General Topics
QUESTIONS
Before continuing, try to answer the following questions. The answers can be found at the end of the article, together with an explanation.
- Which of the following can cause of cerebral palsy?
- Perinatal cerebral hypoxia, ischaemia or trauma.
- Antenatal infections, cerebral maldevelopment, genetic abnormalities.
- Postnatal central nervous system infection or trauma.
- All of the above are possible.
- All cerebral palsy patients are significantly intellectually impaired. True or False?
- What is the commonest clinical type of cerebral palsy?
- Dyskinetic
- Spastic
- Mixed
- Ataxic
- Which is not commonly associated with cerebral palsy?
- Malnutrition, impaired immune system
- Epilepsy
- Suxamethonium apnoea
- Sensory deficits and communication disorders
INTRODUCTION
Cerebral palsy (CP) is a group of non-progressive disorders of motion and posture. It results from injury to the developing brain during the antenatal, perinatal or postnatal period. Clinical manifestations are related to the area of central nervous system (CNS) affected. The clinical picture may vary considerably, from high functioning mild monoplegia with normal intellect to severe spastic quadriplegia with mental retardation.
Perioperative challenges include: seizure control, optimization of respiratory function, gastro-oesophageal reflux, management of pain, muscle spasm, nausea/vomiting and effective communication by close involvement of carers. Where possible a multidisciplinary team should be involved including the surgeon, paediatrician, anaesthetist, acute pain service, specialised nurses, physiotherapist and speech pathologist. Understanding the disease aetiology, clinical manifestations and management will help improve perioperative care of patients with Cerebral Palsy.
AETIOLOGY
In the developed world the prevalence of CP is relatively stable at 1-2.5 per 1000 live births, despite improvements in antenatal and perinatal care. Aetiology of CP is multifactorial and results from injury to the developing brain. The contribution of specific causes is still debated, and causation in individual cases is usually difficult to establish.
Recognised risk factors for developing CP include: perinatal hypoxia, prenatal infection, congenital abnormalities, trauma, and genetic predisposition. CP is likely the final common endpoint from a number of factors affecting early cerebral development, rather than any one specific event. In premature infants, CP is commonly a result of periventricular haemorrhages. For infants born after 34 weeks gestation approximately 50% of spastic quadriplegia CP is caused by prenatal problems including brain maldevelopment, stroke, infections (toxoplasmosis, rubella, cytomegalovirus, herpes virus i.e. TORCH) or genetic disorders. Intrapartum hypoxia (birth asphyxia) for term infants is now believed to cause only 6% of CP. This is less common than previously thought. Postnatal causes include meningitis, viral encephalitis, hydrocephalus, trauma, surgical lesions and their treatment.
CLASSIFICATION
CP encompasses a variety of neurological syndromes and is commonly classified by characteristics of neurological dysfunction (spastic, dyskinetic, ataxic, and mixed) and extremity involved (quadriplegia, hemiplegia, diplegia, and monoplegia).
Swedish Classification for CP (complex cases may defy classification)
- Spastic – 70% (most common clinical manifestation)
- Quadriplegia 27% of all cases of CP
- Diplegia 21%
- Hemiplegia 21%
- Dyskinetic – 10% (often normal intellect but difficulties with communication)
- Dystonia (maintained twisting position of torso and extremities)
- Athetosis (slow, purposeless, distal movements)
- Chorea (quick, jerky, proximal)
- Ataxic – 10%
- Intention tremor and head tremor (titubation)
- Mixed – 10%
- e.g. spastic athetoid
COMMON SURGICAL PROCEDURES
- 60% Orthopaedic procedures: major multilevel surgery involving tenotomies/osteotomies, soft tissue release/tendon transfers, and botulinum toxin injections.
- 10% Dental extractions and restorations.
- 10% Gastrostomy and anti-reflux procedures.
- 10% Imaging.
- 10% Other: neurosurgery, urology, ophthalmology, ENT and insertion of infusion devices.
CLINICAL PROBLEMS AND COMORBIDITIES
Central nervous system
Epilepsy affects approximately 30% of CP patients, and is most common in spastic hemiplegia. Tonic- clonic and complex-partial seizures are common. Normal anticonvulsants should be continued throughout the perioperative period. Understanding anticonvulsant side effects and drug interactions is important.
Visual and hearing deficits, behavioral disorders, communication problems and intellectual impairment are all common. However up to 60% of hemiplegic patients have normal intelligence. It is important to approach CP patients with sensitivity and to allow time for effective communication with patients and their carers. Communication aids may be required such as sign cards or computer techniques.
Attention deficit hyperactivity disorder (ADHD) is common in the higher functioning child. Depression and emotional lability are common in adolescents. These patients should be handled with care as communication difficulties may mask normal intellect.
Cardiovascular
Vascular access may be made difficult by multiple previous cannulations, scars, contractures of upper limbs, communication problems or behavioral issues. Chronic lung disease may lead to pulmonary hypertension, right ventricular hypertrophy or cardiac failure.
Respiratory
Respiratory disorders are ultimately a common cause of death. Problems include pulmonary aspiration, recurrent respiratory infections and chronic lung disease, poor cough with retention of secretions, poor nutritional state and impaired immunity. Scoliosis with restrictive lung defect may lead to cardiopulmonary compromise. Pre-operative physiotherapy, bronchodilators or antibiotics may be required.
The airway should be assessed for potential difficult laryngoscopy due to poor dentition, TMJ dysfunction and positioning problems. Formal airway assessment may be impractical and review of previous anaesthetic charts may be helpful.
Gastrointestinal
Gastro-oesophageal reflux is common due to oesophageal dysmotility and spasm, abnormal lower oesophageal sphincter function and spinal deformity. Reflux is difficult to detect and night wakening may be the only indicator. Salivary drooling due to pseudobulbar palsy may occur with impaired swallowing. Tongue thrusting and poor head movements further contribute to difficult airway management.
Poor oral feeding may lead to dehydration, malnutrition, failure to thrive, electrolyte imbalance and anaemia. Preoperative nasogastric feeding or gastrostomy may be required.
Allergies
Latex allergy has been reported in CP patients, probably due to repeated exposure during multiple operative procedures. A history of such sensitivity must be noted and taken seriously.
Medications
Medical therapy for controlling seizures, spasticity, reflux, constipation and depression should be well understood, in particular with respect to side effects and potential interactions.
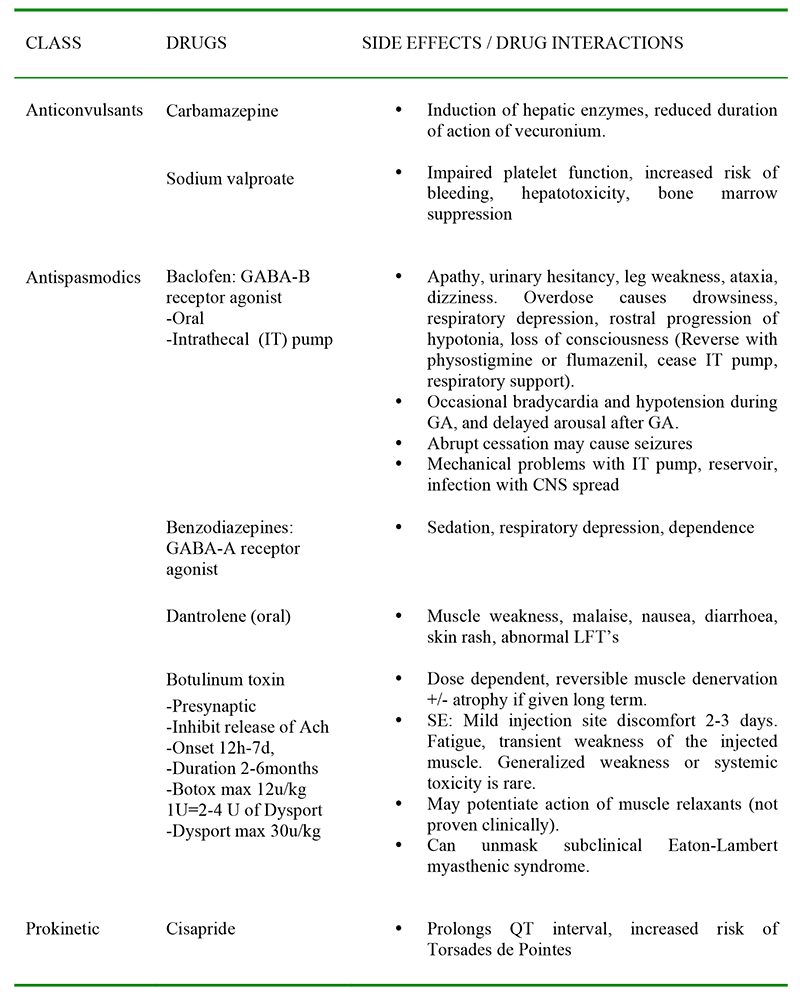
Table 1: Common medications encountered in patients with CP
PERIOPERATIVE MANAGEMENT
Pre operative
Patient anxiety is common and may be exacerbated by poor understanding and communicationdifficulty. It can be useful having the primary carer with the patient at induction, in recovery and during the postoperative period. Parental anxiety and even aggression may be manifestations of previous experiences, stress, frustration, guilt and anger. Respect and good communication is vital in gaining cooperation as well as allaying patient concerns and fears. Consent for any procedure needs to be clearly informed with risks and benefits discussed with the parent or guardian.
Benefits of sedative premedication should be balanced against side effects and potential unpredictable drug responses. Antacids and drying agents may be appropriate. Anticholinergics may be beneficial by drying oral secretions but may increase the risk of chest infection by thickening lung secretions. Local anaesthetic cream should be used at the venepuncture site to reduce pain and distress. Antireflux medication should be continued.
Intra operative
Monitoring should be according to the national safety standard. Temperature monitoring is particularly useful as CP patients are vulnerable to hypothermia, particularly in long procedures. Monitoring depth of anaesthesia may be beneficial as the MAC value is variably decreased. Neuromuscular monitoring is useful as CP patients have altered responses to muscle relaxants.
Vascular access may be difficult and use of ultrasound may not be possible in the uncooperative child. A second anaesthetist is often helpful to help establish IV access. Dehydration from abnormal cognitive responses to thirst and prolonged fasting should be assessed and managed appropriately.
Endotracheal tube size should be selected based on age, with consideration that most children with CP are small for their age. Airway maintenance may be complicated by excessive secretions and reflux. Suction of the oro- or naso-pharynx may help clear excessive secretions. The benefits of rapid sequence induction (RSI) versus gas induction in an uncooperative child must be balanced.
Positioning may be difficult due to fixed contractures, and must be done with extreme care to avoid nerve damage, muscle damage and pressure ulcers. Meticulous care is required in prevention of pressure ulcers, especially in patients receiving epidural analgesia, prolonged immobilization, and in malnourished children.
Temperature regulation is an important issue in CP children. Hypothermia is common due to disordered temperature regulation from hypothalamic dysfunction, lack of insulating muscle and fat and malnourishment. Normothermia may be difficult to achieve despite use of forced air warmers, warmed intravenous fluids and warmed irrigating fluids. Warm humidified gases are beneficial.
Drug responses are altered. For volatile agents, minimum alveolar concentration (MAC) is reduced compared to normal controls. MAC of halothane has been shown to be 20% lower in children with CP and a further 10% lower in those currently taking anticonvulsants. There is resistance to non- depolarising muscle relaxants, perhaps due to a combination of drug interaction with anticonvulsants (increased hepatic clearance, acetylcholine receptor up regulation) and chronic immobilization. There is a slight sensitivity to suxamethonium but clinical significance is not determined. Neuromuscular monitoring (with train of four) in a severely affected limb may underestimate the extent of neuromuscular block. Avoid epileptogenic agents such as enflurane, etomidate, methohexitone, ketamine, and pethidine (norpethidine accumulates in renal failure). Tramadol lowers seizure threshold and is therefore best avoided.
Regional techniques are strongly recommended for intra- and post-operative analgesia in most major procedures. Epidural analgesia is excellent for extensive lower limb surgery, but requires an experienced operator as scoliosis and prior back surgery may make insertion challenging. Any regional infusion must be carefully monitored by an experienced acute pain team and specialised nursing staff.
Post operative
Emergence problems are common. Delayed emergence may be due to hypothermia or residual volatile agent (reduced MAC and possibly MAC awake). Excessive secretion, regurgitation and vomiting, especially in children with pseudobulbar palsy, can complicate airway maintenance. Careful protection of the airway and frequent suctioning is therefore required. Irritability on emergence is common. Presence of parents or primary carer may help to comfort the patient.
Postoperative nausea and vomiting is very common, and anti-emetics should be considered particularly if opioids are used.
Pain assessment can be difficult in the CP patient due to intellectual disability or poor verbal communication skills. Behavioral indicators such as face grimacing, groaning, moaning or altered sleep patterns may be present in the non-pain state and can be inconsistent and difficult to interpret. Behavioural indicators are diverse and lack sensitivity. The primary carer usually understands the child’s personality and is an invaluable resource when assessing the child postoperatively. Surgical pain must be differentiated from benign causes such as hunger, anxiety, and positioning discomfort.
Epidural blockade is beneficial for those undergoing extensive lower limb orthopaedic surgery as it can effectively treat pain and reduce spasm. Intrathecal opioid administration is better than systemic opioids alone for correction of scoliosis, as it decreases intraoperative remifentanil requirement and improves post operative analgesia. A multimodal approach should be used including local anaesthetic techniques, paracetamol, and anti-inflammatory drugs. Systemic opioids may be given by patient controlled analgesia (PCA) or nurse initiated analgesia (NIA). PCA may be used by high functioning patients. Modification of the press button mechanism is often required. Any continuous regional or intravenous analgesic infusions should be managed in appropriate high dependency unit.
SPECIFIC PROBLEMS
Regular oral anticonvulsants should be continued. Patients may require intravenous anticonvulsant cover if over 24 hours without oral intake is expected, particularly in children with a history of generalised convulsions.
Severe muscle spasms are frequent after lower limb orthopaedic surgery. This is caused by spinal reflexes initiated by pain. Baclofen should be continued, as acute withdrawal may lead to seizures and hallucinations. Diazepam (oral, IV or rectal) may be given with appropriate ward monitoring until regular oral medication can be recommenced. Beware of excessive sedation and respiratory depression when benzodiazepines are used in combination with opioids.
Diagnosis of compartment syndrome maybe delayed by regional analgesics and impaired communication. Splitting plaster casts and leg elevation reduces this risk. Vigilant observation is required. Fixed contractures, prolonged pressure over bony prominences and malnutrition may lead to troublesome skin breakdown. Meticulous pressure care and frequent repositioning is required to prevent pressure sores.
Chronic pain requires a multidisciplinary approach particularly useful in adolescent CP patients with normal intelligence that may suffer from depression. Differentiation of surgical pain from other causes of pain is important. Hip subluxation causing pain on transfer; reflux causing night waking; back pain from prolonged sitting; period pain associated with menstruation; and painful spasticity all require different modes of therapy.
Perioperative chest physiotherapy will help those with poor cough, poor secretion clearance, and recurrent chest infections. Patients with poor respiratory function may need postoperative ventilation and even tracheostomy during the weaning process. Preoperative respiratory function tests are unreliable and not predictive of outcome.
Cerebral Palsy children are prone to constipation because of reduced gut motility and fluid intake, and this is worsened by perioperative opioids. Use opioid sparing analgesia where possible and consider normal bowel habits for that child. The prescription of laxatives may be necessary.
KEY POINTS
- Cerebral Palsy is a spectrum of non-progressive disorders of motion and posture resulting from injury to the developing brain during the antenatal, perinatal or postnatal period.
- Understanding of the clinical problems associated with different types of Cerebral Palsy and their drug therapy will allow us to improve perioperative care of these patients.
- Communication problems and sensory deficits may mask normal intellect. Close involvement of the parent or carer is essential.
- Preoperatively: optimise respiratory function, seizure control, gastro-oesophageal reflux disease and nutrition.
- Intraoperatively: prevent aspiration, hypothermia, pressure ulcers, nausea/vomiting, muscle spasm and pain.
- Postoperatively: appropriate pain assessment and management together with prevention of muscle spasms, contractures, chest infections, pressure sores, constipation and malnutrition. Maximise function, mobility and communication.
ANSWERS TO QUESTIONS
- D. All of the above are possible. CP results from injury to the developing brain during the antenatal, perinatal or postnatal period.
- False. Visual & hearing deficits, intellectual impairment, behavioral and communication problems are all common, but up to 60% of hemiplegic patients have normal intelligence.
- B. Spastic type accounts for approximately 70% CP patients.
- C. Suxamethonium apnoea is not commonly associated with cerebral palsy.
WEBLINKS
REFERENCES and FURTHER READING
- Nolan J, Chalkiadis GA, Low J, Olesch CA, Brown T C K. Anaesthesia and pain management in cerebral palsy. Anaesthesia 2000; 55, 32-41.
- Wongprasartsuk P, Stevens J, Cerebral palsy and anaesthesia, Paediatric Anaesthesia 2002; 12:296-303.
- Gibson P R J, Anaesthesia for correction of Scoliosis in Children, Anaesthesia & Intensive Care 2004; 32: 548-559



