Covid-19
KEY POINTS
- Pregnant women are especially susceptible to respiratory pathogens due to the physiological changes of pregnancy as well as being more vulnerable to secondary bacterial pneumonias.
- Vertical transmission to the fetus is uncommon.
- Where possible, early epidural analgesia should be recommended to women in labour with suspected or confirmed coronavirus disease 2019, but ensure platelet count is checked due to increased risk of thrombocytopenia.
- Avoid general anaesthesia unless absolutely necessary for standard indications.
- Donning ‘airborne-precaution’ personal protective equipment should be considered for emergency cases because of the risk of failed neuraxial block and the consequent need for conversion to general anaesthesia and intubation (an aerosol-generating procedure).
Introduction
In December 2019 a pneumonia of unknown cause, subsequently identified as caused by a coronavirus and named coronavirus disease 2019 (COVID-19), was first detected in Wuhan, China. The virus causing it was named ‘severe acute respiratory syndrome coronavirus 2′, or SARS-CoV-2, as it is related to the virus that caused the ‘severe acute respiratory syndrome’ (SARS) outbreak in 2003.1 Coronaviruses are single-stranded RNA viruses which cause illnesses ranging in severity from the common cold to severe and fatal pneumonia.2
Pregnant women may be especially susceptible to respiratory pathogens because of the physiological changes in both their immune and cardiorespiratory systems making them intolerant to hypoxia. There is some evidence suggesting that the risk of critical illness may be greatest in the later stages of pregnancy.2 Parturients are also more vulnerable to secondary bacterial pneumonia in addition to the viral inflammatory process. The clinical outcomes of pregnant women during the SARS epidemic were worse than those of nonpregnant women, with higher rates of tracheal intubation, renal failure, and disseminated intravascular coagulation.3 Data from the Middle East respiratory syndrome (MERS) outbreak were also suggestive of worse outcomes. Reassuringly, early data emerging from the COVID-19 experience suggests most pregnant women with COVID-19 will experience mild disease, with a UK mortality rate of 1%. 2,4
Clinical Features
In the general population, the onset of symptoms is usually within 14 days of exposure. Symptoms range from mild to severe, and most commonly include fever and cough and less frequently dyspnoea, fatigue, headache, and anosmia. Asymptomatic infection is possible.
The UK Obstetric Surveillance System (UKOSS) study is one of the largest studies of pregnant women admitted to hospital with COVID-19 to date.2 In this cohort, 10% of women required respiratory support. The mortality for women admitted to hospital with COVID-19 was 1%, and this is consistent with the rate identified in a comprehensive systematic review.4 The UKOSS study found that in common with the nonobstetric population risk factors for pregnant women developing severe COVID-19 include the following:5
- Being of Black, Asian, or minority ethnicity
- Preexisting comorbidities (particularly cardiac or respiratory)
- Aged >35 years
- Increased body mass index
Pregnant women with COVID-19 are more likely to be delivered by caesarean section, although the UKOSS study and other case series found that most caesarean births were for indications other than maternal compromise due to SARS-CoV-2 infection.
There is emerging evidence that suggests that individuals admitted to hospital with COVID-19 are also hypercoagulable.6 This, compounded with the hypercoagulable state of pregnancy, makes parturients with COVID-19 particularly vulnerable to thromboembolism.
In addition to the impact of COVID-19 on a pregnant woman, there are concerns relating to the potential effect on fetal and neonatal outcomes. Viral pneumonia in pregnant women is associated with an increased risk of preterm birth, intrauterine growth retardation, and perinatal mortality.7 Currently available data do show that while the risk of preterm birth before 37 weeks is increased, COVID-19 is not associated with an increased risk of spontaneous labour.3 One single-centre study in the UK found an almost 4-fold increase in stillbirth rates during the course of the pandemic when compared to the period before the onset of pandemic.8 Although none of the stillbirths in the pandemic period were among women with COVID-19, surveillance studies in pregnant women report that as many as 90% of SARS-CoV-2–positive cases are asymptomatic.9,10 However the increase in stillbirths may have resulted from indirect effects such as patient reluctance to attend hospital when needed during a pandemic.
Evidence suggests that transmission of infection to neonates and infants of women with COVID-19 can occur but is uncommon.11 Outcomes for infants of women with COVID-19 are mostly reassuring. Unlike the Zika virus, there is no evidence that COVID-19 is teratogenic. Although 5 babies died in the UKOSS study, 3 deaths were unrelated to SARS-CoV-2 infection; for the 2 remaining stillbirths it was unclear whether SARS-CoV-2 contributed to the deaths.
Personal Protective Equipment
The choice of personal protective equipment (PPE) when managing COVID-19 suspected or positive patients will depend on the mode of transmission risk.12 SARS-CoV-2, the virus that causes COVID-19, is primarily transmitted through respiratory droplets, or by contact with contaminated objects and surfaces. The virus subsequently replicates in the respiratory epithelium. Although SARS-CoV-2 is not believed to be an airborne virus, airborne transmission may be possible in specific circumstances or clinical settings where aerosols are generated. For aerosol-generating procedures (AGPs) airborne precautions are indicated. Deep exhalation in labour and pushing during delivery are not aerosol generating11 (Figure 1).
Principles of Management
The Royal College of Obstetricians and Gynaecologists have produced comprehensive guidance for the management of obstetric patients with COVID-19.11 The general principles of management are summarised below.
- When a woman with confirmed or suspected COVID-19 is admitted to the maternity suite, the following members of the multidisciplinary team should be informed: senior obstetrician, senior anaesthesia provider, midwife-in-charge, and senior neonatologist or paediatrician.
- Hourly maternal observations including temperature, respiratory rate, and oxygen saturations should be taken. Aim to keep oxygen saturation more than 94%, titrating oxygen therapy accordingly.
- Apply caution with intravenous fluid management. Given the association of COVID-19 with acute respiratory distress syndrome, women with moderate to severe symptoms of COVID-19 should have their fluid status carefully monitored using hourly fluid input and output recordings. Fluid boluses should be administered in volumes of 250–500 mL with reassessment before proceeding with further fluid resuscitation
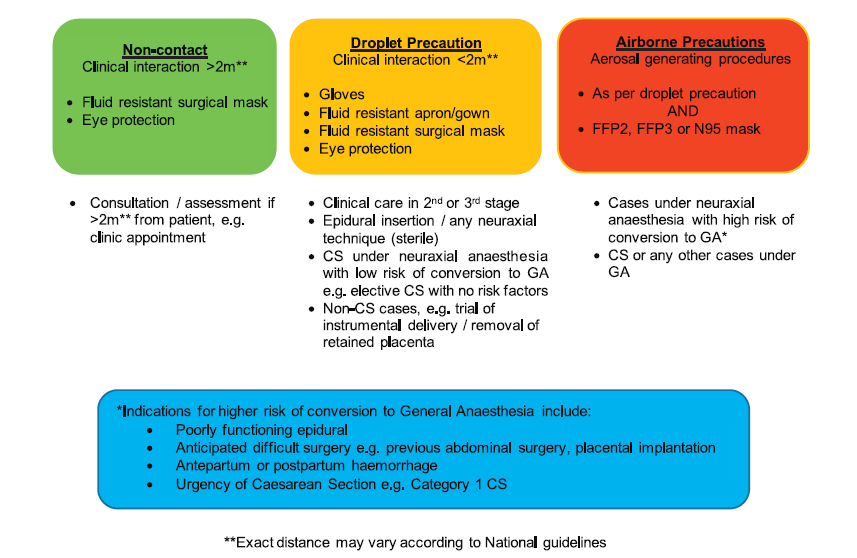
Figure 1. Personal protective equipment for obstetric anaesthesia. CS indicates caesarean section; and GA, general anaesthesia.
4. Efforts should be made to minimise the number of staff members entering the patient’s room or having contact with the patient, and units should develop local plans regarding essential personnel for emergency scenarios.
5. Continuous cardiotocography monitoring should be utilised for fetal monitoring.
6. COVID-19 has been associated with an increased risk of thromboembolic events. The following procedures should be followed for all pregnant women admitted with COVID-19 infection (or suspected COVID-19 infection):
- Women should receive prophylactic low-molecular-weight heparin unless birth is expected within 12 hours. The likelihood of neuraxial analgesia or anaesthesia, delivery, or complications should be considered when making this decision and an individual risk-benefit assessment performed.
- All pregnant women who have been hospitalised and have had confirmed COVID-19 should receive thromboprophylaxis for 10 days following hospital discharge. For women with persistent morbidity, consider a longer duration of thromboprophylaxis.
- If women are admitted with confirmed or suspected COVID-19 within 6 weeks postpartum, they should receive thromboprophylaxis for the period of their admission and at least 10 days post discharge. Consider extending this until 6 weeks postpartum for women with significant ongoing morbidity.
7. Pregnant and postnatal women already have an increased risk of anxiety and postnatal depression. A diagnosis or label of suspected COVID-19 may not be conducive to maternal or fetal well-being, potentially worsening mental health symptoms. Women may also feel more isolated where visitor restrictions are in place and may need additional psychological support.
Labour Analgesia
Published data to support practice recommendations for labour analgesia are limited and are based on data on viral transmission risks of SARS-CoV-2 and other similar viruses, combined with emerging, shared experience from maternity units caring for patients with COVID-19.13
Nitrous Oxide
Use of an Entonox breathing system does not constitute an AGP. Therefore, PPE for AGPs should not be required for staff caring for women with suspected or confirmed COVID-19 who wish to use nitrous oxide analgesia during labour. There is, however, a risk of viral contamination of the breathing system and the equipment circuit must contain an antiviral filter.11,13
Remifentanil
There are no data currently about the use of remifentanil patient controlled analgesia (PCA) in obstetric patients with COVID-19 infection. This should be used with caution in labour due to the risk of respiratory depression, especially in women with respiratory symptoms and avoided in women with oxygen saturations ,95% due to the risk of further desaturation.13
Neuraxial Analgesia
There is no evidence that epidural or spinal analgesia is contraindicated in the presence of coronaviruses. Epidural analgesia is recommended for standard indications to women in labour with suspected or confirmed COVID-19. Labour epidural analgesia may confer an additional benefit in women with COVID-19; the ability to rapidly convert the epidural to surgical anaesthesia in the event of operative delivery being required would potentially avoid the need for general anaesthesia, an AGP.
- Early reports suggested that COVID-19 was associated with thrombocytopenia in up to a third of patients and that the degree of the platelet decrease correlated with the severity of infection. It is good practice to check the platelet count in a patient with COVID-19 before siting an epidural or spinal.13
- As with every labour epidural, regular review to facilitate early identification of problems should be undertaken. Where epidural analgesia is inadequate and unlikely to be successfully converted to anaesthesia for operative procedures, early resite should be considered.
Anaesthesia For Caesarean Section
Considerations
1. Where possible, a dedicated COVID-19 operating room should be designated for use for COVID-19 patients and should be modified accordingly to avoid contamination of equipment and ensure the safety of staff.
2. Patients with suspected or confirmed COVID-19 should wear a fluid-resistant facemask for transfers to the operating room and recovery area.
3. Neuraxial anaesthesia is preferable for the usual indications because it reduces the need for general anaesthesia.
4. Consider strategies for the management of a failed neuraxial technique.
5. Intraoperative pain should be managed appropriately, and general anaesthesia to alleviate pain should not be denied due to the presence of COVID-19.
6. Donning PPE is mandatory and time consuming. Women and their families should be informed about potential delays.10
7. PPE impairs communication; closed-loop communication and checklists should be used whenever possible.
8. Minimise the number of clinical staff in the operating room whilst adhering to a safe level of staffing.
9. For elective surgery, patients with suspected or confirmed COVID-19 should be placed last on the daily schedule to facilitate deep cleaning.
Emergency Caesarean Section
One of the most contentious aspects for anaesthesia providers when caring for a woman with COVID-19 who requires an emergency caesarean section is the choice of PPE and specifically the choice between airborne and droplet precautions. If general anaesthesia is planned, airborne precautions are indicated, and if neuraxial anaesthesia is planned, then droplet precautions are indicated. However, the risk of intraoperative conversion from neuraxial to general anaesthesia is higher in the emergency setting and it may be appropriate to use airborne precautions even if neuraxial anaesthesia is planned.13,14
Changing from a standard surgical face mask to a FFP2/3 or N95 mask in the event of conversion to general anaesthesia could cause delay and risk contamination of the clinician.
Strategies to avoid the need for intraoperative conversion to general anaesthesia must be considered, including de novo initiation of spinal (or combined spinal-epidural) anaesthesia rather than extending poorly functioning labour epidural analgesia.
Given the additional steps involved in preparing for general anaesthesia in COVID-19 patients, and the increased risk from aerosolisation, an expeditious spinal anaesthetic may be appropriate even for category 1 caesarean section procedures. In cases of urgency, spinal anaesthesia should be performed by the most experienced anaesthesia provider to minimise the risk of repeated attempts causing delay or conversion to general anaesthesia.
General Anaesthesia
Rapid-sequence induction should be performed as standard in pregnant patients. Intubation and extubation are AGPs and airborne-precaution PPE should be worn.
1. Do not use high-flow nasal cannulae for preoxygenation or during apnoeic oxygenation.
2. Videolaryngoscopy should be first line where available, with intubation by the most experienced anaesthesia provider available. Videolaryngoscopy allows the provider to maintain a greater distance from the patient’s airway when compared to direct laryngoscopy. Do not ventilate the patient until the endotracheal tube cuff has been inflated.
3. Anticipate rapid desaturation due to impaired respiratory function.
4. Consider wearing a second pair of gloves; remove the outer pair once the endotracheal tube is secured due to respiratory secretion contamination.
5. Avoid using auscultation to confirm endotracheal tube position; utilise alternative methods, eg chest rise, end-tidal CO2.
6. Minimise the number of staff in the room during extubation as it is an AGP.
7. Consider the most appropriate postoperative location for the mother depending on clinical condition. This may require discussion with the intensive care team.
Postoperative and Postnatal Care
1. Awake patients with suspected or confirmed COVID-19 should wear a fluid-resistant facemask for transfer to the recovery location.
2. Despite initial concerns that nonsteroidal anti-inflammatory drugs (NSAIDs) worsen outcomes in patients with COVID-19 disease, there is no clinical evidence to confirm this. Current advice is that NSAIDs can continue to be used for postoperative analgesia.
3. Both clinical staff and patients alike will require additional support during this COVID-19 pandemic. Pregnant and postnatal women already have an increased risk of anxiety and depression. Women and staff should receive timely evaluation of any mental health symptoms.11
Breastfeeding
There is currently insufficient evidence regarding the safety of breastfeeding and the need for separation of mother and baby.11 Since the main concern is that the virus may be transmitted by respiratory droplets rather than breastmilk, breastfeeding mothers should ensure that they wash their hands and wear a fluid-resistant facemask before touching the baby.11 Current guidance for postnatal management of infants born to mothers with confirmed or suspected SARS-CoV-2 infection is to keep mother and infant together.
Broader Considerations For Obstetric Care During The Pandemic
While the focus of healthcare has necessarily shifted to COVID-19, this cannot come at the expense of losing existing standards in other sectors of healthcare. During the Ebola outbreak in Sierra Leone in 2016 it was demonstrated that following the onset of the epidemic, there was a decrease in the number of women attending for antenatal and postnatal care and birth at a healthcare facility, with a corresponding 34% increase in the facility-based maternal mortality ratio and a 24% increase in the stillbirth rate.15 Clinicians should work to mitigate the impact of reduced antenatal, postnatal, and high-risk clinics to ensure maternal and fetal outcomes do not suffer during the pandemic.
SUMMARY
The presence of COVID-19 presents challenges to the anaesthesia provider and wider team and the potential to encounter pregnant patients with suspected of confirmed COVID-19 within maternity facilities should be considered, with steps taken to prepare for their management. Units should develop plans for common procedures and scenarios.
References
1. Gorbalenya AE, Baker SC, Baric RS, et al. Severe acute respiratory syndrome-related coronavirus: the species and its viruses—a statement of the Coronavirus Study Group. bioRxiv 2020; doi: 10.1101/2020.02.07.937862
2. Wong SF, Chow KM, Leung TN, et al. Pregnancy and perinatal outcomes of women with severe acute respiratory
syndrome. Am J Obstet Gynecol. 2004;191:292-297.
3. Knight M, Bunch K, Vousden N, et al. Characteristics and outcomes of pregnant women admitted to hospital with
confirmed SARS-CoV-2 infection in UK: national population based cohort study. BMJ. 2020;369:m2107. doi:10.1136/bmj.m2107
4. Khalil A, Kalafat E, Benlioglu C, et al. SARS-CoV-2 infection in pregnancy: a systematic review and meta-analysis of
clinical features and pregnancy outcomes. EClinicalMedicine. 2020; doi: 10.1016/j.eclinm.2020.100446
5. Williamson EJ, Walker AJ, Bhaskaran K, et al. OpenSAFELY: factors associated with COVID-19 death in 17 million
patients. Nature. 2020; doi: 10.1038/s41586-020-2521-4
6. Bikdeli B, Madhavan MV, Jimenez D, et al. COVID-19 and thrombotic or thromboembolic disease: implications for
prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol. 2020;75(23):2950-2973.
7. Goodnight WH, Soper DE. Pneumonia in pregnancy. Crit Care Med. 2005;33(suppl 10):S390-S397. doi:10.1097/01.ccm.0000182483.24836.66
8. Khalil A, von Dadelszen P, Draycott T. Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA. 2020; doi:10.1001/jama.2020.12746
9. Campbell KH, Tornatore JM, Lawrence KE, et al. Prevalence of SARS-CoV-2 among patients admitted for childbirth in southern Connecticut. JAMA. 2020;323(24):2520-2522.
10. Sutton D, Fuchs K, D’Alton M, et al. Universal screening for SARS-CoV-2 in women admitted for delivery. N Engl J Med. 2020;382(22):2163-2164.
11. Royal College of Obstetricians and Gynaecologists. Coronavirus (COVID-19) infection in pregnancy. Version 10.1. RCOG 2020. https://www.rcog.org.uk/coronavirus-pregnancy. Accessed July 10, 2020.
12. Cook TM. Personal protective equipment during the coronavirus disease (COVID) 2019 pandemic—a narrative review. Anaesthesia. 2020;75(7):920-927.
13. Bampoe S, Odor PM, Lucas DN. Novel coronavirus SARS-CoV-2 and COVID-19. Practice recommendations for obstetric anaesthesia: what we have learned thus far. Int J Obstet Anesth. 2020; 43:1-8.
14. Kinsella SM. A prospective audit of regional anaesthesia failure in 5080 caesarean sections. Anaesthesia.
2008;63(8):822-832.
15. Jones SA, Gopalakrishnan S, Ameh CA, et al. ‘Women and babies are dying but not of Ebola’: the effect of the Ebola virus epidemic on the availability, uptake and outcomes of maternal and newborn health services in Sierra Leone. BMJ Glob Health. 2016; 1(3):e000065.



