aetiologies of acute intrapartum abdominal pain. Differential diagnoses include the following12:
- Uterine rupture
- Placental abruption
- Chorioamnionitis
- Rupture of a splenic artery aneurysm
- Pregnancy-related liver disease (eg, preeclampsia with hepatic rupture)
- Ovarian cyst torsion or rupture
- Mesenteric ischaemia
- Acute appendicitis or cholecystitis
Evidence of postpartum haemorrhage despite active management of the third stage of labour should raise suspicion for uterine rupture.
Management of Uterine Rupture
Management of suspected or confirmed uterine rupture requires specialist multidisciplinary care with immediate delivery in combination with maternal and neonatal resuscitation. Early recognition and prompt transfer to an operating room for an emergency laparotomy and delivery of the fetus is fundamental to minimise the risk of neonatal hypoxic brain injury and maternal morbidity and mortality.8
Resuscitation and treatment priorities include the following13:
- Check for maternal responsiveness
- Call for help: Seek assistance from multidisciplinary specialists, and if there are signs of major haemorrhage, activate a massive transfusion protocol (or massive haemorrhage protocol, if available)
- Airway and breathing
a. Administer high-flow oxygen and ensure the patient is oxygenating and ventilating appropriately
b. If the patient is unable to effectively oxygenate or protect their airway, consider early intubation using a rapid sequence induction technique; ideally, this will occur in an operating room using appropriate induction drugs for a cardiovascularly unstable patient - Circulation
a. Ensure early left uterine displacement/lateral positioning to minimise aortocaval compression
b. Ensure IV access with 2 large-bore IV cannulae (eg, 14-16G)
c. Send blood for full blood count, venous blood gas and coagulation screen (including fibrinogen) or viscoelastic testing (eg, rotational thromboelastometry or thromboelastography), and activate the massive transfusion protocol if not already done
d. Commence fluid resuscitation in the hypovolaemic patient using a warmed crystalloid solution (eg, normal saline 0.9% or compound sodium lactate) until blood products are available
e. Administer blood products early if clinically indicated, before blood results are available
f. Administer tranexamic acid 1 g IV within 3 hours of delivery to reduce systemic hyperfibrinolysis and the risk of maternal mortality secondary to haemorrhage14; predelivery administration of tranexamic acid should be considered in women actively bleeding or at high risk of haemorrhage15 - Arrange urgent transfer of the patient to the operating room for emergency CD
- Administer GA using a rapid sequence induction technique
a. GA is indicated given the urgency and likely haemodynamic instability associated with uterine rupture, and using a preexisting labour epidural catheter may be appropriate in addition for intra-/postoperative pain management
b. Take care with induction dosing, with consideration for haemodynamic effects (consider using ketamine if cardiovascularly
unstable) - Use appropriate surgical techniques to safely deliver the fetus and achieve haemostasis, which in some cases may
necessitate emergency hysterectomy - Use an arterial line for invasive blood pressure monitoring and blood sampling (insertion of a central venous cannula for venous pressure monitoring, blood sampling and vasopressor administration may be considered but should not delay induction of anaesthesia and/or commencement of surgery)
- Avoid hypothermia (provide warm IV fluids, warm blankets and a warm operating room), avoid hypocalcaemia (administer 10% calcium chloride, 10 mL, or 10% calcium gluconate, 20-30 mL) and avoid acidosis (aggressive fluid resuscitation may be required)
- Consider using intraoperative cell salvage for autologous blood transfusion, if available
- Use point-of-care testing, including rotational thromboelastometry or thromboelastography and blood gas analysis to guide resuscitation and correction of coagulopathy
If the patient is in periarrest, an obstetric advanced life support algorithm should be used.
SUMMARY
Pregnant women with a history of CD and no contraindications to vaginal delivery may be appropriate candidates for VBAC. Given the risk of unsuccessful TOLAC and the need for emergency surgery, the anaesthetist should be made aware early of women attempting TOLAC to risk stratify and plan appropriate labour analgesia and anaesthetic management. Neuraxial labour analgesia is an effective and safe option for women undergoing a TOLAC, which may be converted to surgical anaesthesia in case of urgent CD. Uterine rupture is a major complication of TOLAC/VBAC, and the clinical team should be aware of this risk factor and its symptoms and signs. Early recognition of uterine rupture and immediate transfer to an operating room for emergent delivery (with GA) and active resuscitation are critical to minimise maternal and fetal morbidity and mortality associated with this serious event.
REFERENCES
1. Gupta JK, Birmingham GCS, Cambridge RR, et al. Birth after previous caesarean birth: green-top guideline No. 45. Royal
College of Obstetricians and Gynaecologists (RCOG); 2015. Accessed May 4, 2020. https://www.rcog.org.uk/global
assets/documents/guidelines/gtg_45.pdf
2. Leung Y, Gibson G, White S, et al. Birth after previous caesarean section. Royal Australian and New Zealand College of
Obstetricians and Gynaecologists; 2019. Accessed May 4, 2020. https://ranzcog.edu.au/RANZCOG_SITE/media/RANZ
COG-MEDIA/Women%27s%20Health/Statement%20and%20guidelines/Clinical-Obstetrics/Birth-after-previous-Caesare
an-Section-(C-Obs-38)Review-March-2019.pdf?ext¼.pdf
3. Wise J. Alarming global rise in caesarean births, figures show. BMJ. 2018;363:k4319.
4. New Zealand Ministry of Health. Report on Maternity 2017. Wellington, New Zealand: Ministry of Health; 2019. Accessed May 5, 2020. https://www.health.govt.nz/system/files/documents/publications/report-maternity-2017-may19.pdf
5. Australian Institute of Health and Welfare. Australian’s Health: Births in Australia Ch 7.14 Labour, Birth and Outcomes. Canberra, Australia: Commonwealth of Australia; 2018. Accessed May 5, 2020. https://www.aihw.gov.au/reports/aus
tralias-health/australias-health-2018-in-brief/contents/births-in-australia
6. Pont S, Austin K, Ibiebele I, et al. Blood transfusion following intended vaginal birth after cesarean vs elective repeat cesarean section in women with a prior primary cesarean: a population-based record linkage study. Acta Obstet Gynecol Scand. 2019;98(3):382-389.
7. American College of Obstetrics and Gynecology. ACOG practice bulletin No. 205 summary: vaginal birth after cesarean delivery. Obstet Gynecol. 2019;133(2):393-395.
8. Hibbard JU, Gilbert S, Landon MB, et al. Trial of labor or repeat cesarean delivery in women with morbid obesity and previous cesarean delivery. Obstet Gynecol. 2006;108(1):125-133.
9. Landon MB, Leindecker S, Spong CY, et al. The MFMU Cesarean Registry: factors affecting the success of trial of labor after previous cesarean delivery. Am J Obstet Gynecol. 2005;193(3 pt 2):1016-1023.
10. Grisaru-Granovsky S, Bas-Lando M, Drukker L, et al. Epidural analgesia at trial of labor after cesarean (TOLAC): a significant adjunct to successful vaginal birth after cesarean (VBAC). J Perinat Med. 2018;46(3):261.
11. Landon MB, Frey H. Uterine rupture: after previous cesarean delivery. UpToDate. 2020. Accessed August 12, 2020.
https://www.uptodate.com/contents/uterine-rupture-after-previous-cesarean-delivery?search¼uterine-ruptur
e&source¼search_result&selectedTitle¼1~121&usage_type¼default&display_rank¼1
12. Kilpatrick CC. Approach to acute abdominal pain in pregnant and postpartum women. UpToDate. 2020. Accessed June 4,
2020. https://www.uptodate.com/contents/approach-to-acute-abdominal-pain-in-pregnant-and-postpartum-women
13. Plaat F, Shonfeld A. Major obstetric haemorrhage. BJA Educ. 2015;15(4):190-193.
14. Shakur H, Roberts I, Fawole B, et al. Effect of early tranexamic acid administration on mortality, hysterectomy, and other
morbidities in women with post-partum haemorrhage (WOMAN): an international, randomised, double-blind, placebocontrolled trial. Lancet. 2017;389(10084):2105-2116.
15. Ahmadzia HK, Phillips JM, Katler QS, James AH. Tranexamic acid for prevention and treatment of postpartum hemorrhage: an update on management and clinical outcomes. Obstet Gynecol Surv. 2018;73(10):587-594.



